Finney and Jaboulay Techniques
Hasan T. Kirat
Feza H. Remzi
Crohn’s disease (CD) is an inflammatory condition without known cure. CD may manifest in one of the three principal patterns: obstructive, inflammatory, and perforating. Surgery is needed for at least half of patients with CD during their lifetime (1). While extensive surgical resection does not reduce recurrence of the disease, it may place the patients at risk for the development of short-bowel syndrome (2). Strictureplasty, which was adapted from pyloroplasty for the treatment of tuberculous stricture, has become a valuable choice in patients affected by diffuse obstructive CD, since it conserves the bowel (3). Some studies found no difference in the recurrence rate following strictureplasty and resection (4,5). Others showed significantly shorter reoperation-free survival for patients undergoing strictureplasty alone or strictureplasty with resection than those who underwent resection alone (6). While the most preferred strictureplasty is the Heineke-Mikulicz (H-M) for the strictures <10 cm in length (7), Finney or Jaboulay strictureplasties are most applicable to patients with longer strictures (8,9). Some studies found higher rate of recurrence following Finney or Jaboulay techniques compared to H-M strictureplasty (8,10). However, a meta-analysis of 1,825 strictureplasties showed that the proportion of patients requiring additional surgery was decreased when a Finney strictureplasty was used (7). Strictureplasty has also become the preferred technique for obstructive duodenal CD, when complications develop. This chapter describes techniques and outcomes of Finney and Jaboulay strictureplasties for small-bowel and duodenal CD.
Duodenal Strictureplasty
Although CD rarely involves the duodenum, when complications such as bleeding, perforation, or obstruction develop, surgery is needed. Bypass surgery has been abandoned after strictureplasty has become the preferred technique for obstructive duodenal CD. H-M or Finney procedures are used depending upon the length and position of the stricture. For strictureplasty, a full Kocher maneuver is used to completely mobilize the duodenum. During strictureplasty, simultaneous strictures should be assessed by passage of a deflated urinary catheter, especially at the junction of the third and fourth parts of the duodenum. Gastrostomy and vagotomy, when pyloroplasty was performed, are no longer used (11).
Worsey et al. (11) reported 13 CD patients with duodenal stricture. Two patients had postoperative complications. At a median follow-up of 3.6 years, one patient underwent reoperation for recurrence. They concluded that strictureplasty is a safe and effective operation for duodenal CD. Use of Finney-type anastomosis also has been reported for duodenal stricture in CD with good results (12). However, a study including 13 patients with strictureplasty showed that strictureplasty for duodenal CD is associated with a high incidence of postoperative complications and restructure, since nine patients required further surgery with a follow-up of 9 years (13). The difference in the duration of follow-up may explain these different results. Further studies investigating recurrence after duodenal strictureplasties with longer follow-up and greater number of patients are needed.
Worsey et al. (11) reported 13 CD patients with duodenal stricture. Two patients had postoperative complications. At a median follow-up of 3.6 years, one patient underwent reoperation for recurrence. They concluded that strictureplasty is a safe and effective operation for duodenal CD. Use of Finney-type anastomosis also has been reported for duodenal stricture in CD with good results (12). However, a study including 13 patients with strictureplasty showed that strictureplasty for duodenal CD is associated with a high incidence of postoperative complications and restructure, since nine patients required further surgery with a follow-up of 9 years (13). The difference in the duration of follow-up may explain these different results. Further studies investigating recurrence after duodenal strictureplasties with longer follow-up and greater number of patients are needed.
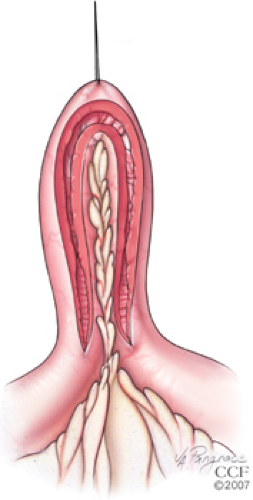
Technique for Finney Strictureplasty
Finney strictureplasty is performed for strictures between 10 and 20 cm long. It can be performed with either the stapler or hand-sewn technique. In the hand-sewn technique, first, a stay suture is placed on the mid portion of the stricture. This area is folded over onto itself, and a U-shaped enterotomy is made through the stricture using scalpel or cautery (Fig. 59.1). Another suture is placed on the normal side of the bowel to hold the U-shape in place. After the posterior edges are sutured in a continuous fashion (Fig. 59.2), anterior edges are sutured together in an interrupted fashion using long-term absorbable sutures in one layer (Fig. 59.3).