Chapter 75B Esophageal varices
Acute management of portal hypertension
Overview
The most important aspect of care in patients with suspected variceal or other portal hypertensive hemorrhage is adequate resuscitation while directed diagnostic maneuvers and therapies are being coordinated. Although this chapter focuses on acute esophageal variceal bleeding, many of the principles and therapies may apply to other sources of portal hypertensive bleeding. Acute variceal hemorrhage is associated with a 15% to 20% mortality rate at 6 weeks (Abraldes et al, 2008; Villanueva et al, 2006). Although evidence supports the use of endoscopy for diagnosis and treatment, insufficient resuscitation can lead to significant periprocedural complications. Appropriate pharmacotherapy has proven equally effective in controlling variceal hemorrhage in some studies. More importantly, pharmacotherapy can be started immediately in any hospital, regardless of endoscopic staff availability.
The morbidity of patients who present with acute variceal hemorrhage is strongly influenced by their reason for recent decompensation. In most instances, early resuscitative measures followed by pharmacotherapy and endoscopy allow improvement in hepatic synthetic function and provide time to address more definitively the overall management of the patient and any recurrent bleeding. In patients with life-threatening exsanguination, balloon tamponade is a useful maneuver until the patient is stable enough for endoscopy. In patients with bleeding refractory to pharmacotherapy and endoscopic intervention, transjugular intrahepatic portosystemic shunting (TIPS) generally is the next option for short- and mid-term stabilization (see Chapter 76E). Shunt operations (see Chapters 76A through 76D) have traditionally been reserved for individuals for whom transplantation and TIPS are not an option but who have a reasonable chance of operative survival.
Emergency Management
Before any diagnostic maneuvers can be performed (e.g., endoscopy), support of the circulating blood volume with adequate resuscitation is imperative. Isotonic crystalloid is the first replacement fluid of choice, but typed and cross-matched blood products are needed for the majority of patients with variceal hemorrhage. Evidence supports the use of colloids over crystalloid and packed red blood cells with the end points of optimal hemodynamics and oxygen transport (Shoemaker, 1987). Maintenance of hemoglobin values of approximately 8 g/dL are recommended; higher blood volumes are associated with increased portal pressures, higher rebleeding rates, and higher mortality rates. Other measures of the adequacy of resuscitation include systolic blood pressures of 90 to 100 mm Hg, central venous pressures of 9 to 16 mm Hg, and adequate urine output; pulmonary artery occlusion catheters may be a useful adjunct in some patients. When the adjusted prothrombin time is prolonged by more than 3 to 4 seconds, fresh frozen plasma is likewise recommended. Recombinant Factor VIIa has not been shown to benefit patients with cirrhosis with gastrointestinal (GI) hemorrhage over standard therapy (Bosch et al, 2008). For patients with significant bleeding or decreased consciousness, endotracheal intubation should be expedited.
Complications from variceal bleeding contribute to overall morbidity and mortality related to chronic liver disease. Preventing these complications can therefore have a significant impact on the short-term mortality rate associated with variceal bleeding. Antibiotic prophylaxis has been shown to decrease variceal rebleeding and bacterial infection (Bernard et al, 1999; Fernandez et al, 2006). Systematic reviews have shown decreased mortality rates with antibiotic prophylaxis in the setting of GI bleeding (Soares-Weiser et al, 2002). Consensus agreement supports norfloxacin use for 7 days (400 mg bid) in patients with two or more of the following: malnutrition, ascites, encephalopathy, or serum bilirubin level greater than 3 mg/dL. Ceftriaxone had better outcomes than norfloxacin when given intravenously in areas with known quinolone resistance according to randomized, controlled data (Fernandez et al, 2006). It may be that other antibiotics with similar spectra of activity would provide satisfactory substitutes in the event of problems with patient tolerance, local antibiotic availability, or susceptibility issues.
Controlling Acute Hemorrhage: Pharmacologic Agents
Coupling pharmacologic measures and endoscopy with the initiation of preventative measures provides the most sustainable results when attempting to control acute GI hemorrhage in patients with advanced liver disease. The specific drugs are widely available, generally safe, and can be initiated as soon as variceal hemorrhage is suspected. Drugs such as somatostatin or its analogues, octreotide and vapreotide, work by constricting arterial and thus venous splanchnic blood flow, thereby reducing portal hypertension acutely. In randomized controlled trials comparing these vasoactive agents with others, including vasopressin and terlipressin, no significant differences in bleeding control were reported, although vasopressin was associated with more adverse events (Banares et al, 2002; Villaneuva et al, 2006). Currently, an initial bolus dose of octreotide 50 µg IV followed by 50 µg/h is recommended. Duration usually extends from 72 hours to 5 days, and recurrent bleeding should be treated with an additional bolus dose. Only octreotide and vasopressin are currently available in the United States.
Controlling Acute Hemorrhage: Endoscopic Therapy
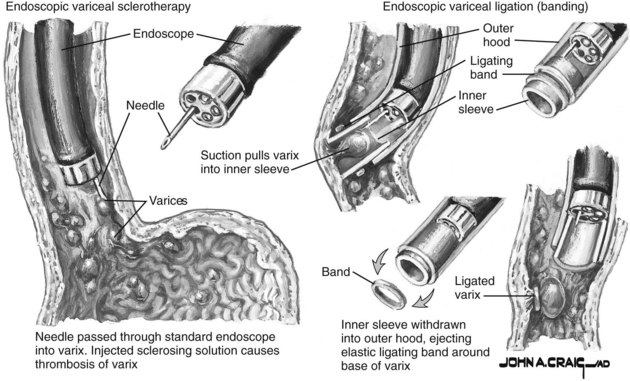
The two main endoscopic therapeutic choices are endoscopic variceal ligation (EVL) and sclerotherapy. The strong preference remains for EVL, given its superior control of bleeding and decreases reported in rebleeding rates, mortality rates, and esophageal complications. Both techniques require a skilled endoscopist; however, when both groups were treated with somatostatin concomitantly, failure rates of EVL were estimated at 10% compared with 24% of sclerotherapy patients. Failure to control acute bleeding is also significantly more frequent in the sclerotherapy group (Villanueva et al, 2006).
After adequate sedation and diagnostic endoscopy, EVL should commence. The decision regarding whether to start with a standard 2.8-mm gastroscope versus a therapeutic endoscope is practitioner dependent given the potential for clot removal by irrigation. Once a variceal source has been identified, the endoscope should be removed and a multibanding kit should be applied with a standard gastroscope. Bands should be applied to any vessels actively spurting blood or displaying stigmata of recent hemorrhage, such as red wale marks, white nipples, and/or adherent blood clots. Other vessels should then be ligated, starting as close as possible to the esophagogastric junction. The varix is drawn into the ligator by applying suction, and a band is then applied as shown in Figure 75B.1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree