Chapter 32 Fertility Preservation in Cancer Patients
INTRODUCTION
In the modern era of aggressive treatment of malignancies, many cancer survivors will be of reproductive age and wish to resume normal lives. Consequently, fertility preservation has become an increasingly important issue. In addition to the expected difficulties with fertility, obstetrics disorders, such as early pregnancy loss, premature labor, and low birth weight, have also been described after cancer treatment.1
PATIENT POPULATION
The target population is comprised of female and male cancer patients who wish to retain future fertility. Childhood cancer is relatively uncommon, affecting only about 14 of every 100,000 children in the United States each year, and almost 80% of these children survive to adulthood. The most common childhood malignancies are acute lymphoblastic leukemia, central nervous system tumors, and lymphomas. During adolescence, the incidence of osteosarcoma also increases. In the early 20s, the risk of sarcomas and embryonic cancers increases as well.1 In adults, the leading cancers are lung, colon and rectum, and breast, the latter of which is the most common cancer in women. Gynecologic malignancies, lymphomas (including Hodgkin’s disease), melanomas, and bladder cancers are also relatively common. The mainstay of treatment of all of these malignancies remains surgery, chemotherapy, and radiation.
Premature gonadal failure is a well-known consequence of ovarian exposure to chemotherapeutic drugs. A wide variety of malignant and nonmalignant conditions during the reproductive years are treated with gonadotoxic chemotherapy. Although there are several reports of girls under age 16 who have requested preservation of fertility before cancer therapy, the most common malignancy in reproductive-age women that requires immediate fertility intervention is breast cancer.2,3 Fifteen percent of all breast cancer cases are estimated to occur in women younger than age 40.4
Premature gonadal failure is also a well-known consequence of ovarian exposure to radiation. In general, radiotherapy is used cautiously in children and adolescents because of its late sequelae on immature and developing tissues.1 Pelvic radiotherapy is most commonly used to provide local disease control for solid tumors, including tumors of the bladder, rectum, uterus, cervix, and vagina, all of which are more common in adult women. Cervical cancer is perhaps the most common malignancy in reproductive-age women desiring fertility-preserving intervention. It is estimated that 50% of the 13,000 women newly diagnosed with cervical cancer in the United States will be younger than age 35.5
CHEMOTHERAPY AND OVARIAN DAMAGE
Cytotoxic Drug Targets
The menstrual dysfunction that occurs during chemotherapy is not always due to the direct toxic effects on the ovary. Severe illness, malnutrition, and general mental and physical stress can interfere with normal function of the hypothalamic-pituitary-ovarian axis. Short-term disruption of a menstrual cycle can also be the result of destruction of growing follicles rather than primordial follicles. Destruction of all growing follicles will delay menses for at least 3 months, because it takes a primordial follicle approximately 85 days to reach the stage of ovulation.
Risk Factors for Gonadal Damage
The most important risk factors for gonadal damage are the age of the patient, the drug class, and cumulative dose of the drug. The risk of gonadal damage increases with the age of the woman. This is most likely due to the presence of fewer remaining oocytes compared to younger patients. In one study of women who had received mechlorethamine, Oncovin (vincristine), procarbazine, and prednisone (MOPP protocol) for Hodgkin’s disease, the subsequent amenorrhea rate was 20% for women younger than age 25, compared to 45% for those at least 25 years old.6 In another study, the overall incidence of premature ovarian failure after MOPP chemotherapy was 61%.7
Cytotoxic chemotherapeutic agents are not equally gonadotoxic. Cell-cycle nonspecific chemotherapeutic agents are considered to be more gonadotoxic than cell-cycle specific ones (Table 32-1). Alkylating agents are among the most gonadotoxic of these cell-cycle nonspecific drugs, and women who have received high-dose alkylating agent therapy are at highest risk for premature ovarian failure. Cyclophosphamide is considered to be the most gonadotoxic member of this category.
Table 32-1 Gonadotoxic Chemotherapeutic Agents*
* Female gonads; male gonads may have different sensitivity. Many drugs have unknown risks.
Predicting Ovarian Failure
Premature ovarian failure does not consistently occur in patients receiving multiagent chemotherapy, regardless of age or type of chemotherapeutic agent. Most young patients with Hodgkin’s disease treated with multiagent chemotherapy and radiation to a field that does not include the ovaries will be fertile, although their fertility will begin to decrease at a younger age than matched controls.8 A spontaneous conception was reported in a young woman with premature ovarian failure after 14 courses of an alkylating agent combined with pelvic irradiation for treatment of Ewing’s sarcoma of the pelvis.9 This exemplifies the difficulties in predicting the probability of ovarian failure after chemotherapy, which also makes it difficult to evaluate the efficacy of treatment aimed at preserving ovarian function.
