Fig. 12.1
A straight soft distal attachment (Olympus Medical Systems, Tokyo, Japan)
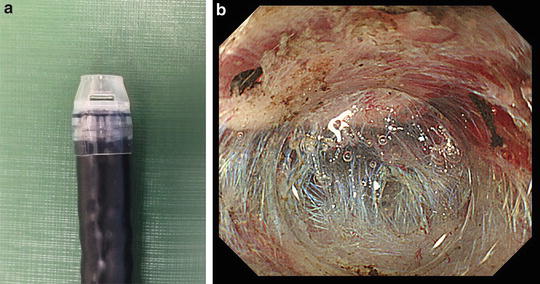
Fig. 12.2
A short ST hood (small-caliber tip hood) (Fujifilm, Tokyo, Japan)
Knives
Short needle type knives, such as the Dual Knife (Olympus Medical Systems, Tokyo, Japan, Fig. 12.3a) and the Flush Knife (Fujifilm, Tokyo, Japan, Fig. 12.3b), are the most popular devices for colorectal ESD. The Dual Knife is the most maneuverable device, owing to its soft and flexible nature, and it is ideal for colonic ESD [11]. The Flush Knife has water flushing function through its sheath, thus it is able to give additional submucosal fluid cushion during the procedure [12]. Both of the knives have a small disk or ball at the tip of the needle that can get hold of the target tissue.
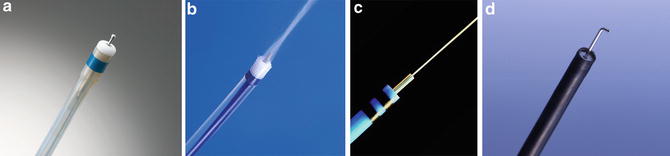
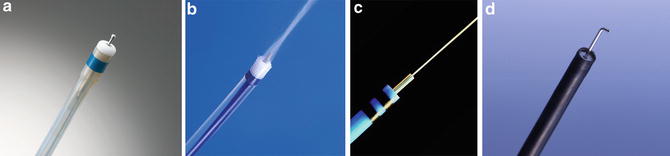
Fig. 12.3
Various ESD knifes suitable for colorectal ESD
The Hybrid Knife (ERBE, Tubingen, Germany, Fig. 12.3c) is also a length adjustable short needle knife. The particular specification of this knife is the pressure-controlled water jet function through its needle. It can inject some solution without using an injection needle, even through the mucosa, by setting appropriate water pressure [13]. It is a promising technology for ESD; however, precise control of the knife within a narrow space is rather difficult due to its rigidity and the relatively thick knife tip.
Many standard colorectal ESD procedures can be smoothly done with the above-mentioned short needle type knives, but in the case of a difficult situation, one had better to switch to the Hook knife (Olympus Medical Systems, Tokyo, Japan, Fig. 12.3d). It has a rotatable small hook part at the tip. One can hook and pull the target tissue with this hook before cutting it, which aids safety [14].
Hemostatic Forceps and Endoclips
Before starting ESD, it is necessary to have readily available hemostatic forceps (Pentax Co. Ltd. and Olympus Medical Systems, Tokyo, Japan) and rotatable clip fixing devices (Olympus Medical Systems, Tokyo, Japan, Boston Scientific, Boston, U.S.A.) to use anytime for bleeding and perforation. The hemostatic forceps must not be confused with a hot biopsy forceps, the latter being much larger and not pointed at the tip. The use of hot biopsy forceps is not recommended for colonic procedures, mainly for fear of a delayed perforation owing to focal over-coagulation.
Injection Solutions
Normal saline is the most popular injection fluid for conventional EMR. However, the mucosal protrusion created with the injection of normal saline does not last long enough to provide sufficient time for submucosal dissection [15]. In order to create a long-lasting submucosal fluid cushion, several other fluids have been used for ESD; among those, Glyceol solution (consisted of 10 % glycerin, 5 % fructose, and 0.9 % sodium chloride) is the most popular solution for the standard procedure. And a much more viscous agent, such as sodium hyaluronate [15–17], is preferable for larger and more difficult lesions. A sodium hyaluronate solution at a concentration of 0.4 % (MucoUp, Seikagaku Kougyo Co., Tokyo, Japan; derived from rooster comb) can create a prominent, long-lasting effect and is approved in Japan for use in the endoscopic resection of colorectal lesions [18]. A mixture with a small amount of added epinephrine is effective for the control of bleeding during the procedure. A further additive, indigocarmine dye, is useful for aiding clear visualization of the submucosal layer and visual differentiation from muscle.
Carbon Dioxide Insufflation
The safety and efficacy of carbon dioxide (CO2) insufflation during ESD with the patient under conscious sedation and deep sedation have been reported [19–21]. Since the procedure time of ESD is much longer than other ordinary endoscopic procedures, it is mandatory to use CO2 insufflation for ESD procedure. Moreover, even in the event of perforation, with CO2 insufflation there is enough time to close the perforation with clip placement because leaked CO2 into the abdominal cavity and/or retroperitoneal space is quickly absorbed.
Strategy for Colorectal ESD
The demarcation of colonic lesions is usually quite obvious and clear, so initial marking is not necessary for colorectal ESD (Fig. 12.4a). And it is very important to make a strategy for the procedure in order to perform colorectal ESD successfully.
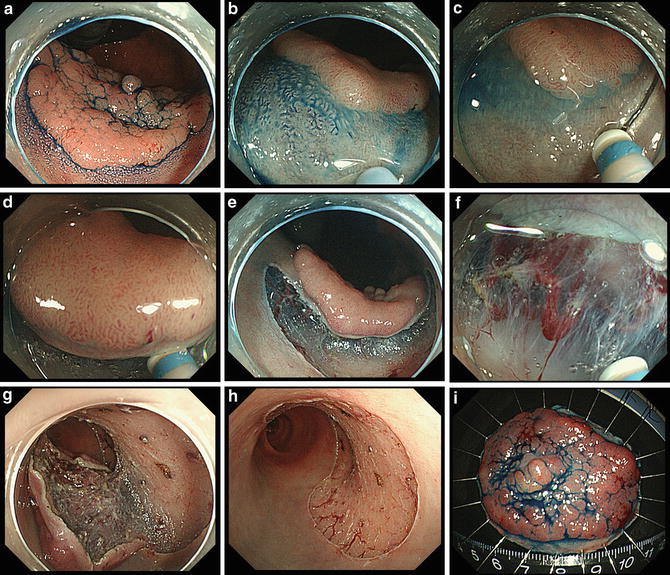
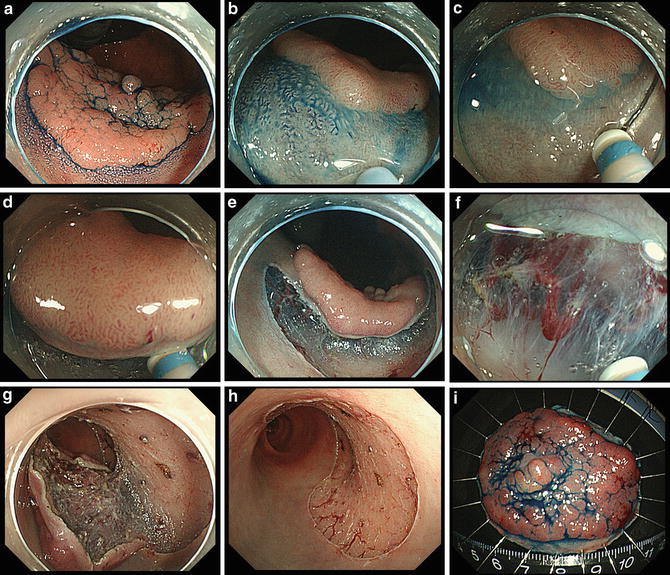
Fig. 12.4
Standard colonic ESD procedure for a mid-sized LST-G. The lesion was completely removed in an en bloc fashion. Resected specimen revealed a well-differentiated tubular adenocarcinoma with an adenomatous component; 46 × 38 mm, pSM (0.8 mm), INFa, ly0, v0, pHM0, pVM0
One usually starts the procedure at the proximal side of the lesion, along the uppermost part (in terms of gravity) (Fig. 12.4b). If it is possible to keep the endoscope in a retroflexed view, it is better to start the procedure in this position since the endoscope is more stable and the target lesion is more easily approximated to the working channel (Fig. 12.4c). Circumferential mucosal incision is not recommended, since injected solution can easily leak out from the incised area. Submucosal dissection should be started immediately after partial mucosal incision, tracing along the inner edge of the incision line (Fig. 12.4d) until a submucosal pocket is created (Fig. 12.4e). It is quite important to get into the submucosal space with the transparent hood after initial submucosal dissection; this makes it easier to continue submucosal dissection with a stable condition under good visualization of the submucosa (Fig. 12.4f). When it is necessary, change the patient position in order to open the submucosal space widely by utilizing gravity (Fig. 12.4g). After progressing through submucosal dissection of more than half of the lesion from the upper side, reverse the position of the patient so that the remaining side becomes easier to dissect for the rest of the procedure. Keeping the submucosal fluid cushion sufficient by additional injection when necessary, any remaining incision and dissection can be safely done. Check the resected area and coagulate the exposed blood vessels carefully (Fig. 12.4h). Stretch the resected specimen on a cork board with pins before submitting it to the pathologist (Fig. 12.4i).
