Type of incontinence
Frequency
Never
Rarely
Sometimes
Usually
Always
Solid
0
1
2
3
4
Liquid
0
1
2
3
4
Gas
0
1
2
3
4
Pad usage
0
1
2
3
4
Lifestyle impact
0
1
2
3
4
An often overlooked component of the history of the patient suffering from fecal incontinence is the presence of other pelvic floor complaints. Physicians should be sure to inquire about the presence of any form of rectal prolapse as well as the presence of urinary incontinence or genital organ prolapse. There is significant overlap of symptoms in this complex patient population.
Physical Examination
A complete physical examination will include inspection of the perianal skin for scars from prior surgeries, trauma or birthing injuries, fistulae, excoriation from chronic soiling, or large prolapsing hemorrhoids.
A specific evaluation of the perineal body in parous females should include palpation to determine if it is thinned.
At rest, the anal canal should be well approximated, not patulous. A patulous anus suggests a possible rectal prolapse, which is best reproduced by asking the patient to Valsalva while sitting on a toilet or squatting. Checking the perianal sensation to pinprick as well as the anocutaneous “wink” reflex will serve as a simple assessment of neurologic function.
Digital rectal examination can reveal masses or a fecal impaction. It also provides a gross assessment of both resting tone and voluntary squeeze.
Lastly, anoscopy or potentially a rigid vs. flexible proctosigmoidoscopy may reveal inflammatory bowel disease, infectious proctitis, or neoplastic process if suspected.
Diagnostic Studies
Endoanal Ultrasound
Endosonography has become the diagnostic cornerstone of the anorectal physiologic evaluation of fecal incontinence.
The ultrasound provides excellent imaging of the internal anal sphincter, which appears hypoechoic (Fig. 18.1).
Fig. 18.1
Normal endoanal ultrasound. The red line illustrates the lateral border of the external anal sphincter (hyperechoic) while the yellow depicts the lateral border of the internal anal sphincter (hypoechoic)
The external sphincter is hyperechoic, and scar tissue often has a mixed echogenicity appearance.
The most important parameter is to determine if the musculature is intact or if there are traumatic defects present. When present, defects in the musculature should be measured.
Additionally, the perineal body thickness (PBT) should be measured. PBT less than 10 mm is considered abnormal, and those patients with PBT greater than 12 mm are considered unlikely to have a sphincter defect in the absence of prior reconstructive surgery (Fig. 18.2).
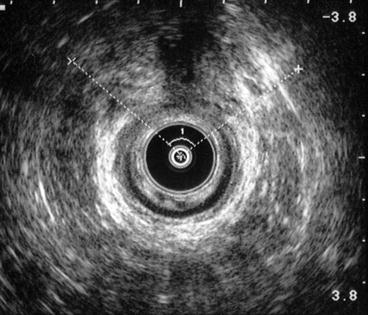
Fig. 18.2
Endoanal ultrasound with anterior sphincter defect (internal and external)
Anorectal Manometry
Anorectal manometry provides important information about the functional status of the anal sphincters and distal rectum. There is no standardized method of manometric evaluation. Several methods have been described.
Microtransducers can be used in the anal canal and are well tolerated by patients. Multichannel water-perfused catheters are perhaps the most common tool used to perform anal manometry.
The resistance of flow of fluid from the catheter determines pressure measurements.
Measurements can be taken in a continuous fashion (continuous pull-through) or at set levels within the anal canal (station pull-through).
Measurements
Resting Pressure. The mean resting pressure in healthy volunteers ranges from 40 to 70 mmHg. The internal anal sphincter generates the majority of the resting pressure. This smooth muscle is in a continuous state of maximal contraction accounting for 55–60 % of resting tone.
Squeeze Pressure. The maximal squeeze pressure in healthy individuals is two to three times the baseline resting value. The external anal sphincter is the main contributor to the generation of these pressures. Traumatic defects of the external anal sphincter, whether from obstetric or surgery, often result in decreased squeeze pressures.