Markers for Gonadal Damage
Serum Markers
Cancer chemotherapy is associated with a transient suppression of inhibin B in prepubertal girls. Consequently, inhibin B levels, together with sensitive measurements of FSH, are potential markers of the gonadotoxic effects of cancer chemotherapy in prepubertal girls.10
Ultrasonographic Markers
Another method to assess ovarian reserve in these patients is ultrasonographic determination of ovarian volume and antral follicle count.11 Cancer survivors with normal ovarian function tend to have normal antral follicle counts, although their ovarian volumes are often smaller than controls.
RADIOTHERAPY AND DAMAGE TO PELVIC ORGANS
Pelvic radiotherapy damages both the ovaries and the uterus. Ovarian damage from radiotherapy results in impaired fertility and premature ovarian failure.11–19 Radiation therapy–induced uterine damage manifests as impaired growth and blood flow.20 The effects on subsequent pregnancies can be substantial.
Ovarian Damage
The ovarian follicles are remarkably vulnerable to DNA damage from ionizing radiation. Radiation therapy results in ovarian atrophy and reduced follicle stores.18 As a result, serum FSH and luteinizing hormone (LH) levels progressively rise and estradiol levels decline within 4 to 8 weeks after radiation exposure.
However, a recent study suggested the presence of germline stem cells in the adult ovary.19 If these findings are confirmed by others, they leave open the possibility that new oocytes might be able to be regenerated after depletion by chemotherapy or radiotherapy.
Risk Factors for Ovarian Damage
Cancer patients are at high risk for premature ovarian failure after treatment with pelvic or total body radiation. The degree of ovarian damage is related to the patient’s age and the total dose of radiation to the ovaries (Table 32-2). For example it may take 12 Gray (Gy; 1 rad = 1 cGy) to induce permanent ovarian failure in prepubertal girls and only 2 Gray to achieve the same result in women older than age 45.12 It is generally estimated that a single dose of 6.5 to 8.0 Gy will cause permanent ovarian failure in most postpubertal women.13
Table 32-2 Determinants of Radiation-induced Gonadal Failure
| Age of patient |
| Concomitant chemotherapy |
A dose-dependent reduction in the primordial follicle pool occurs when exposing ovaries to radiotherapy. It is estimated that as little as 3 Gy is enough to destroy 50% of the oocyte population in young reproductive-age women.14
The dose-response of the ovaries to irradiation has been demonstrated in several studies.15–17 When the mean radiation dose to the ovary was 1.2 Gy, 90% of patients retained their ovarian function. When the mean dose was 5.2 Gy, only 60% retained ovarian function. Ovarian failure will occur in virtually all patients exposed to pelvic radiation at doses necessary to treat cervical cancer (85 Gy) or rectal cancer (45 Gy) or to total body radiation for bone marrow transplantation (8 to 12 Gy to the ovaries). The addition of chemotherapy to radiotherapy further decreases the dose required to induce premature ovarian failure.
Uterine Damage
Pregnancy after Radiation Therapy
Pregnancies achieved by survivors of childhood cancer who have received pelvic irradiation must be considered high risk due to the uterine factor.20,21 Common obstetric problems reported in these patients include early pregnancy loss, premature labor, and low birthweight infants.
FERTILITY PRESERVATION STRATEGIES
Pharmacologic Protection
Gonadotropin-releasing Hormone (GnRH) Agonists
One of the first strategies attempted was to mimic the premenarchal state by administering GnRH agonists.22,23 This was based on the observation that ovaries of premenarchal girls are less sensitive to cytotoxic drugs than adult ovaries. The hypothesis is that suppressing FSH and LH elevation will inhibit the normal physiologic loss of primordial follicles by recruitment and subsequent atresia. Other possibilities include a protective effect of decreased ovarian perfusion secondary to the resultant hypoestrogenic milieu or a direct gonadal effect mediated through sphingosine-1-phosphate or germline stem cell preservation.24
The most compelling study of this approach to date was performed in primates. A prospective, randomized, controlled trial using rhesus monkeys demonstrated that administration of GnRH agonists protected the ovary against cyclophosphamide-induced damage.25
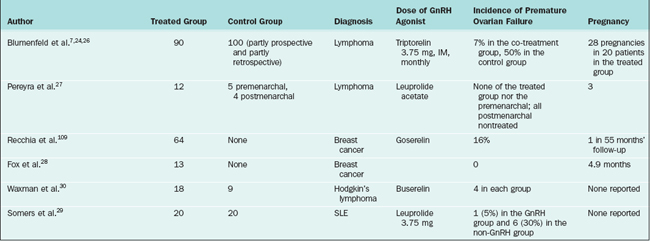
Several human studies have also shown promising results (Table 32-3). In the largest study, 90 lymphoma patients treated with chemotherapy and GnRH agonists had a premature ovarian failure rate of 7% compared to a 30% rate for patients treated with chemotherapy alone.7 Similar results were reported by others.26–29 One small prospective, controlled study of 18 women showed that GnRH agonists were not effective in the prevention of premature ovarian failure.30
Some investigators have questioned the theoretical value of GnRH agonist gonadal suppression in preserving ovarian function in susceptible patients.31,32 Research has shown that primordial follicles initiate follicle growth through an unknown mechanism, which is gonadotropin independent.33 GnRH-1 receptor is expressed on the human ovary, but its physiologic or pharmacologic role is unclear. However, 80% of human ovarian cancers express GnRH receptor and both GnRH agonists and antagonists inhibit the proliferation of cancer cell lines.34
Another important fact is that although mRNA expression for FSH receptors has been identified in human primordial follicles, there is no report of identification of the FSH receptor protein in these follicles.35 FSH receptor protein is uniformly present in as early as 3–4 granulosa layer preantral follicles.31 Consequently, it is possible that GnRH analogues preserve only follicles that have initiated growth, which constitute less than 10% of all the follicular pool at any given time in the ovary. Once follicle growth has been initiated, each follicle is destined either to undergo atresia or to ovulate. It is quite possible that GnRH agonist cotreatment delays the fate of these follicles, hence giving the impression that ovarian function is protected in the short run.
A final observation that suggests that GnRH therapy might not work is that prepubertal children receiving heavy chemotherapy still suffer from ovarian failure.36 Meirow proposed that because younger patients have a larger ovarian reserve, absence of immediate ovarian failure does not mean that gonads are unaffected by the chemotherapy37 but simply that the patient has a sufficient number of oocytes not to demonstrate immediate failure. Given the above-mentioned arguments and counterarguments, a prospective, randomized study with sufficient power will appropriately evaluate the effectivness of GnRH analogues as a potential strategy for fertility preservation.
Oral Contraceptive Pill and Progestins
Unfortunately, suppressive therapy with a variety of oral steroids such as oral contraceptives or progestins has not been shown to be effective in preventing damage from chemotherapy or radiation therapy.38–41
Apoptotic Inhibitors: A New Research Direction
Inhibition of apoptosis signaling events could potentially stop the apoptotic process and protect the patient from premature ovarian failure. Apoptosis plays an essential role in germ cell dynamics, both prenatally and postnatally.42,43 Moreover, apoptosis could be activated aberrantly via chemotherapeutic drugs.44,45
Sphingosine-1-phosphate may be an example of an apoptotic inhibitor. Ceramide is a sphingolipid molecule believed to be an early messenger signaling apoptosis in response to stress. It was shown that oocytes of mice that lacked the enzyme to generate ceramide, acid sphingomyelinase, and wild type mice oocytes that had been treated with sphingosine-1-phosphate therapy resisted apoptosis induced by doxorubicin.46
OVARIAN TRANSPOSITION
Transposing the ovaries out of the field of irradiation appears to help to maintain ovarian function in patients scheduled to undergo gonadotoxic radiotherapy. Transposing the ovaries reduced the radiation dose to each ovary compared to ovaries left in their original location.47 Transposed ovaries received a dose of 126 cGy during intracavitary radiation, 135 to 90 cGy during external radiation therapy with a total dose of 4500 cGy, and 230 to 310 cGy during para-aortic node irradiation with a dose of 4500 cGy.48
Lateral versus Medial Transposition
Lateral transposition appears to be more effective than medial transposition. Initial experience with medial transposition (i.e., suturing the ovaries posterior to the uterus and shielding them during treatment) showed that this approach is generally ineffective. A compilation of 10 case reports and small series showed an ovarian failure rate of 14% after lateral transposition compared to 50% after medial transposition.49
One study compared 7 cervical cancer patients who underwent lateral ovarian transposition to 9 Hodgkin’s disease patients who underwent medial transposition, all of whom underwent radiation therapy.50 Six of the 7 patients with lateral transposition were shown to have ovaries outside the field by computed tomography (CT), and all retained ovarian function. Scattered doses to the ovaries were calculated to be 100 to 300 cGy. The 1 patient with ovaries within the field received 450 cGy and developed ovarian failure. After medial transposition, CT showed that only 3 of the 13 ovaries were outside the field. Even the 3 ovaries outside the field received approximately 300 cGy.
Lateral Ovarian Transposition
There are several advantages to laparoscopic transposition; as a result, this approach has become the most common. Laparoscopic transposition can be performed as an outpatient procedure with little disruption of the planned therapeutic schedule. The ability to do this easily will eliminate unnecessary transposition in the majority of cervical cancer cases where radiation therapy is not required. An important advantage of laparoscopic ovarian transposition is that radiation therapy can be initiated immediately postoperatively, preventing failure due to the ovaries migrating back to the irradiation field.17,51,52 In cases of vaginal or cervical cancers being treated by brachytherapy, laparoscopic ovarian transposition can be performed under the same anesthetic for inserting the brachytherapy device.53
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree