CHAPTER 61 Endoscopic Treatment of Pancreatic Disease
EARLY ACUTE PANCREATITIS
When a patient presents with acute pancreatitis the role of endoscopy is limited to two situations: first, those patients with gallstone-induced pancreatitis (see Chapters 58 and 66) and second, to provide nutritional support via enteric feeding (see Chapter 5). Gallstone pancreatitis is caused by impaction of a stone within the common channel of the ampulla of Vater, usually transiently. ERCP and biliary sphincterotomy are used to improve the outcome of gallstone pancreatitis by removal of an impacted stone with relief of pancreatic ductal obstruction. Initial studies of patients with acute gallstone pancreatitis and choledocholithiasis used urgent (within 72 hours of admission) ERCP and sphincterotomy (if a stone was identified). An improved outcome was seen only in patients with clinically severe acute pancreatitis.1 Studies now suggest that the improved outcome following ERCP and sphincterotomy in gallstone pancreatitis results from reduced biliary sepsis rather than improvement in pancreatitis.2,3 A meta-analysis showed that early ERCP in patients with predicted mild or severe acute biliary pancreatitis without concomitant acute cholangitis did not significantly reduce overall complications and mortality.4 Similarly, results from a prospective randomized trial showed that ERCP and sphincterotomy could decrease morbidity in patients with gallstones pancreatitis and ampullary obstruction when the duration of obstruction did not exceed 28 hours.5 ERCP in patients with severe gallstone acute pancreatitis is best reserved for patients with suspected biliary obstruction, based on hyperbilirubinemia and evidence of clinical cholangitis because it is unlikely that the ampulla is obstructed in the presence of a normal serum bilirubin.6,7 Other imaging modalities in patients with severe biliary pancreatitis such as EUS and MRCP can help select patients for ERCP when bile duct stones are identified.8,9 If bile duct stones are not identified during ERCP performed for acute gallstone pancreatitis, there are no data to guide whether an empirical biliary sphincterotomy should be performed. However, sphincterotomy can reduce the risk of recurrent acute pancreatitis and cholangitis prior to cholecystectomy.10
Evidence supports enteral feeding for patients with severe acute pancreatitis based on randomized prospective studies comparing total parenteral nutrition with enteral feeding (through a nasoenteric feeding tube placed beyond the ligament of Treitz) instituted within 48 hours of illness onset.11 Lower cost and fewer infectious complications are seen with enteral feeding (see Chapter 5). There are a variety of endoscopic techniques for placing nasojejunal feeding tubes in the setting of acute pancreatitis12 including transnasal endoscopy.13
LOCAL COMPLICATIONS OF ACUTE PANCREATITIS
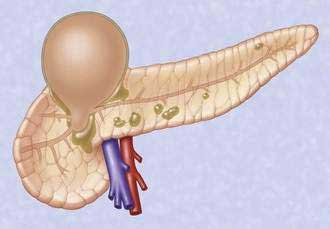
Acute fluid collections, acute pancreatic pseudocysts, organized pancreatic necrosis, and pancreatic abscesses may arise as a result of acute pancreatitis.14 Acute fluid collections form early in the course of acute pancreatitis and usually resolve without therapy. Acute pseudocysts arise as a sequela of acute pancreatitis, require at least four weeks to form, and are devoid of significant solid debris. Acute pancreatic pseudocysts usually form as a result of limited pancreatic necrosis that produces a pancreatic ductal leak (Fig. 61-1). Alternatively, areas of pancreatic and peripancreatic fat necrosis may liquefy over time and become a pseudocyst.15 Despite the requirement of at least four weeks for a pseudocyst to form, it is important to realize that some patients with significant early acute pancreatic necrosis (>30%) may evolve the pancreatic and peripancreatic necrosis into a collection that radiographically resembles a pseudocyst.16 These collections contain significant solid debris, and endoscopic treatment of them using typical pseudocyst drainage methods often results in infectious complications because of contamination and inadequate removal of solid debris.17,18
ACUTE PANCREATIC PSEUDOCYST
Drainage of an acute pseudocyst is indicated for treatment of symptomatic pseudocysts that may or may not be infected19 and for progressive enlargement on imaging studies. Symptoms and signs from an acute pseudocyst include abdominal pain, often exacerbated by eating, weight loss, gastric outlet obstruction, obstructive jaundice, and pancreatic duct leakage, which may result in pancreatic ascites or pancreatic fistulae.20 Pseudocysts may be drained through the papilla (transpapillary), through the gastric or duodenal wall (transmurally), or by using a combination of the two.
Transpapillary Drainage
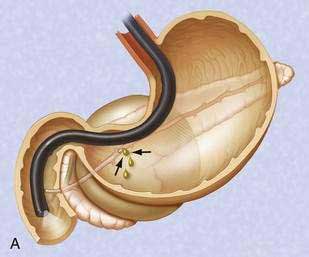
If the pseudocyst communicates with the main pancreatic duct, placement of a pancreatic duct stent with or without pancreatic sphincterotomy is effective, especially for smaller pseudocysts (<5 to 6 cm) that are not otherwise approachable transmurally.21 The proximal end of the stent (toward the pancreatic tail) may directly enter the pseudocyst, bridge the area of leak into the pancreatic duct upstream from the leak, or lie completely downstream to the leak. Bridging the leak is the preferred approach because it restores ductal continuity and appears to be more effective (Fig. 61-2).22,23 Transpapillary drainage avoids bleeding or perforation that may occur with transmural drainage. However, pancreatic stents may induce scarring of the main pancreatic duct.24
Transmural Drainage
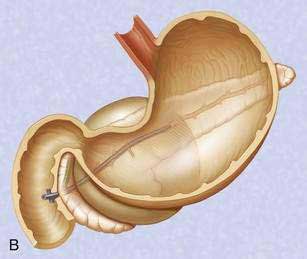
There is no standardized approach to transmural pseudocyst drainage. Transmural drainage is performed by entering the cyst using a needle without cautery or using a cautery device (e.g., needle knife). Some endoscopists believe EUS-guided drainage is mandatory prior to performing endoscopic transmural drainage to prevent bleeding and perforation.25 Although the superiority of EUS-guided versus non–EUS-guided drainage has not been demonstrated,26 there are increasing data to support its routine use during transmural drainage,26–28 especially when non–EUS-guided drainage fails.29 EUS-guided entry is successful in more than 95% of patients and with low complication rates.30–32 Non–EUS-guided entry also can be performed33 and, in the hands of experienced operators, successful transmural entry has been reported in 91 of 94 patients in lesions as small as 3 cm and without endoscopically visible extrinsic compression.34 Once the pseudocyst is successfully entered, the transmural tract is balloon dilated to 8 to 10 mm in diameter to allow placement of one or two 10-French stents (Fig. 61-3).35
Following uncomplicated attempted endoscopic drainage, a follow-up CT is obtained four to six weeks after the procedure. The internal stents are endoscopically removed after documented radiographic pseudocyst resolution. Success rates, recurrence rates, and complication rates of endoscopic drainage of pancreatic pseudocysts are variable, likely because of many reports included acute and chronic pseudocysts and pancreatic abscesses. In addition, some patients underwent transpapillary drainage and others underwent transmural drainage. Nonetheless, cumulatively successful drainage is achieved in approximately 75% to 90%, with complication rates of about 5% to 10% and pseudocyst recurrence rates of 5% to 20%.36,37
ORGANIZED PANCREATIC NECROSIS (WALLED-OFF PANCREATIC NECROSIS)
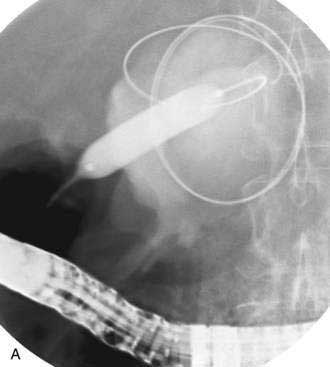
Pancreatic necrosis is nonviable pancreatic parenchyma, usually associated with peripancreatic fat necrosis. In the earliest form, this is detected on contrast-enhanced CT by demonstrating areas of nonenhancing pancreatic parenchyma. Pancreatic necrosis is frequently accompanied by major pancreatic ductal disruptions. Over the course of several weeks, the collection may continue to evolve and expand the initial area of necrosis and contains both liquid and solid debris (Fig. 61-4). The terms organized pancreatic necrosis20 and walled-off pancreatic necrosis (WOPN)38 have been used to differentiate this process from the early (acute phase) of pancreatic necrosis. The CT appearance of organized pancreatic necrosis may be mistaken as an acute pseudocyst.16
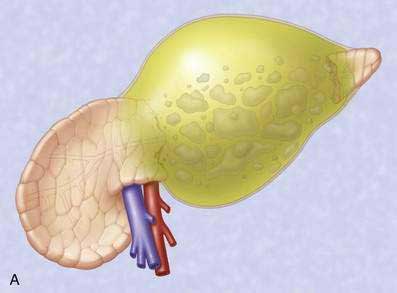

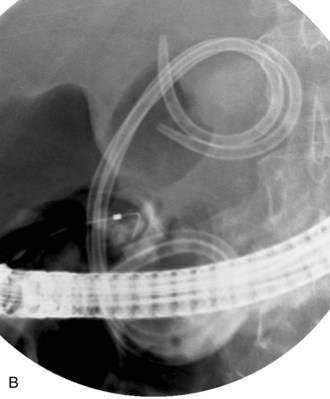
Figure 61-4. A, Illustration of walled-off (organized) pancreatic necrosis. B, Computed tomography scan of patient with organized pancreatic necrosis. Successful endoscopic therapy using direct necrosectomy was performed (see Fig. 61-5).
The indications for and timing of drainage of sterile WOPN are controversial. Endoscopic drainage cannot be performed until the process becomes organized, which usually occurs several weeks after onset of pancreatitis. Indications for drainage of sterile WOPN are refractory abdominal pain, gastric outlet obstruction or failure to thrive (continued systemic illness, anorexia, and weight loss) at four or more weeks after the onset of acute pancreatitis.38 Because endoscopic drainage of WOPN is more technically difficult, carries a higher rate of complications, and tends to involve more severely ill patients than patients with acute pseudocyst, the decision to endoscopically intervene when the process is sterile pancreatic necrosis must be carefully considered.39 Alternative management options to endoscopic drainage include nutritional support with parenteral or enteral jejunal feeding and nonendoscopic drainage methods such as percutaneous and surgical drainage. The management option selected is usually based on local expertise and severity of comorbid medical illnesses. Ideally, these patients are best managed by a multidisciplinary approach.
Infected necrosis is an indication for drainage. Percutaneous fine-needle aspiration may be required to determine the bacteriologic status prior to intervention.40
Because of the need to evacuate solid material, the endoscopic approach to drainage of WOPN differs from drainage of pseudocysts. In general, the transpapillary approach alone is not adequate because it does not allow removal of solid debris. Therefore, the transmural drainage approach is used. The endoscopic approach has evolved. Initially nasal irrigation tubes were placed of alongside transmurally placed stents in order to lavage the solid debris.41 Subsequent approaches used percutaneous endoscopic gastrostomy (PEG) tubes to provide a method of placing irrigation tubes into the necrotic cavity and avoid uncomfortable transnasal tubes.42,43
The most recent approach for removal of necrotic debris is to perform direct endoscopic debridement. This is performed by dilating the transmural tract with large-caliber balloons (up to 20 mm) and passing a forward-viewing endoscope through the tract directly into the necrotic cavity (Fig. 61-5).44,45 Snares, grasping forceps, and other accessories are then be used to remove solid debris. This approach has been shown in a retrospective study to be superior to the irrigation approach.46 Nevertheless, repeat procedures are often needed to re-dilate the transmural tract, to debride residual necrotic material, and to attempt to treat underlying pancreatic ductal disruptions in hopes of preventing a ductal disconnection.
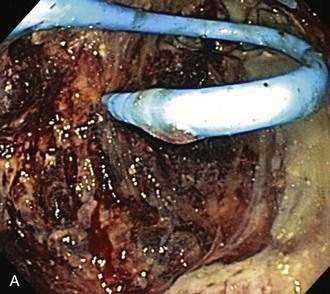

Figure 61-5. Direct endoscopic necrosectomy performed in the patient depicted in Figure 61-4. A, Endoscopic view from inside the necrotic cavity; an indwelling pigtail stent is seen with surrounding necrotic debris. B, Necrotic solid material being withdrawn from the cavity through the posterior gastric wall with a snare.
Drainage of pancreatic necrosis is associated with a higher complication rate and longer hospital stay.27,47 Patients with acute pseudocysts tend to have less severe ductal abnormalities and fewer recurrences.
PANCREATIC ABSCESS
When a broad definition of pancreatic abscess is taken to include infected pseudocysts or infected liquefied collections without significant solid debris (pancreatic necrosis), success rates following endoscopic drainage are high, although there are few series with small numbers of patient.47–49
COMPLICATIONS OF ENDOSCOPIC THERAPY OF PANCREATIC FLUID COLLECTIONS
Operator experience likely plays a role in the outcome following endoscopic drainage.50 Life-threatening bleeding or perforation may arise following attempted endoscopic drainage of pancreatic fluid collections. Infectious complications usually occur from inadequate drainage of fluid and solid debris. Infection can usually be managed by additional endoscopic procedures and placement of percutaneous drains. Endoscopic therapy followed by complications may adversely alter the surgical outcome as compared to patients undergoing primary surgical therapy.51,52