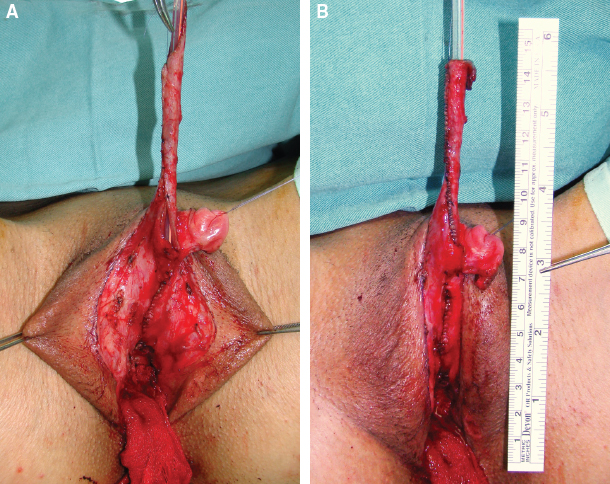
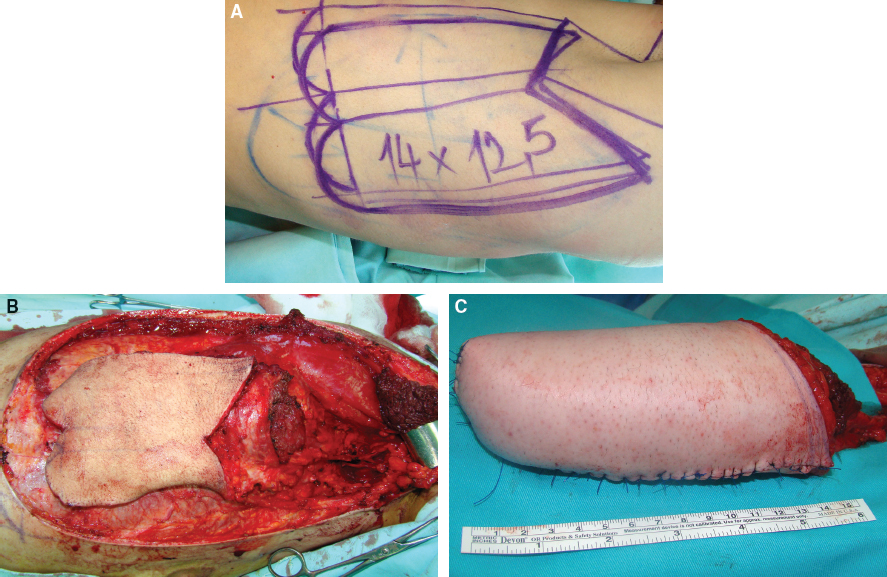
CHAPTER 10 Reconstruction of the neophallus is one of the most difficult elements in the surgical treatment of female transsexual patients. Although a variety of surgical techniques are available, their results are not equally acceptable to all patients. Overall the patient chooses the preferred surgical technique after he has been completely informed regarding all treatment options, the advantages, and possible complications.1 For patients requiring an adult-sized phallus, the myocutaneous latissimus dorsi free flap is a good option for phallic reconstruction. Various flaps (vaginal, labial, and clitoral flaps) and grafts (buccal mucosal graft) are recommended for urethral lengthening, whereas implantation of a penile prosthesis in the second stage enables penetration and sexual intercourse. However, the lack of erogenous sensitivity of the neophallus remains problematic. Metoidioplasty is a technically demanding and challenging surgical procedure that is used in female-to-male (FTM) transgender patients who want gender reassignment surgery without undergoing a complex, multistaged surgery to create an adult-sized phallus. This technique creates a neophallus from a hormonally hypertrophied clitoris in FTM patients who do not wish to have sexual intercourse.2,3 In patients who want a larger phallus, many different surgical techniques have been reported that use available local vascularized tissues or microvascular tissue transfers. An ideal phalloplasty includes one surgical stage, protective and erogenous sensitivity, good aesthetic appearance, a volume sufficient to place a protected prosthesis, sufficient rigidity to allow sexual intercourse, patency of the neourethra, and low donor-site morbidity.4–10 The most widely used flap for total neophalloplasty is the radial forearm flap.8 However, it has many drawbacks, such as an unsightly donor-site scar, very frequent urethral complications, and a small penis that does not allow the safe insertion of a penile prosthesis in most patients. These were the main reasons we developed a new technique with the myocutaneous latissimus dorsi free flap, which was based on favorable experimental and clinical experience.11–13 This flap has a reliable and suitable anatomy to meet the aesthetic and functional needs of phallic reconstruction. Because of its workable size, ease of identification, long neurovascular pedicle, and minimal functional loss after removal, the latissimus dorsi flap has been used for various reconstructions.14,15 The main advantage of this flap is its large surface area, allowing an excellent penile size (length and circumference), large enough to allow urethroplasty and implantation of a penile prosthesis. Moreover, the penis can be constructed to the size desired by the patient. Neophallus retraction seems less likely with muscle-based grafts than with fasciocutaneous forearm flaps, because denervated, well-vascularized muscle is less prone to contraction than connective tissue. Sexual function of this neophallus remains problematic, because the flap lacks orgasmic sensitivity; it is restricted to the glans, with a preserved dorsal nerve bundle incorporated at the base of the neophallus. Strong motivation and excellent cooperation of the partner are mandatory for successful sexual intercourse.11,12 Our present technique includes the removal of internal female genitalia, including hysterectomy, adnexectomy, and vaginectomy, the creation of a neophallus from the myocutaneous latissimus dorsi free flap, its fixation in the pubic region and anastomosis with the blood vessels of the right leg, and reconstruction of the scrotum. The second and third stages of phalloplasty (urethral reconstruction and penile prosthesis implantation) are performed several months after the first stage. Our