Difficult Situations for Colorectal ESD
Good maneuverability of the endoscope is the most important factor for a successful ESD procedure. There are some factors that can cause poor maneuverability of the endoscope. A long and strongly inflectional colon or severe adhesion of the colon due to previous surgery or some other diseases are major reasons for poor maneuverability of the endoscope. In these particular situation, ESD becomes almost impossible to do and even insertion of the endoscope becomes extremely tough. However, using a balloon assisted endoscope system, there is still some chance to perform ESD. Currently, a 152 cm universal double balloon endoscope (Fuji EI-530B, Fig. 12.5, Fujifilm Tokyo, Japan), which is a suitable length for standard ESD instruments, is commercially available. The majority of difficult situations caused by poor maneuverability of the endoscope can be under better control with this system. If one cannot get better control with the balloon-assisted endoscope system, one had better not attempt ESD.


Fig. 12.5
Universal double balloon endoscope (Fujifilm, EI-530B, Tokyo, Japan)
Other difficult situations usually arise due to the nature of the lesions themselves. Large lesions crossing the haustral hold (Fig. 12.6), large lesions invading the anal canal (Fig. 12.7) or those at the ileocecal valve (Fig. 12.8) are very difficult situations for ESD. In order to dissect the submucosal tissue smoothly, one has to open the submucosal space by utilizing gravity and changing patient position. In the case of lesions with anal canal invasion, it is necessary to use some local anesthesia, such as 1 % lidocaine, when the operator cuts tissue within the anal canal. And in the case of lesions with ileocecal valve involvement, initial injection and incision should be started from the ileal side, otherwise it becomes almost impossible to cut the ileal side at later stages.
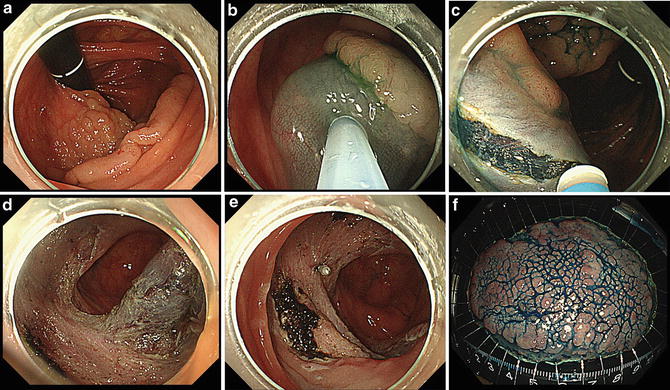
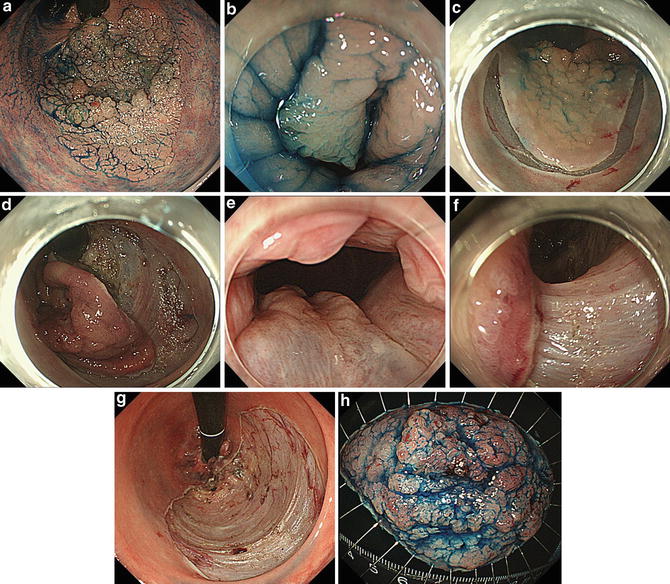
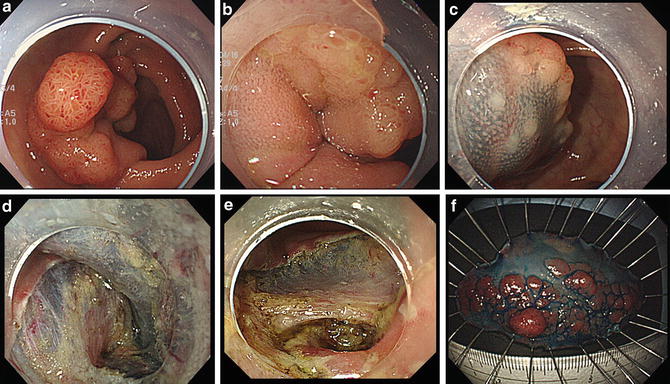
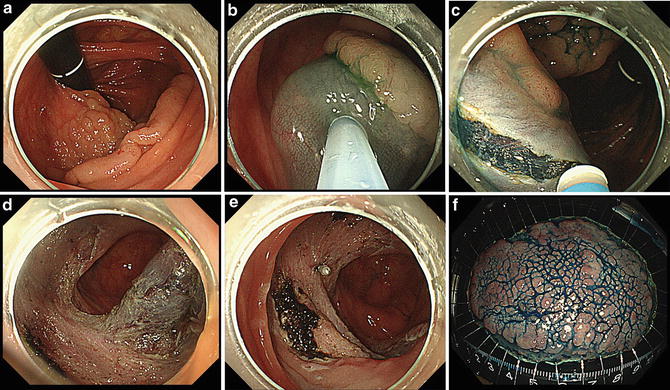
Fig. 12.6
A large LST-G located at ascending colon, straddling two folds. Resected specimen revealed a well-differentiated tubular adenocarcinoma, 78 × 56 mm, pM, ly0, v0, pHM0, pVM0
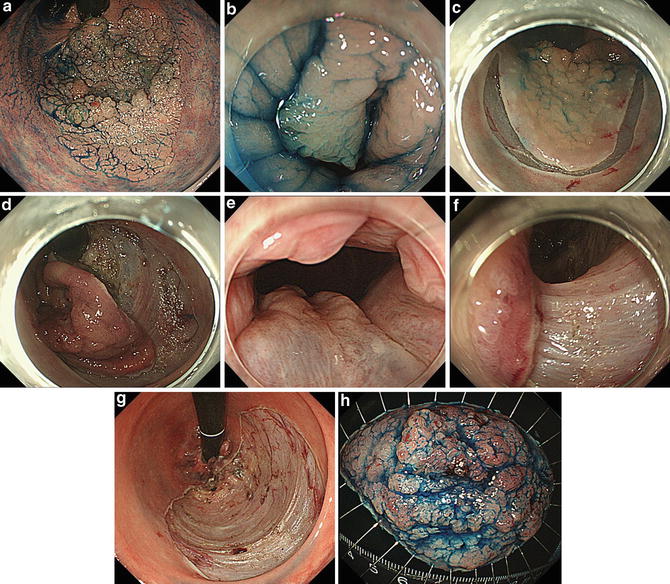
Fig. 12.7
A large LST-G invading to the anal canal. ESD was performed using 1 % lidocaine at the anal canal. Resected specimen revealed well-differentiated tubular adenocarcinoma, 65 × 48 mm, pM, ly0, v0, pHM0, pVM0
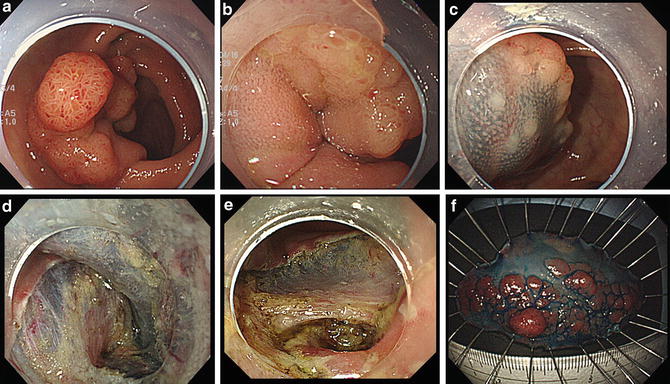
Fig. 12.8




A large LST-G involving the ileo-cecal valve. Complete resection was achieved and pathological diagnosis was a tubular adenoma with severe atypia, 60 × 30 mm, pHM0, pVM0
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








