Bile duct stone management has greatly changed in the past 2 decades. Open surgical techniques have mostly been replaced by transoral endoscopic techniques. Routine common bile duct stones can be managed by standard biliary endoscopic sphincterotomy and extraction. Various advanced transoral techniques can also manage most difficult ductal stones. In skilled centers, laparoscopic ductal stone management has assumed a back-up role.
In Western countries, most stones in the common bile duct (CBD) result from passage of gallbladder stones into the CBD. Stones in the common duct are found in 8% to 18% of patients with symptomatic gallbladder stones. At least 3% to 10% of patients undergoing cholecystectomy have CBD stones. Patients with symptomatic bile duct stones are at high risk of experiencing further symptoms or complications if left untreated. Given the potential serious complications of bile duct stones, specific therapy generally is indicated regardless of symptoms.
Introduction of endoscopic retrograde cholangiopancreatography (ERCP) with biliary sphincterotomy in 1974 opened a new era in the nonsurgical treatment of CBD stones. Such endoscopic management is now the mainstay in the management of bile duct stones. Multiple supplemental techniques are now available.
This article discusses the current state of endoscopic treatment of extrahepatic bile duct stones. This includes conventional endoscopic management of CBD stones and alternative strategies for stones that are more difficult to remove. Gallstone pancreatitis, intrahepatic stones (mostly seen in Asians), and postliver transplant problems are not discussed.
Routine common bile duct stones
Stones less than 1 cm in diameter with normal terminal CBD/sphincter anatomy are considered routine because more than 85% can be managed by standard biliary endoscopic sphincterotomy (BES) and extraction ( Fig. 1 ).
Biliary endoscopic sphincterotomy
Enlargement of the biliary sphincter is necessary for luminal passage and endoscopic stone removal. This is mostly commonly done via electrocautery sphincterotomy. Routine pre-ERCP coagulation assessment is probably unnecessary unless there is history of liver disease or kidney disease, family history of bleeding disorder, or anticoagulation medicine use.
The procedure is performed with a sphincterotome, which consists of a Teflon catheter with a cautery wire exposed for a length of 20 to 35 mm near the tip. After deep bile duct cannulation is achieved, the sphincterotome is retracted until only 5 to 8 mm remain in the duct/papilla. The cutting wire of sphincterotome is then bowed so that it comes in greater contact with the roof of the papilla. The orientation of the cutting wire should be between the 11:30 and 12:30 positions to reduce the likelihood of retroperitoneal perforation. Applying intermittent bursts of diathermic current from the electrosurgical generator makes the incision through the sphincter. The length of the incision may range from 7 to 15 mm, depending on the size of the stone to be extracted and size of papilla. The combination of cutting current blended with coagulation current is most frequently used. Attempts to decrease postsphincterotomy pancreatitis by decreased coagulation current have resulted in more bleeding. One cautery option is use of a microprocessor-controlled system, which automatically alternates cutting and coagulation current by intrinsic software, the so-called ENDO CUT mode of the ERBE electrosurgical generator (ERBE Elektromedizin GmbH, Tubingen, Germany). An advantage of this method is a stepwise cutting action, which avoids a rapid uncontrolled incision. Additionally, it may also reduce the bleeding after BES. A large retrospective analysis suggested that the microprocessor-controlled BES is associated with a significantly lower frequency of intraprocedural bleeding but had no impact on clinically relevant postprocedure bleeding.
After a successful BES, 85% to 90% of CBD stones can be retrieved by a basket or balloon catheter. The choice between a basket or balloon catheter is largely one of personal preference and size of the stone to be extracted. The extractor basket provides greater mechanical forces than the balloon catheter and is preferable for stones larger than 8 mm. Endoscopists should be prepared to use a needle knife to remove the distally impacted CBD stone, which shows characteristic bulging papilla ( Fig. 2 ).
Most prospective series report an overall short-term complication rate for ERCP or sphincterotomy of approximately 4% to 10%. In a large, prospective US multicenter trial, the overall complication rate of BES was 9.8% in 2347 patients, including pancreatitis in 5.4%, bleeding in 2%, procedure-related cholangitis in 1%, cholecystitis in 0.5%, and perforation in 0.3%. In the subgroup of 1600 patients who had common duct stones, the overall complication rate was 8%.
Biliary endoscopic sphincterotomy
Enlargement of the biliary sphincter is necessary for luminal passage and endoscopic stone removal. This is mostly commonly done via electrocautery sphincterotomy. Routine pre-ERCP coagulation assessment is probably unnecessary unless there is history of liver disease or kidney disease, family history of bleeding disorder, or anticoagulation medicine use.
The procedure is performed with a sphincterotome, which consists of a Teflon catheter with a cautery wire exposed for a length of 20 to 35 mm near the tip. After deep bile duct cannulation is achieved, the sphincterotome is retracted until only 5 to 8 mm remain in the duct/papilla. The cutting wire of sphincterotome is then bowed so that it comes in greater contact with the roof of the papilla. The orientation of the cutting wire should be between the 11:30 and 12:30 positions to reduce the likelihood of retroperitoneal perforation. Applying intermittent bursts of diathermic current from the electrosurgical generator makes the incision through the sphincter. The length of the incision may range from 7 to 15 mm, depending on the size of the stone to be extracted and size of papilla. The combination of cutting current blended with coagulation current is most frequently used. Attempts to decrease postsphincterotomy pancreatitis by decreased coagulation current have resulted in more bleeding. One cautery option is use of a microprocessor-controlled system, which automatically alternates cutting and coagulation current by intrinsic software, the so-called ENDO CUT mode of the ERBE electrosurgical generator (ERBE Elektromedizin GmbH, Tubingen, Germany). An advantage of this method is a stepwise cutting action, which avoids a rapid uncontrolled incision. Additionally, it may also reduce the bleeding after BES. A large retrospective analysis suggested that the microprocessor-controlled BES is associated with a significantly lower frequency of intraprocedural bleeding but had no impact on clinically relevant postprocedure bleeding.
