Chapter 34 Female Infertility
INTRODUCTION
Definitions
Infertility
Infertility is associated with a broad spectrum of definitions and classifications, indicating that it is interpreted very differently by various groups and individuals (Table 34-1). Broadly defined, infertility depicts a diminished capability to conceive and thereby bear children.
| Infertility | One-year period of unprotected intercourse without successful conception |
| Subfertility | An ability to conceive a pregnancy that is decreased from age-matched and population-matched controls |
| Fecundability | The probability that actions taken in a single menstrual cycle will result in a pregnancy |
| Fecundity | The probability that actions taken in a single menstrual cycle will result in a live birth |
| Primary infertility | A patient who has never been pregnant |
| Secondary infertility | A patient with a previous history of a pregnancy regardless of outcome (i.e., spontaneous abortion, ectopic pregnancy, stillbirth, or live birth) |
| Chemical pregnancy | A pregnancy diagnosed by a positive β-hCG titer that spontaneously aborts before clinical verification by other means such as transvaginal ultrasonography |
| Clinical pregnancy | A pregnancy diagnosed by a positive β-hCG titer and clinically verified, usually with transvaginal ultrasound (i.e., intrauterine sac or fetal cardiac activity) or, in cases of miscarriage, by pathologic examination |
The medical definition of infertility is a 1-year period of unprotected intercourse without successful conception. Utilizing this strict interpretation, infertility is a common problem, affecting at least 10% to 15% of all couples. Based on observational data, the remaining 85% to 90% of couples attempting conception will achieve a pregnancy within that 1-year timeframe.1,2
When viewed across the entirety of their reproductive lifetimes, the problem becomes even more common, and up to 25% of women can have an episode of undesired infertility for which they actively seek medical assistance.3 This is because the desire to conceive can change markedly over the reproductive life of a woman, which is generally considered to be between ages 15 and 44. Couples additionally may not actively attempt conception continually during an entire calendar year, but sporadically across a wider timespan.
Normal Fecundity Rates
Overall birth rates in the United States have changed markedly over the past 200 years due to an innumerable set of changes in physical, environmental, and social circumstances. The first official U.S. census was performed in 1790 and reported an overall crude birth rate of 55 per 1000 population.4
To measure the true reproductive capacities of Homo sapiens sapiens as individual biologic beings, studies of fertility in the so-called natural populations should be closely examined. Natural population is a term given to groups in which couples are generally permitted to reproduce without any societal limitation to reproduction.5
The Hutterites of North America are an often utilized example of such a natural population.6–8 This sect of Swiss immigrants originally came to the New World in the mid-sixteenth century and eventually settled in several locations, all in the northern United States and southern Canada. The Hutterites are a closed and very close-knit, truly communal society. There are only six surnames within the entire social structure. All families share equally, and there is therefore no direct impetus or incentive to limit the size of the nuclear family unit. Consequently, they absolutely refuse to use contraception. Overall, the average number of pregnancies per female was 15, while the number of live births averaged 11. Remarkably, although the overall rate of infertility was only 2.4%, a marked decrease in fecundity with advancing age has been documented, with 89% of Hutterite women having their last live birth after age 34, 67% bearing children after age 40, and a mere 13% after age 45. We will discuss the effects of advancing age on fertility later in this chapter.
Data from studies such as these have suggested that fertility in women generally peaks between ages 20 and 24.9,10 It remains fairly stable until approximately age 30 to 32, at which time it begins to decline progressively.11,12 This decline accelerates markedly after age 40. At a bottom line, therefore, fecundity rates in women at age 20 approximate 20% per cycle. This is the peak fecundity rate reflected in the natural setting and can be used as the gold standard when comparing success rates. Subsequently, fertility rates decrease by 4% to 8% in women age 25 to 29; 15% to 19% lower by age 30 to 34; 26% to 46% by age 35 to 39, and 95% lower at age 40 to 45.4,13
Over short periods of time, any cross-sectional population of infertile couples will behave in a relatively uniform manner; in other words, a statistically constant proportion will conceive with each additional cycle of treatment and follow-up. Over longer periods of time however, cycle fecundability appears to decline markedly and the overall cumulative pregnancy rate eventually plateaus.14,15
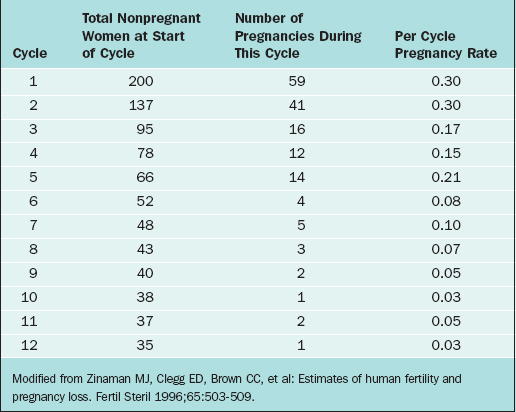
The overall pregnancy rate will never reach 100%. This is primarily due to the overall heterogeneity of infertile and subfertile populations as a whole. Those couples with the highest relative fecundity rates achieve pregnancy most rapidly and are therefore removed from the population, leaving only those couples with more serious problems remaining in the infertile pool. As an example, Zinaman and colleagues reported a prospective observational study of 200 healthy couples desiring to achieve pregnancy and followed them conservatively over a period of 12 menstrual cycles.16
The fecundability rates were highest during the first 2 months of follow-up, greater than 25% per cycle, and had dropped drastically by 6 months to less than 10% per cycle. By the end of the trial, the per cycle fecundability rate was only 3% (Table 34-2).