High-Pressure Zone. The high-pressure zone is defined as the length of the internal anal sphincter, through which pressures are greater than half of the maximal resting pressure. The high-pressure zone is approximately 2–3 cm in women and 2.5–3.5 cm in men.
Rectoanal Inhibitory Reflex. The rectoanal inhibitory reflex (RAIR) is thought to play a role in the fine adjustments of continence. Rectal distension, usually with small volumes (10–30 mL), causes a contraction of the external anal sphincter followed by a pronounced internal anal sphincter relaxation. This reflex enables the sensory mucosa of the anal canal to “sample” the contents of the distal rectum and the patient to distinguish between gas, liquid, and solid stool. This reflex is absent or abnormal in patients with Hirschsprung’s disease, Chagas’ disease, dermatomyositis, and scleroderma.
Rectal Sensation. Alterations in rectal sensation can lead to decreased fecal continence. Rectal sensation is measured with an intrarectal balloon and incremental instillation of known volumes of air. Sensation is generally achieved with 40 mL air. Overflow incontinence can result from a decrease in rectal sensation and subsequent fecal impaction.
Rectal Compliance. Compliance is determined by the change in pressure associated with a change in volume (C = V/P). This is calculated by subtracting the volume of first sensation from the maximum tolerable volume and dividing by the change in pressure at these two points. A noncompliant rectum can contribute to fecal incontinence as the patient is not able to accommodate the amount of stool presented to the rectum. This is common in conditions, which cause proctitis.
Pudendal Nerve Terminal Motor Latency (PNTML)
Pudendal neuropathy has been implicated in the etiology of fecal and urinary incontinence. Assessment of the PNTML is an important component to the evaluation of the patient with fecal incontinence. A disposable electrode is attached to the examiner’s finger, which is then directed toward the ischial spine, and electrical impulses are delivered to the pudendal nerve. The time for response at the level of the external anal sphincter is measured. Normal response is within 2.0 ± 0.2 ms.
Electromyography
Anal electromyography (EMG) relies on the use of a concentric needle electrode to record electrical activity generated by the anal sphincter muscle fibers. Sequential recordings of the motor unit potentials are taken circumferentially around the anal canal.
Defecography
Defecography is the radiological visualization of the act of defecation. It provides a picture of the successive phases of defecation and gives a dynamic impression of pelvic floor activity during these actions. Changes in the rectal configuration and the anorectal angle become visible, and the degree of evacuation can be studied.
Colonoscopy
Endoscopic evaluation of the colon and rectum should be considered in the evaluation of patients with fecal incontinence to exclude a mucosal lesion or inflammatory condition, which could cause a change in the stool consistency or rectal compliance.
Treatment
Nonoperative Management
Medical Therapies
There are a variety of pharmacotherapies available for the medical management of fecal incontinence, but ultimately the number of randomized, placebo-controlled trials is limited. In fact, the Cochrane Database systemic review on the subject stated “there is little evidence with which to assess the use of drug therapies for the management of fecal incontinence.”
Medical management therapies are broadly broken down into the following categories: bulking agents, constipating agents, and laxative regimen with scheduled disimpactions.
Bulking Agents
Fiber, both natural and synthetic, has long been a staple in treatment of minor fecal incontinence. It has the benefit of adding bulk and has the ability to absorb additional fluid, providing a more solid stool in the face of mild chronic diarrhea.
Constipating Agents
In patients with diarrhea-predominant irritable bowel syndrome, it is estimated that 20 % have associated fecal incontinence.
It therefore stands to reason that use of constipation-inducing drugs, such as loperamide, codeine, diphenoxylate plus atropine, difenoxin plus atropine, and amitriptyline, is of utility for this group of patients. Loperamide is a synthetic opioid, which inhibits small and large intestinal peristalsis via the m (Mu) receptors in the gut. It has also been shown to increase anal resting sphincter pressure, improve rectal sensation, and retention of fluid load, as well as increase the RAIR. Amitriptyline has also been suggested as therapy based on its anticholinergic properties leading to a reduction in the frequency and amplitude of rectal motor complexes.
Laxative Regimen with Scheduled Disimpactions
In contrast to patients with diarrhea, patients with constipation and fecal impaction experience fecal incontinence secondary to overflow incontinence. Chassagne et al. compared a regimen of 30 g lactulose daily to 30 g of lactulose daily with the addition of a daily glycerin suppository and a weekly tap water enema in 206 institutionalized elderly patients with a history of prior fecal impaction and at least weekly episodes of fecal incontinence. The patients receiving the suppositories and weekly enemas in addition to the lactulose had a 35 % reduction in fecal incontinence episodes and a 42 % reduction in soiled laundry.
Biofeedback
The goal of biofeedback is to use visual, auditory, or other forms of sensory information to improve a patient’s ability to sense rectal distention and reinforce appropriate sphincter contraction.
Published studies typically demonstrate improvement in continence for both adults and children as a result of biofeedback in over 70 % of the patients.
Current described methods are widely variable and include weekly or biweekly sessions of 30 or 60 min, use of home practice machines, EMG, manometry, and even ultrasound. Long-term, the benefits of biofeedback are less clear, with many authorities suggesting an attenuation of results and the need for “refresher” training sessions. Regardless, a trial of biofeedback is considered an important noninvasive, first-line therapeutic option for highly motivated patients who have failed medical management.
Secca® Procedure
The Secca® procedure involves the use of radiofrequency delivered as an alternating current at high frequency leading to frictional movement of ions and generation of heat or thermal energy. As a result of the delivered thermal energy, there is immediate contraction of collagen fibers, which are then permanently shortened via remodeling resulting in a tightening of the muscle.
In Secca®, the radiofrequency is delivered to the anal sphincter under constant monitoring of the temperature and tissue impedance while simultaneously cooling the probes at the surface to minimize mucosal damage.
The Secca® procedure is typically performed in an outpatient, ambulatory setting under intravenous sedation with local anesthetic. Prophylactic antibiotics are given. The patient is positioned in either prone jackknife or lithotomy, following which, the handpiece is inserted into the anal canal and lined up, so the four needle electrodes will be deployed at the level of the dentate line.
The patients selected are generally those with mild to moderate complaints of fecal incontinence who have failed conservative measures including dietary modification, pharmacotherapy and biofeedback, and do not have a demonstrable sphincter defect.
To date, the studies have been limited by either small sample size or length of follow-up.
Injectables
Injection of a biocompatible bulking agent has been adapted from its initial reported successful application in the treatment of urinary incontinence. Its chief application is for the treatment of minor fecal incontinence due to internal anal sphincter dysfunction.
This option gains significance because surgical repair of the internal anal sphincter has not been shown to be effective, whereas more aggressive operations and their attendant complications are typically out of proportion to the complaints of this specific patient population. Proponents of this therapy cite the fact that it is a safe, minimally invasive therapy, typically administered on an outpatient basis, in some instances in an office setting with minimal complications under local anesthetic alone or with intravenous sedation.
The technique involves injection of a bulking agent either into the anal submucosal or intersphincteric space.
Currently the two most studied materials are silicone biomaterial and carbon-coated microbeads.
The mechanism of action is not fully understood, but Davis et al. suggested an increase in anal resting pressure secondary to augmentation of the anal cushions and restoration of anal canal symmetry. Other proposed mechanisms include bulking of the anal canal providing increased resistance to the passage of stool, allowing for improved sensation and that fibrosis over time contributes to increased sphincter muscle volume.
Typically, the maximal improvement in fecal continence is observed within the first 1–6 months and appears durable up to 1–2 years later.
Because of concerns of absorption and migration of the bulking agent, further long-term data are still needed.
Additionally, the ideal number and location of injections, utility of ultrasound guidance for said localization, and which materials and volume are most suitable for injection have yet to be definitively determined.
Table 18.2 summarizes the results of the use of injectables for the treatment of fecal incontinence.
Table 18.2
Injectable anal sphincter bulking agents for treatment of minor fecal incontinence
Author (year)
N
Bulking agent
Significant improvement of fecal incontinence
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access




