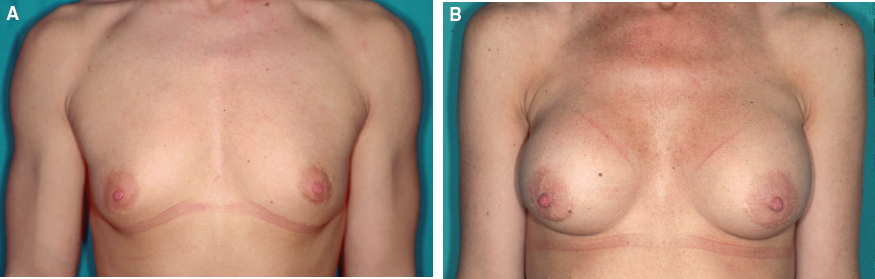
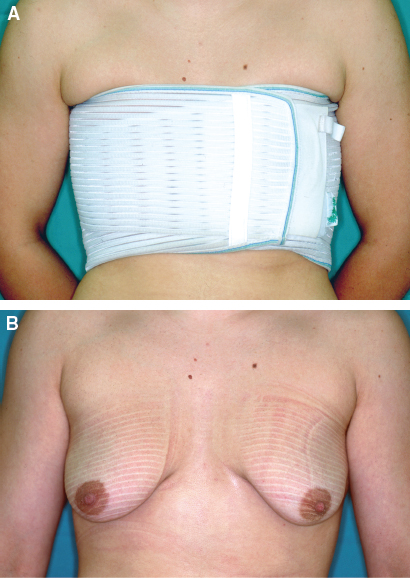
CHAPTER 3 Top surgery is one of the most commonly performed gender reassignment surgeries. Male-to-female top surgery consists of breast augmentation with implants and/or autologous tissue. Female-to-male top surgery includes mastectomy and creation of a male chest. The Standards of Care (SOC) of the World Professional Association of Transgender Health (WPATH) offers flexible guidelines for the treatment of people experiencing gender dysphoria and puts forth the following criteria for top surgery1: Although not an explicit criterion, it is recommended that transwomen undergo feminizing hormone therapy (minimum 12 months) before breast augmentation surgery. The purpose is to maximize breast growth to obtain better surgical (aesthetic) results. Top surgery can greatly facilitate patients’ experience of living in a gender role that is congruent with their gender identity. This experience is required for 12 months before bottom surgery (vaginoplasty or metoidioplasty/phalloplasty). However, for some transgender individuals, top surgery may be the only surgical step that is undertaken during transition. For most transwomen, breast augmentation (or breast “reconstruction”) greatly increases subjective feelings of femininity. Mammaplasty provides a more feminine profile, facilitating adjustment to the gender identity and increasing factors involved in passability (Fig. 3-1). In a prospective, noncomparative, cohort study, it was shown that the gains in breast satisfaction, psychosocial well-being, and sexual well-being after transwomen underwent breast augmentation were statistically significant and clinically meaningful to the patient shortly after surgery, as well as in the long term.2 Mammogenesis in transwomen receiving estrogens follows a pattern similar to female pubertal mammogenesis as described by Marshall and Tanner.3 As breast development, it is not exclusively dose responsive—67% to 75% of the transwomen require an augmentation mammaplasty, because hormonal treatment only results in a softly pointed breast as seen in young girls or the small conical form found in young adolescents (Tanner stage 2 or 3).4 Because breast prostheses are implanted in transsexuals with “young adolescent” breast development, the patient should be informed that the complex feminine form and age-related changes to the breast cannot be imitated by using symmetrical hemispheric implants. Therefore the results of an augmentation mammaplasty in a transwomen with minimal hormone-induced mammogenesis may be poor.4 Other anatomic differences, which should be taken into consideration in transwomen, are the wider male chest, a stronger pectoral fascia, a more developed pectoralis muscle, and the smaller dimensions of the nipple and areola. Usually a larger-volume breast implant is chosen by transwomen than that chosen for breast augmentation by a female patient, but even with a larger implant, it is often impossible to avoid abnormally wide cleavage between the breasts. The nipple and areola should always overlie the implant centrally, and a very medial position of these implants could result in a divergent nipple position with an unacceptable breast appearance.5 Despite some sexual differences in the chest wall and mammary anatomy, the implantation of breast implants is not essentially different from breast augmentation in a female patient, except that larger prostheses are usually used. The same choices apply regarding the type of implant, position of the pocket, and surgical approach. Patient and surgeon can choose between a silicone gel–filled implant and a saline-filled implant. In most patients, a textured implant is chosen to reduce the potential for capsular contracture. When a more cohesive gel–filled implant is chosen, it can be an anatomic implant, resulting in additional filling of prominence in the lower part of the breast. The incision can be either axillary, inframammary, or even periareolar, although the latter is less popular in transwomen because of the smaller size of the areola. If an inframammary incision is used, it should be positioned lower than the preoperative inframammary fold, because the distance between the inferior areolar margin and inframammary fold will expand after augmentation mammaplasty, probably resulting from the recruitment of the inframammary or even abdominal skin.4 The pocket for the implant can be created behind the glandular tissue or pectoralis muscle. Some authors recommend implanting the prosthesis in a subglandular position.4 This is especially indicated in patients who have more subcutaneous and glandular tissue to start with (Tanner stage 4 or 5). The surgical procedure is easier to perform and less painful. Many surgeons, however, prefer to put the implant in a retropectoral position. In this case the lower portion (as well as part of the medial origin) of the pectoralis muscle should be detached from the thoracic cage.6 In the retropectoral position, the prosthesis is covered with more soft tissue (important in thin patients), and a lower risk of capsular contraction has also been reported. In most institutions breast augmentation is often performed during the same surgical procedure as genital surgery. In this case the operation starts with breast augmentation, which is the most sterile part of the intervention. However, both procedures can even be carried out simultaneously if two surgical teams are available. For various reasons, some patients may prefer to have the augmentation mammaplasty performed as a preceding procedure (eventually combined with castration to allow official gender change) or as a subsequent surgical intervention. Fat grafting or lipofilling is a technique in which fat is harvested by liposuction of the abdomen or thighs. Subsequently, the fat is centrifuged to separate the oil, fluid, and blood supernatants.7 As a result, a concentrated, “purified” fat sample is obtained, which can be injected into the subcutaneous plane (Fig. 3-2). In transwomen who already have some breast volume from hormone treatment, fat grafting can be a good option to provide a moderate augmentation of the breast, thereby avoiding the need for an implant. However, patients should be informed that a variable percentage of the injected fat is resorbed, and that a second or even a third procedure may be necessary to achieve sufficient volume. Breast reconstruction with autologous free flaps or pedicled flaps in transwomen has not yet been described. However, in an era in which screening for a genetic predisposition of breast cancer is more commonly performed, this procedure may become important in the future. A bilateral prophylactic mastectomy and consecutive primary reconstruction with either autologous tissue (for example, a deep inferior epigastric perforator flap) or a breast implant should be offered to patients with a genetic predisposition for breast cancer.8 Kanhai et al4 reported the main (but rarely occurring) complications after breast augmentation: hematoma, synmastia, capsular contracture, a decreased sensation in the nipple and/or part of the breast, leakage of the prostheses (more obvious in saline-filled prostheses than in cohesive silicone gel–filled prostheses), and malposition of the prostheses. Although it is very rare in these patients, mastopexy can be the treatment of choice to correct substantial mammary ptosis, but usually an augmentation is sufficient to fill out the (slightly) ptotic breasts. Galactorrhea is another rare condition that can occur preoperatively or postoperatively. It requires an extensive hormonal evaluation, with particular attention to the pituitary gland. Except for hormonal causes, excessive prolactin secretion causing galactorrhea may also result from a peripheral stimulus, such as breast manipulation or intercostal nerve stimulation. Galactorrhea in the latter case is associated with chest incisions or inflammation of the chest wall and thus may also be caused by mammary implants. In many patients, however, no cause for the galactorrhea can be found, and the condition remains idiopathic. Postoperative follow-up is mandatory in all patients undergoing breast augmentation. Gooren et al9 performed a cohort study documenting the occurrence of breast cancer in 2307 transgender individuals with an exposure to cross-sex hormones between 5 and 30 years and reported 10 cases of breast cancer in transwomen. All patients received oral estrogens for prolonged periods to maintain secondary female characteristics. Three of these 10 cases were not estrogen-dependent breast carcinomas. Their study suggested that cross-sex hormone administration does not increase the risk of breast cancer development in transwomen. Breast carcinoma incidences were comparable with male breast cancers and thus lower than in the female population. However, the historic use of cross-sex hormones may have been too short for malignancies to develop. Therefore good screening and follow-up are imperative. Moreover, because breast examinations are also very well accepted by transwomen, transgender patients should be encouraged to participate in relevant cancer screening protocols, which for breast cancer screening is the same as for cisgender women.10 Routine preoperative investigation of family history is imperative. Screening for genetic predisposition (for example, BRCA mutations) should be considered in patients with multiple breast and/or ovarian cancers within their family (often diagnosed at an early age)—two or more primary breast and/or ovarian cancers in a single family member and/or cases of male breast cancer within their family. Because hormonal treatment has little influence on breast size, the first (and arguably most important) surgery performed in transmen is the creation of a male chest by means of subcutaneous mastectomy (SCM). This procedure allows the patient to live more easily in the male role and thereby