Fig. 36.1
LAGB with PSG. The band is placed around the upper part of the stomach to form a small gastric pouch. The fundus of the stomach is plicated to reduce gastric volume
Gastric plication can be done as a standalone procedure or in combination with LAGB. Although unproven, we believe that gastric plication in combination with LAGB is likely to provide longer weight loss durability. It can also be done below the band or all the way up the stomach with a band placed over the top of the plication. We have chosen to place a band by traditional methods and plicate below in order to capitalize upon the published durability of the band [11]. The gastric plication can be done as an anterior plication or as a greater curvature plication. Greater curvature plication has been shown to have a greater weight loss potential [5] and therefore is our preferred technique. We describe the steps used to perform a LAGB with PSG. The use of gastric plication for weight loss surgery is still considered investigational by the American Society for Metabolic and Bariatric Surgery (ASMBS) and their recommendation is that such procedures should be done with Institutional Review Board (IRB) approval [12].
36.2 Indications and Contraindications
Because LAGB with PSG is a novel technique, we recommend that the operation be done under the approval of an IRB. We believe that the procedure will be an effective operation for treating morbid obesity and its related comorbidities. The intention of the operation is to augment the weight loss seen in LAGB. Indications for the procedure would include the indications for metabolic surgery in general, body mass index (BMI) greater than 35 kg/m2 or a BMI of 30 kg/m2 with comorbidities associated with obesity including hypertension, diabetes, obstructive sleep apnea.
The benefit of this operation over other metabolic surgeries is that no bowel anastomosis or gastrointestinal resection is performed. Patients at high risk for resection line or anastomotic leaks are likely to benefit from this operative approach over LRYGB or LSG. This patient population includes those who are immunosuppressed or have inflammatory bowel disease.
Another benefit of the operation is the ability to “reverse the operation” and essentially restore the anatomy to its original configuration. The LAGB can be removed and the PSG can be reversed by removing the plication sutures. This is a benefit over LSG or LRYGB that cannot be easily reversed. LAGB with PSG is also indicated in patients with previous abdominal operations that may have reduced bowel length or significant bowel adhesions that may make LRYGB difficult or contraindicated.
We would avoid offering this operation to patients who have had a history of gastric cancer or are at increased risk for gastric cancer. After the PSG there is a significant amount of stomach that cannot be inspected by endoscopy and this could potentially lead to a delayed diagnosis for gastric cancer. These patients are likely to be better served by LSG or LRYGB with resection of the gastric remnant.
36.3 Technique
36.3.1 Step 1: Operative Set-up
The patient is placed in the supine position with both arms tucked at the patient’s side. The bed is placed in steep reverse Trendelenburg to allow for eventual exposure of the esophageal hiatus. The assistant stands on the patient’s left side while the operative surgeon is positioned on the patient’s right side.
36.3.2 Step 2: Access to the Abdomen
The procedure can be done either using a multiport laparoscopic approach or through a SILS™ port (Covidien, New Haven, CT, USA). For the multiport laparoscopic approach we place a 5-mm port just superior and to the left of the umbilicus to be used as a camera port utilizing a 5-mm 30° laparoscope. The assistant is on the left side of the patient and the assistant port is placed along the left anterior axillary line in the subcostal region, 5-mm port. The working ports are a 15-mm port in the midclavicular line half-way between the subcostal margin and the umbilicus. This port is eventually used to introduce the adjustable gastric band. And a 5-mm port in the right anterior axillary line in the subcostal space serves as the second working port (Fig. 36.2). A Nathanson liver retractor is placed in the subxiphoid space to retract the left lobe of the liver.