CAUSES OF INFERTILITY AND SUBFERTILITY
The simplest manner to express the overall causes of medical and environmental conditions that cause infertility is to divide the overall problem into male factors and female factors. One of the broadest investigations concerning these categorizations was conducted by the World Health Organization (WHO) Task Force on the Diagnosis and Treatment of Infertility in 1992.17 Although there were several significant differences in their findings depending on the economic environment of the populations studied, the data was remarkably uniform.
The actual percentages that individual factors are found to be the primary cause of infertility vary widely between studies. However, in a broad meta-analysis of more than 20 trials studying infertile couples, the following primary diagnoses were found: disorders of ovulation (27%), abnormal semen parameters (25%), abnormalities of the fallopian tube (22%), unexplained infertility (17%), endometriosis (5%), and other (4%).18 An additional cause is cervical factors, including cervical stenosis, which accounts for up to 5% of infertility in many series.19
Direct observations on human populations allow us to group the causes of infertility into five broad categories, listed in Table 34-3. This broad listing of root causes, although perhaps not complete, can be used as a basis for the initial evaluation of the infertile couple. The overall purpose of the evaluation is to determine which of these overall processes needs to be improved, repaired, or overcome to establish a successful pregnancy. Each question asked at the initial interview, each laboratory test requested, every diagnostic procedure performed must always reflect the need to categorize the problem as simply as possible to suggest the appropriate remedy.
Table 34-3 Causes of Infertility
Infertility and Weight
Anovulation, oligo-ovulation, subfertility, and infertility have all been commonly described in women who are significantly above or below their ideal body weight.20
In one study, women with anovulatory infertility were stratified by body mass index (BMI) and compared to normal fertile controls.21 It was clear that the overall risk of ovulatory abnormality was increased with any significant variation from ideal body weight. Obese women (BMI > 27 kg/m2) had a relative risk of anovulatory infertility of 3.1 compared to women closer to their ideal body weight (BMI 20–25 kg/m2). At the same time, women with a BMI lower than 17 kg/m2 had a relative risk of anovulatory infertility of 1.6. Although the relative risk of anovulation was highest in obese women, it was also significantly increased in underweight women as well.
INITIAL EVALUATION OF THE INFERTILE COUPLE
Last, this initial evaluation should lay down the guidelines of possibility to the patients. Not all therapies will work in all patients and not all patients will become pregnant regardless of the therapy. The couple should be given a concise outline of the possibilities of care and all of the information necessary to make an intelligent decision concerning their options. When the patients are allowed to have such an involvement in decision making, it allows them to more easily accept the failure of any individual therapy and helps them reach closure if success is never attained.
Primary Elements of the Initial Infertility Evaluation
The initial evaluation consists of seven primary elements (Table 34-4). It is recommended that the entire initial evaluation should be completed before direct recommendations concerning treatment are suggested to the patients. Most patients will accept a temporary delay in their therapies while full evaluation of all aspects of their clinical state is accomplished far easier than they do frequent changes in their protocol interspersed with intermittent testing and analysis.
Table 34-4 Initial Infertility Evaluation
| History |
| Physical examination |
| Semen analysis |
| Tests of hormonal status |
| Assessment of tubal patency |
| Tests of ovulatory status |
| Assessment of luteinization |
HISTORY
In the female partner, the relevant medical history concerning the causes and the nature of infertility covers a broad range of subjects.22,23
Attention to detail during this collection of data is imperative.
Demographics
It is important to determine where the patient has lived. Extragenital Mycobacterium tuberculosis infections remain one of the most common causes of pelvic inflammatory disease in the third world.24–26
In areas where tuberculosis is an endemic disease, such as Vietnam and the Philippines, tuberculus epididymitis and salpingitis are common. If recent diagnostic testing has not been done, placement of an intermediate purified protein derivative (iPPD) should be performed and the results drive further investigation. Even in the United States, up to 2% to 5% of tubal disease can be tubercular in nature.27
Menstrual History
Information should be obtained about the following subjects:
Gynecologic History
Gynecologic questioning should include questions about the following subjects:
Obstetric History
Family History
Table 34-5 Genetic Screening for Various Ethnic Groups
| Ethnic Group | Disorder | Screening Test |
|---|---|---|
| Ashkenazi Jews | ||
| African Americans | Sickle cell anemia | Presence of sickle cell hemoglobin, confirmatory hemoglobin electrophoresis |
| Mediterranean populations | Beta-thalassemia electrophoresis | Mean corpuscular volume (MCV) < 80%, followed by hemoglobin |
| Southeast Asians Chinese | Alpha-thalassemia | Hemoglobin electrophoresis if mean corpuscular volume < 80% |
| Cystic fibrosis | DNA analysis of specified panel of 25 CFTR gene mutations |
Adapted from American Society for Reproductive Medicine: Appendix A: Minimal genetic screening for gamete donors. In 2004 Compendium of ASRM practice committee and ethics committee reports. Fertil Steril 82:S22–S23, 2004.
Social History
The utilization of herbal preparations in the United States has reached epidemic proportions. As much as 32% of the population as a whole use some type of herbal preparation purchased over the counter,36 but less than 8% will volunteer these substances when asked openly what medications they are taking.37
Many of these products have ingredients that contain active hormones, estrogen disrupters, vasoactive amines, or anti-inflammatory ingredients, all of which can have a marked effect on both the menstrual cycle and fecundity. Not all of these products are contraindicated; their ingredients should be examined by the physician for possible effects on reproduction. There are many on-line (www.pda.com or www.NaturalDatabase.com) and print compendiums that outline the specific nature of the herbal and vitamin ingredients of these over-the-counter supplements.38,39
Sexual History
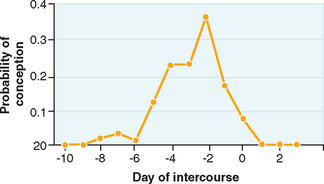
Coital Frequency and Timing
It is important to be aware of the association of coital timing and the probability of successful conception (Fig. 34-1). Because activated sperm can last for up to 80 hours in the female reproductive tract,40,41 it has long been a general recommendation that intercourse occur at specific times during the menstrual cycle to ensure that at the time of expected ovulation there will be capacitated sperm available for fertilization. There can, however, be a significant diminution of both cycle and overall fecundity rates if coitus becomes too frequent.42,43
Dyspareunia
Is there deep thrust dyspareunia? Deep thrust dyspareunia can be a very common gynecologic problem, but it is usually an episodic or intermittent complaint.44
The etiology of this symptom stems from the relative immobility of the pelvic organs and arises from rapid stretching of the uterosacral and cardinal ligaments due to the sudden movement of the cervical/uterine unit during coitus. It can also be caused by direct pressure on nodular lesions of endometriosis in the uterosacral ligaments or in the pouch of Douglas. Deep thrust dyspareunia should raise the suspicion of an organic disease, such as endometriosis or adenomyosis.45–48
Is there increased pain with orgasm? Orgasm is physiologic, typified by rhythmic contractions of the orgasmic platform and the uterus, created involuntarily by localized vasocongestion and myotonia.49 These contractions have a recorded rhythmicity of approximately 0.8 seconds, as the tension increment is released in the orgasmic platform, but accumulates slowly and more irregularly in the uterine corpus. The eventual strength of these uterine contractions may be 4 to 5 times the baseline to peak intensity of a labor contraction.50
Localized production of prostaglandins and endoperoxidases in both endometriosis and adenomyosis can intensify these contractions and cause sensitization of C-afferent nerve fibers in the pelvis, thereby eliciting greater pain with each of these individual contractions.51 Marked pain with orgasm may therefore be a diagnostic suggestion of organic disease of the reproductive tract.52
Sexual Orientation
In the United States alone, an estimated 2.3 million women identify themselves as lesbians.53 Many of these women will present for medical therapy of this absolute male factor infertility, either alone or with a partner. Traditionally, many physicians have altered their history taking and diagnostic regimen in lesbian populations due to the seeming absence of significant risk factors for pelvic inflammatory disease and other sexually transmitted diseases. However, this is not always the case.
Numerous studies have reported that 53% to 99% of women who identify themselves as lesbians have at some time had sex with men, and 25% to 30% of these women continue to have sex with men.54
Up to 25% of this population has been pregnant at one time, and more than 60% of those who had been pregnant report having one or more induced abortions.55
REVIEW OF SYSTEMS
Headaches
Patients should be questioned to find out both the frequency of self-medication with nonsteroidal anti-inflammatory drugs (NSAIDs) and the dosage taken. Headaches can be associated with pituitary lesions, such as craniopharyngiomas56,57 and prolactinomas.58,59 Prolactinomas are relatively common causes of anovulation.
Each can cause hormonal derangements that lead to anovulation and infertility. Additionally, frequent headaches of any etiology may lead a patient to self-medicate with large doses of over-the-counter NSAIDs. It has been suggested that at high doses, these medications can interfere with the inflammatory processes of ovulation and implantation.60,61 Patients should also be advised to avoid taking these medications during their therapeutic protocols to prevent these abnormalities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree