A man who desires restoration of fertility after vasectomy has two main treatment options for having his genetic child: vasectomy reversal or sperm extraction with subsequent in vitro fertilization with intracytoplasmic sperm injection. Microsurgical reconstructive techniques and their widespread availability have made vasectomy reversal a realistic option for many couples; however, vasectomy reversal outcomes are varied because there are many factors that alter the chance of success. Some of these factors become known preoperatively, whereas others can only be ascertained at the time of surgery. Intraoperatively, the urologist must identify factors and understand how they will affect the decision to proceed. This article systematically reviews each of these phases of decision-making and management.
A man who desires restoration of fertility after vasectomy has two main treatment options for having his genetic child: vasectomy reversal or sperm extraction with subsequent in vitro fertilization with intracytoplasmic sperm injection (IVF-ICSI). Other options for parenting include donor sperm or adoption. Microsurgical reconstructive techniques and their widespread availability have made vasectomy reversal a realistic option for many couples. However, the technical and functional success of these reconstructive procedures, reported as patency and pregnancy rates, respectively, are varied. Studies on vasovasostomy (VV) outcomes report patency rates between 75% and 86% and pregnancy rates between 45% and 70%. Studies on vasoepididymostomy (VE) outcomes report patency rates between 31% and 92% and pregnancy rates between 10% and 50%. Because couples have a variety of options for parenting, it would be helpful to identify factors that predict the outcome of attempted reconstruction for an individual.
Vasectomy reversal outcomes are varied because there are many factors that alter the chance of success. Some of these factors become known preoperatively, whereas others can only be ascertained at the time of surgery. Preoperatively, the urologist must identify and understand the predictive value of these factors in order to properly advise the patient and his partner. The discussion with the couple should include a comparison of their likelihood of success with vasectomy reversal compared to their likelihood of success with testicular sperm extraction, which yields 100% successful sperm retrieval rates in cases of obstructive azoospermia, and subsequent IVF-ICSI, which yields 20% to 37% pregnancy rates per initiated cycle, as per the most recently published report from the Centers for Disease Control in 2005. Intraoperatively, the urologist must identify factors and understand how they will affect the decision to proceed to a VE. The significance of postoperative management is unclear; nevertheless, it deserves consideration. This article systematically reviews each of these phases of decision-making and management.
Preoperative factors
Obstructive Interval
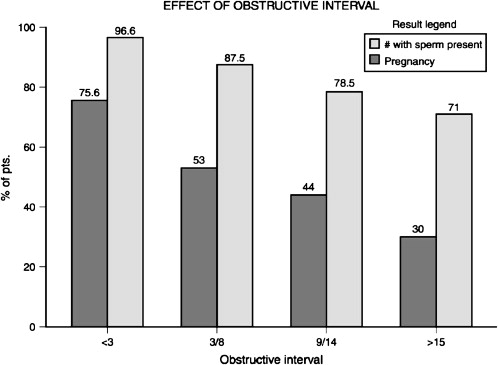
The impact of increasing obstructive interval on the success of vasectomy reversal was first reported by Silber. Although Silber reported that there was a precipitous decrease in success 10 years after vasectomy, this tenet was initially challenged by the Vasovasostomy Study Group. This landmark work demonstrated that there is not a precipitous decline in success at any point of time after vasectomy, but, rather, a gradual downward trend ( Fig. 1 ). In contrast, a more recent study from Boorjian and colleagues demonstrated no change in patency rates (88%–91%), even 15 years after vasectomy. These investigators noted that the pregnancy rates declined precipitously 15 years after vasectomy, from 82% to 89%, to 44%; however, before 15 years they stayed the same, even when a more complicated VE was performed. The investigators attributed their higher overall success rates to newer reconstructive techniques and their higher VE success rates to routine use of VE in cases of intravasal azoospermia (unless there was clear, copious fluid). It is important to note that a pregnancy rate of 44% in patients 15 years after vasectomy is still higher than reported pregnancy rates of 20% to 37% per IVF-ICSI cycle. Kolettis and colleagues determined outcomes for vasectomy reversal after at least 10 years of obstruction. The patency/pregnancy rate for obstructive interval of 10 to 15, 16 to 19, and 20 or more years was 74%/40%, 87%/36%, and 75%/27%, respectively. When compared to IVF-ICSI rates contemporaneous to this article (25% per initiated cycle in 2002), vasectomy reversal still yielded higher success rates.