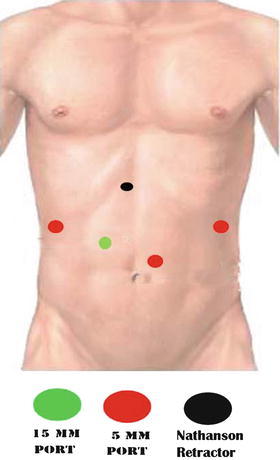
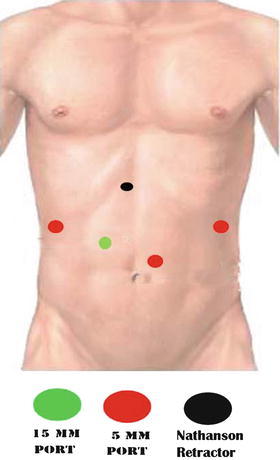
Fig. 36.2
Multiport placement for LAGB. A Nathanson retractor can be used in cases where the left lobe of the liver obscures the proximal stomach
To perform the procedure through a single incision we use a SILS™ port (Covidien) at the umbilicus. Through the SILS™ port (Covidien) we place three trocars. One trocar is used for a 5-mm articulating laparoscope while the other two trocars are used for the operative instruments. These trocars vary between 5-mm to 15-mm depending on the step being performed in the procedure. It is helpful to select a SILS™ port (Covidien) that allows for the upsizing and downsizing of trocars while maintaining pneumoperitoneum.
36.3.3 Step 3: Placement of the Adjustable Gastric Band (AGB)
AGBs are placed via the accepted pars flaccida technique described by O’brien and colleagues [13] with a few exceptions pointed out below. As usual the retro-gastric tunnel is created from the infero-medial base of the right crus of the diaphragm and extended to the angle of His as marked by the consistently found left inferior phrenic vein. We advocate the use of an articulating grasper to avoid potential injuries to the posterior gastric wall. The band tubing and buckle are coupled, but left unlocked (which is a deviation from the traditionally described technique) in order to facilitate passage of an endoscope. Typical gastro-gastric plication is then performed between the fundus and cardia of the stomach. The most cephalad aspect of the fundus is plicated with 2–3 interrupted, non-absorbable sutures in order to create a loose gastric tunnel (Fig. 36.3).
Fig. 36.3
The band is plicated in place by approximating the cardia of the stomach to the fundus over the band with non-absorbable sutures
36.3.4 Step 4: Gastroscopy
A standard gastroscope (29Fr equivalent) is advanced through the pyloric channel and positioned along the lesser gastric curvature. The gastroscope serves as both a calibration tube as well as a means to evaluate the gastric lumen upon completion of the greater curvature plication (Fig. 36.4). The use of a calibration tube (bougie) is not universally performed by varying surgeons (Table 36.1) for gastric plication. We find that an endoscope helps to prevent over narrowing of the gastric lumen that can lead to obstruction.
Fig. 36.4
Endoscopic evaluation of the gastric lumen after plication to confirm a uniform tubular narrowing of the lumen
Table 36.1
Variation in published techniques for plicated sleeve gastroplasty
Study (first author) | Year | Plication | Approach | Method | Patients | Bougie | Distance from pylorus (cm) |
|---|---|---|---|---|---|---|---|
Talebpour [4] | 2007 | Greater curvature | Laparoscopic | Suture | 100 | None | 3 |
Huang [8] | 2011 | Greater curvature | Laparoscopic | Suture | 1 | 38 Fr | 3 |
Ramos [14] | 2010 | Greater curvature | Laparoscopic | Suture | 42 | 32 Fr | 0 |
Brethauer [5] | 2011 | Anterior | Laparoscopic | Suture | 9 | None | 4 |
Greater curvature | 6 |
36.3.5 Step 5: Identification of the Pylorus
The pylorus is typically identified laparoscopically, but the endoscope may be employed if necessary. A point 8 cm proximal to the pylorus, along the greater curvature, is marked as the distal extent of the plication (Fig. 36.5).
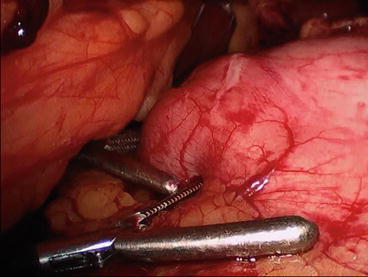




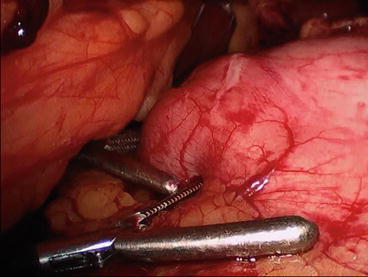
Fig. 36.5
The plication is carried distally to approximately 8 cm from the pylorus. Standard graspers are used to measure the distance from the pylorus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