phalloplasty can be performed as a separate surgery after or before metoidioplasty or at the same time as metoidioplasty as a one-stage procedure. Patients should receive hormonal treatment for a minimum of 1 year before surgery. The donor-site region must be treated with professional massage, which will improve skin elasticity and thus direct closure of the donor site after harvesting of the flap. The massage is performed regularly for at least 3 months before surgery. The donor site is defined as the nondominant side of the latissimus dorsi muscle region. A clear understanding of the anatomy of the clitoris is important for this surgical reconstruction. The clitoris consists of erectile bodies (paired bulbs and paired corpora, which are continuous with the crura), the glans clitoris, the neurovascular bundle dorsally, and the wide urethral plate ventrally. The glans is a midline, densely neural, nonerectile structure that is the only external manifestation of the clitoris. The distribution and course of the neurovascular bundle of the clitoris are similar to those of the penis; the blood supply of the clitoris comes from the deep artery and dorsal artery of the clitoris, which branch off from the internal pudendal artery. The wide urethral plate with well-developed spongiosal tissue is adherent to the corporeal bodies, forming a ventral chordee. The clitoris has fundiform and suspensory ligaments, as in penile anatomy. However, the clitoral ligaments are more developed and make it hidden and curved.16,17 Removal of female reproductive organs (that is, hysterectomy and bilateral salpingo-oophorectomy) can be performed either before or at the same time as phalloplasty. The vaginal mucosa is completely removed by colpocleisis, except for the part of the anterior vaginal wall close to the native urethral orifice, which is used for reconstruction of the bulbar urethra (Fig. 10-1). Lengthening of the clitoris begins with a circular incision beneath the clitoral glans at the border between the inner and outer layers of the clitoral prepuce and continues around the urethral plate and native urethral orifice. After total degloving, fundiform and suspensory clitoral ligaments are detached from the pubic bone to advance the clitoris, mobilizing it to enable its fixation in a new position at the base of the neophallus. Fig. 10-1 Female-to-male patient. A hysterectomy, bilateral salpingo-oophorectomy, and vaginectomy were performed through a vaginal approach. In FTM patients, the gap between the neourethra and female urethral meatus always exceeds 10 cm. Reconstruction of the neourethra begins with the reconstruction of its bulbar part. A vaginal flap is harvested from the anterior vaginal wall, with its base close to the female urethral meatus.18 This flap is joined with the remaining part of the divided urethral plate, which forms the bulbar part of the neourethra. Further urethral reconstruction includes using all available vascularized hairless tissue to lengthen the neourethra to the maximum extent, which prevents postoperative complications. In this way the new urethral opening is placed in the first half of the neophallus, minimizing the requests for longer neophallus urethroplasty. Both varieties of flaps, clitoral and labial, have fine supportive tissue that prevents fistula formation and yields satisfactory aesthetic results (Fig. 10-2). Fig. 10-2 A, Proximal urethra created with the urethral plate and a vaginal flap. A very long flap from both the labia minora and clitoral skin is dissected on a well-vascularized pedicle. B, The flap is tubularized, allowing an additional increase in urethral length. The vaginal space is closed, and the perineum is fashioned to resemble that of males. Both labia majora are joined in the midline over the neourethra, creating a one-sac scrotum. Silicone testicle prostheses are inserted into the labia majora, completing the scrotoplasty. The patient is placed in the lateral position (the upper torso is placed in a full lateral position at 90 degrees, and the pelvis is at a 30-degree angle) to provide access to the groin. The flap is marked on the latissimus dorsi donor site; it consists of two parts: a rectangular part for the neophallic shaft and a circular component for glans reconstruction (Fig. 10-3, A). Flap dissection starts with an incision of the anterior skin margin down to the deep fascia. The plane is developed between the latissimus dorsi and serratus anterior muscles with sharp and blunt dissection. The flap is divided inferiorly and medially, cauterizing the large posterior perforators of the intercostal vessels, and then lifted to expose the neurovascular pedicle. The pedicle, which is surrounded by fatty tissue, is identified and dissected proximally up to the axillary vessels. The thoracodorsal nerve is identified and isolated proximally for 3 to 4 cm, which preserves its vascularization. The flap is elevated completely except for the neurovascular bundle, which is not transected until the recipient vessels and nerve have been prepared for microanastomosis (Fig. 10-3, B). The latissimus muscle is fixed to the edges of the skin at several points to prevent layer separation during further dissection. The flap is tubularized, creating the neophallus while still perfusing on its vascular pedicle (Fig. 10-3, C). The circularized terminal part is rotated back over the distal body and sutured to create a neoglans. Thus a completely constructed neophallus is detached from the axillary region after clamping and dividing the subscapular artery, vein, and thoracodorsal nerve at their origins to achieve maximal pedicle length.
Female-to-Male Gender Affirmation Phalloplasty: Latissimus Dorsi Flap
Key Points
 The myocutaneous latissimus dorsi free flap is a reliable alternative to the radial forearm flap for neophalloplasty in female-to-male transgender patients.
The myocutaneous latissimus dorsi free flap is a reliable alternative to the radial forearm flap for neophalloplasty in female-to-male transgender patients.
 A synchronous two-team approach could be used (team one, harvesting of the flap; team two, dissection of the recipient area and recipient blood vessels for later microvascular anastomosis).
A synchronous two-team approach could be used (team one, harvesting of the flap; team two, dissection of the recipient area and recipient blood vessels for later microvascular anastomosis).
 It is possible to remove the vagina and reconstruct the scrotum with insertion of silicone testicle implants in the same stage.
It is possible to remove the vagina and reconstruct the scrotum with insertion of silicone testicle implants in the same stage.
 Both labia minora and dorsal hairless clitoral skin are harvested with the preserved blood supply for use in urethral lengthening.
Both labia minora and dorsal hairless clitoral skin are harvested with the preserved blood supply for use in urethral lengthening.
 The neophallus is placed just above the top of the labia majora, creating a good relationship between the phallus and newly created scrotum.
The neophallus is placed just above the top of the labia majora, creating a good relationship between the phallus and newly created scrotum.
 The neophallic urethra is reconstructed as a staged procedure with buccal mucosal and skin grafts.
The neophallic urethra is reconstructed as a staged procedure with buccal mucosal and skin grafts.
Indications and Contraindications
Surgical Technique: Main Procedure
Preoperative Assessment
Clitoral Anatomy
Removal of Female Reproductive Organs
Clitoral Lengthening and Repositioning
Urethral Lengthening
Reconstruction of the Perineum and Creation of the Scrotum
Flap Design and Marking
Abdominal Key
Fastest Abdominal Insight Engine