Currently, pregnancy rates are used to compare success between IVF-ICSI and vasectomy reversal. Malizia and colleagues proposed cumulative live-birth rates over six cycles of IVF as a more appropriate measure of success because it represents achievement of the ultimate goal, the birth of a live child, after completed treatment. In their series of 6,164 patients undergoing 14,248 cycles, they demonstrated overall cumulative live-birth rates between 51% and 72% that was age-dependent (65%–86% in females <40 years old and 23%–42% in females >39 years old). Note that these success rates are for IVF overall, and are not specific to cases that used ICSI. Future discussion of cumulative live-birth rates as an outcome should compare rates specific to IVF-ICSI after sperm extraction and live-birth rates at any point in time after a vasectomy reversal.
In addition to its adverse effect on success of VV, increasing obstructive interval is also associated with an increased incidence of epididymal obstruction and the resultant need for VE. Although Boorjian and colleagues reported a 25% overall incidence of VE in their series, with no significant difference in use according to obstructive interval, Fuchs and Burt reported that 62% of patients with an obstructive interval 15 years or more required a VE for repair. Parekattil and colleagues designed a mathematical computer model based on obstructive interval and patient age to detect the need for a VE. This model was 100% sensitive and 58.8% specific with an area under the receiver-operating curve of 0.8. This model was subsequently validated to have 84% sensitivity and 58% specificity in a total of 345 patients at seven institutions. These studies highlight a clear relationship between obstructive interval and epididymal obstruction requiring a more complicated and less successful VE for repair.
Prior Fertility
Nearly all patients undergoing vasectomy reversal have a history of having previously fathered children or impregnated a partner. Although a history of fertility does not ensure normal spermatogenesis, the absence of previous fertility should raise concern. The vasectomy patient without prior fertility should undergo the standard endocrinologic infertility evaluation; however, it should be noted that the incidence of clinically significant endocrinopathies in infertile men is low (1.7%). Routine endocrinologic evaluation is not generally required in the individual with normal testicular size, consistency, and history of fertility prior to vasectomy.
Prior fertility in the female partner may provide additional useful information. There is a statistically significant difference between pregnancy rates after vasectomy reversal for patients whose current spouse was previously pregnant (57%) and those whose current spouse had not been previously pregnant (49%).
Prior Inguinal Surgery
Inguinal surgery, usually a pediatric hernia repair or a hernia repair with mesh, may result in a second point of vasal obstruction. The true prevalence of vasal obstruction from inguinal surgery is not known; however, in a multi-institutional report, 14 men were found to have vasal obstruction after hernia repair with mesh: 9 had bilateral obstruction and 5 had unilateral obstruction with contralateral testis atrophy or epididymal obstruction. The potential significance of this should be reviewed with the patient before reconstruction is attempted. Repair of obstruction in the inguinal canal or retroperitoneum can be technically demanding. Laparoscopy has been used for retrieval and mobilization of a retroperitoneal vas deferens in order to permit a tension-free, patent anastomosis in a case of extensive mesh-induced fibrosis of the inguinal vas deferens after herniorrhaphy. Furthermore, the need to complete two anastomoses on the same vas may result in a devascularized segment and technical failure.
Lizza and colleagues reviewed the records of 11 patients undergoing transseptal-crossed VV for obstructive azoospermia resulting from unilateral vasal obstruction and damage to the contralateral testis. They reported 50% patency rates and 25% pregnancy rates. Sabanegh and Thomas reported similar results in 10 patients undergoing transseptal-crossed VE. These data highlight the fact that more complex reconstruction is associated with lower success rates, and these issues should be discussed with any patient with a history of prior inguinal surgery.
Prior Vasectomy Reversal
Repeat vasectomy reversal is a valid option after failed initial reversal. Hernandez and Sabanegh performed a retrospective review of 41 men (38 had one previous reversal and 3 had multiple previous reversals) who underwent repeat vasectomy reversal. This group overall had a patency rate of 79% and a pregnancy rate of 31%. The only statistically significant predictor for successful pregnancy was a history of conception with the current partner. Pasquallotto and colleagues reviewed 18 patients who underwent repeat VE. The overall patency rate was 66.7%. Patency rates varied according to the level of anastomosis: 66.7% in the caput, 62.5% in the corpus, and 100% in the cauda. Each of these studies indicates that failure of prior reconstruction is not a contraindication to reconstructive procedures. However, the lower pregnancy rates after VE should be discussed with the patient.
Same Partner
Outcomes of vasectomy reversal in men with the same female partners are better than those for men with new partners. The Vasovasostomy Study Group first described this relationship ( Table 1 ). Chan and Goldstein confirmed this higher success rate in a subgroup of 27 men undergoing vasectomy reversal who had the same partner as before their vasectomy. They achieved a patency rate of 100% and a pregnancy rate of 86%. Interestingly, the live-birth rate in couples with the death of a child was 100%. Chan and Goldstein proposed previous proven fecundity as a couple, shorter obstructive interval, and stronger emotional dedication to having a child as possible reasons for higher success rates in men with same female partners.
| Effect of Indication on Fertility After Vasovasostomy | |
|---|---|
| Indication | No. Pregnant/Total in Group (%) |
| Divorce | 303/612 (50) |
| Death of child/same partner | 16/21 (76) |
| Other | 87/154 (57) |
Partner Age
As with any infertility intervention, the age of the female partner is an important factor in assessing the appropriateness of the intervention. Hinz and colleagues, in a retrospective analysis of 212 patients undergoing vasectomy reversal, identified age of female partner greater than 40 years as a predictor for lower pregnancy rates compared to those 30 to 39 years or less than 30 years ( P = 0.014 univariate and P = 0.010 multivariate). Gerrard and colleagues described patency/pregnancy rates for patients with female partners aged 20 to 24, 25 to 29, 30 to 34, 35 to 39, and greater than 40 as 90%/67%, 89%/52%, 90%/57%, 86%/54%, and 83%/14%, respectively. The pregnancy rate for patients with female partners aged greater than 40 years was 14%, compared to 56% for those with female partners aged less than 40 years. These two studies indicate a precipitous drop in pregnancy rates when the female partner is greater than 40 years old.
IVF-ICSI is also greatly influenced by the age of the female partner. Reported overall pregnancy rates for IVF-ICSI is 36.9% in women less than 35 years old, compared to 10.7% in women greater than 40 years old. IVF pregnancy rates in couples with only male-factor infertility are 44.7% in women less than 35 years old and 20.2% in women greater than 40 years old, indicating a detrimental effect of advanced partner age. Fuchs and Burt found a similar decline in pregnancy rates with advanced partner age that was seen in Gerrard and colleagues’s study. They found pregnancy rates of 64% for those with female partners aged less than 30 years of age and pregnancy rates of 28% for those with female partners greater than 40 years of age. Their data suggest slightly better pregnancy rates with vasectomy reversal (28%) when compared to IVF-ICSI for only male-factor inferility (20.2%) in this subgroup of couples with females aged greater than 40 years.
Antisperm Antibodies
Although discussed as a factor that may affect successful outcome, assessment of antisperm antibodies (ASA) is not generally performed prior to proceeding with a vasectomy reversal.
Meinertz and colleagues, in an effort to suggest the importance of ASA testing before vasectomy reversal, reported on 216 men who underwent VV and were subsequently tested with the mixed antiglobulin reaction for IgA and IgG specific to ASA bound to the sperm membrane. Free ASA in serum and seminal plasma were analyzed with the gelatin agglutination test and the tray agglutination test. In a subgroup with a pure IgG response, the rate of conception was 85.7%. In this group, only 42.9% of men who also had IgA on the sperm achieved pregnancy. When 100% of the sperm were covered with IgA, the pregnancy rate decreased to 21.7%. The combination of IgA on all sperm and a serum titer of greater than 255 was associated with a pregnancy rate of 0.
Carbone and colleagues published a study of 14 patients with partial obstruction (epididymal fullness) and ASA who had previously undergone vasectomy reversal. All patients had positive ASA status as defined as greater than 20% binding on indirect immunobead assay testing. After repeat vasectomy reversal without treatment of the ASA, the pregnancy rate was 50%. Sperm motility increased from 4.4% to 52.3%, and sperm concentration doubled. This suggests the reason for failure of the first vasectomy reversal was technical and not from ASA. The investigators concluded that ASA status is not a significant factor in failed VVs.
ASA form in the vast majority of individuals subjected to vasectomy. This fact, in conjunction with the fact that the majority of men will conceive after a technically successful vasectomy reversal, indicates the inability of ASA testing to predict successful vasectomy reversal. Therefore, determination of ASA status before attempted reversal is, in general, not recommended, as it will not affect the management of the individual patient.
Intraoperative factors
Surgeon Skill
Microsurgical reconstruction emphasizes technical skill and expertise. Outcomes improve with experience and refinement of technique. This was demonstrated in the fourfold greater success of VVs performed between 1994 and 1999, compared to those performed between 1980 and 1984, in a series from Holman and colleagues.
VEs are technically more demanding, and some urologists offer only VV for vasectomy reversal. Chawla and colleagues examined 22 cases of repeat vasectomy reversal after failed VV. Upon exploration, they found that 48% of the men had epididymal obstruction as the etiology for their initial failure. All surgeons offering vasectomy reversals should be able to offer VE if required, based on intraoperative findings.
There have been many attempts to train surgeons in new techniques using formal laboratory experiences. The authors performed a survey to assess the success of a group of urologists who had participated in a microsurgery course compared to those who had not (Nagler HM, Belker AM, unpublished data, 1997). Those surgeons who performed microsurgical VV without practice had a 53% patency rate, compared with an 89% patency rate for those surgeons who practiced their microsurgical skills in a laboratory before employing them clinically. This survey demonstrated the need to practice microsurgery in the laboratory before conducting it in a clinical setting.
Intravasal Fluid
The characteristics of the intravasal fluid and the presence of sperm in the fluid from the testicular vas deferens affect the likelihood of successful vasectomy reversal. Of patients with copious, clear fluid and motile intravasal sperm, 94% had a return of sperm to the ejaculate, compared with 60% of those with no sperm in the vasal fluid. The pregnancy rates for these two groups were 63% and 31%, respectively.
The decision to proceed with VV or to convert to VE is based on intraoperative inspection of the intravasal fluid, epididymal findings, the patient’s desires based on preoperative consultation, history of prior attempted VV, and the urologist’s skills. Despite the widely held dogma based upon prior reports, Sharlip reported a patency rate of 80% for patients without intravasal fluid at the time of VV. Nevertheless, most urologists believe that VV should be performed only if fluid containing whole sperm or sperm parts is encountered. Sigman reported excellent patency rates of 95%, 100%, and 100% for patients with sperm heads, sperm with short tails, and whole sperm, respectively. This study answered an often debated issue and now enables the urologist to perform the technically more successful procedure with the confidence that the results will be comparable for each of these observed findings. However, Kolettis and colleagues demonstrated a patency/pregnancy rate of 76%/35% when only sperm parts were encountered. The patency rate improved to 84% if cases with an occasional sperm head were excluded. This success rate is not as good as when complete sperm are encountered, but it is at least as good as most urologists’ experience with VE. VV is indicated when only sperm parts are encountered, but the urologist should consider VE if only an occasional sperm head is encountered.
If clear or copious fluid is encountered without sperm in the first-time reversal patient with an obstructive interval less than 11 years, VV may also be performed. Kolettis and colleagues reported a patency/pregnancy rate of 80%/38% in this subgroup. However, after the obstructive interval exceeds 11 years, VE is recommended.
VE is indicated if intravasal fluid is absent or if it is a thick, inspissated, toothpaste-like fluid. The epididymis should be examined (not explored) when there is thick fluid without sperm or when no fluid is observed. If a clear epididymal obstruction is encountered, VE is generally indicated.
Testicular Remnant Length
Witt and colleagues reported a correlation between the length of the postvasectomy testicular vasal remnant and the intravasal fluid characteristics: the longer the segment, the better the intravasal fluid. They showed that 94% of patients with a testicular remnant greater than 2.7 cm had whole sperm in the intravasal fluid. This observation has not been confirmed by other investigators, presumably because of the subjective nature of the measurement relative to the convoluted portion of the vas and that the length only predicted the intraoperative vasal findings. Preoperatively, one is unable to accurately assess the vasal remnant.
Sperm Granulomas
Sperm granulomas are discovered microscopically between 10% and 30% of the time in men undergoing vasectomy reversal. It is probable that, given sufficient time, all men will develop sperm granulomas at the vasectomy site, the epididymis, or the rete testis. Although sperm granulomas presumably allow the efferent ductules to vent into surrounding tissues, thus allowing the release of pressure that may protect the epididymis from tubule rupture or dysfunction, there was no difference in the technical or functional results achieved in patients with or without the presence of sperm granulomas. Sperm granulomas have been associated with better grades of sperm quality in the intraoperative vas; however, the Vasovasostomy Study Group found that a sperm granuloma at the site was not associated with successful repair. Patency/pregnancy rates were 96%/63% when a sperm granuloma was present bilaterally, and they were 85%/51% when it was absent bilaterally. These differences were not statistically significant. Boorjian and colleagues also could not demonstrate a statistically significant difference. However, Bolduc and colleagues found an odds ratio (95% confidence interval) of 2.4 (1.3–4.4) and statistical significance (0.004) in favor of patients with sperm granulomas. More studies are required to evaluate the relationship between the presence of sperm granulomas and the rates of success.
Vasectomy Site and Length
The site of vasectomy may result in a greater technical challenge for repair if it is in the convoluted portion, as opposed to the straight portion, of the vas deferens. In their single surgeon series, Patel and Sigman found patency rates of 98.1% and 97.3% for convoluted VV and straight VV, respectively, and this difference was not statistically significant. They conclude that although convoluted VV is considered technically more challenging, technical success is comparable with straight VV. However, this finding reflects only that single urologist’s skill level and not that of all urologists performing microsurgical reconstruction.
Although not studied, when there is a long segment of vas absent from an “aggressive” vasectomy, reversal is technically more demanding and may result in tension on the anastomosis. A longer absent segment may also necessitate more vigorous mobilization of the vas with greater potential for devascularization and subsequent fibrosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