facilitates the experience of living in a gender role that is congruent with their gender identity, which is a prerequisite for external genital surgery. A large body of literature on the optimal technique for performing SCM exists, but the majority focuses on women with breast disease or men with gynecomastia. There is a paucity of information regarding removal of the breasts in transmen. Obviously, the male and female chests are anatomically different.11,12 The female chest has excess skin, excess glandular tissue, and a surrounding surplus of subcutaneous fat. Regarding the inferior confinement of the breast, in the female, the inframammary fold is well defined. In the average male, the chest does not show an inframammary fold, and the inferior margin of the pectoralis muscle (often somewhat squared by rudimentary breast tissue and nipple) represents the dim inferior margin of the chest. The importance of obliterating the inframammary fold while contouring the male chest has been stressed by several authors.11 From a purely anatomic viewpoint, SCM in transmen is virtually identical to that of the mastectomy for breast disease or prophylaxis. However, the goals for transmen differ, because they include aesthetic contouring of the chest wall by removal of breast tissue and excess skin, reduction and proper positioning of the nipple and areola, obliteration of the inframammary fold, and minimization of chest wall scars—in short, the creation of an aesthetically pleasing male chest.12 Many of the techniques for the treatment of gynecomastia have been used or modified in SCM for transmen, and the methods and indications for each have been discussed in the literature.12–14 The reports describe liposuction, semicircular circumareolar techniques, concentric circular techniques, transareolar incisional techniques, and more radical procedures, such as breast amputation with a free nipple graft.15–19 Poor aesthetic outcomes include contour abnormalities (breast, inframammary fold, and nipple), issues related to the nipple-areola complex (NAC) (size, placement, and viability), skin redundancy, and poor scarring.11 Secondary corrections are occasionally necessary. Indeed, performing SCM in transmen is more difficult than correction of gynecomastia in males, because in most cases transmen will usually have more breast volume and a greater degree of skin excess and ptosis. According to Hage and Bloem,12 skin excess and not breast volume is the factor that should determine the appropriate SCM technique. Based on more than 400 SCMs we have performed for transmen over the past 15 years, we agree that skin quality—specifically, skin “elasticity”—is also a key factor. It can make the difference between a good aesthetic outcome and a poor one, especially with a less experienced surgeon. In this patient population, poor skin quality can be exacerbated when the patient has engaged in years of “breast binding” (Fig. 3-3).
Top Surgery
Key Points
 Top surgery is one of the most commonly performed gender reassignment surgeries.
Top surgery is one of the most commonly performed gender reassignment surgeries.
 For most transwomen, breast augmentation greatly increases subjective feelings of femininity.
For most transwomen, breast augmentation greatly increases subjective feelings of femininity.
 Despite some sexual differences in chest wall and mammary anatomy, the implantation of a breast prosthesis is not essentially different from breast augmentation in a female patient.
Despite some sexual differences in chest wall and mammary anatomy, the implantation of a breast prosthesis is not essentially different from breast augmentation in a female patient.
 Breast volume, as well as skin quality, is a key factor that should determine the appropriate subcutaneous mastectomy technique in transmen.
Breast volume, as well as skin quality, is a key factor that should determine the appropriate subcutaneous mastectomy technique in transmen.
 The Ghent algorithm helps us to choose from five techniques, resulting in an aesthetically pleasing male chest.
The Ghent algorithm helps us to choose from five techniques, resulting in an aesthetically pleasing male chest.
Indications and Contraindications
 A persistent, well-documented gender dysphoria
A persistent, well-documented gender dysphoria
 The capacity to make a fully informed decision and to give consent for treatment
The capacity to make a fully informed decision and to give consent for treatment
 Age of majority in a given country
Age of majority in a given country
 If a prospective candidate for top surgery has a significant medical or mental health concern, it must be well controlled.
If a prospective candidate for top surgery has a significant medical or mental health concern, it must be well controlled.
Breast Augmentation in Transwomen
Surgical Techniques
Breast Implant
Fat Grafting
Autologous Flap Surgery
Complications
Subcutaneous Mastectomy in Transmen
Abdominal Key
Fastest Abdominal Insight Engine