After a successful BES, 85% to 90% of CBD stones can be retrieved by a basket or balloon catheter. The choice between a basket or balloon catheter is largely one of personal preference and size of the stone to be extracted. The extractor basket provides greater mechanical forces than the balloon catheter and is preferable for stones larger than 8 mm. Endoscopists should be prepared to use a needle knife to remove the distally impacted CBD stone, which shows characteristic bulging papilla ( Fig. 2 ).
Most prospective series report an overall short-term complication rate for ERCP or sphincterotomy of approximately 4% to 10%. In a large, prospective US multicenter trial, the overall complication rate of BES was 9.8% in 2347 patients, including pancreatitis in 5.4%, bleeding in 2%, procedure-related cholangitis in 1%, cholecystitis in 0.5%, and perforation in 0.3%. In the subgroup of 1600 patients who had common duct stones, the overall complication rate was 8%.
Balloon sphincteroplasty
To potentially decrease the rate of complications of BES, balloon sphincteroplasty (BSP) was introduced as a sphincter-preserving alternative. In addition to the lower risk of bleeding and perforation, another apparent advantage of the procedure is that the sphincter of Oddi function can be preserved. This could avoid the lifelong reflux of duodenal contents into the bile duct through the opened sphincter. BSP was first described by Staritz and colleagues in 1983 but was then nearly abandoned as a treatment of bile duct stones after reports of serious postprocedure pancreatitis. In the mid-1990s, its use was revived with the more favorable results from several groups.
For balloon dilation, a standard guide wire is inserted into the bile duct after selective bile duct cannulation. After removing the catheter, usually a 6- to 10-mm hydrostatic balloon-tipped catheter is passed over the guide wire and positioned across the papilla. The balloon is expanded with contrast medium until ablation of the waistline of the balloon occurs. The dilation is maintained for 15 to 30 seconds. The optimal size of the balloon in BES has not been established. Most studies have reported results with 8-mm diameter dilation balloons, although some studies have used balloons up to 15 mm in diameter.
The drawback of sphincteroplasty compared with sphincterotomy is the more limited size of the papillary opening. Mechanical lithotripsy assistance was more frequently required in the patients undergoing BSP. Stones measuring more than 8 mm often require mechanical lithotripsy to enable extraction across the papilla.
Overall success rate for BSP is comparable with that of BES. The reported success rates of stones removal are 81% to 99% for BSP and 85% to 98% for BES. Randomized trials comparing BSP with BES suggest that BSP is at least as effective as BES in patients with small to moderate-sized bile duct stones. Although sphincteroplasty has decreased rates of bleeding and probably perforation, higher rates of postprocedure pancreatitis are reported. In a US multicenter study by DiSario and colleagues, which randomized patients with suspected biliary stone to endoscopic balloon dilation or endoscopic sphincterotomy, pancreatitis occurred at a rate 2 times greater in the balloon dilation group compared with the sphincterotomy group (15.4% vs 8%, P <.001). The meta-analysis of randomized controlled trials by Baron and Harewood showed an early complication rate of BSP comparable with BES for removing CBD stones during ERCP. Overall, the early complication rates for BSP and BES were 10.5% vs 10.3% ( P = .9). The bleeding rate was higher in the BES group (2.0% vs 0, P = .001) whereas the rate of pancreatitis was higher in the BSP group (7.4% vs 4.3%, P = .05). Another recent meta-analysis demonstrated that the procedure carries significant higher risk of pancreatitis (RR = 1.96) over sphincterotomy. Therefore, in the Western world, BSP is reserved for patients who have uncorrectable coagulopathy and possibly older patients who are less prone to post-ERCP pancreatitis.
Difficult/large common bile duct stones
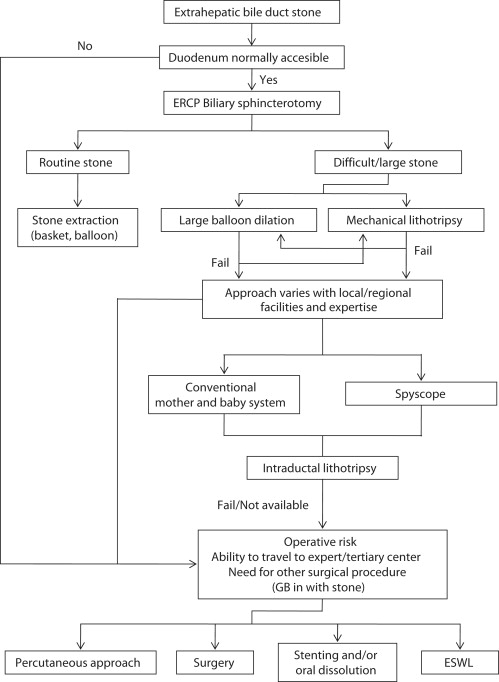
Approximately 10% to 15% of patients have bile duct stones that cannot be removed using standard BES and balloon/basket extraction techniques. These stones generally are larger than 1.0 cm, impacted, located proximal to strictures, or associated with duodenal diverticulua. Such factors make adequate sphincterotomy and extraction difficult. Ultimately, the stone must be (1) extracted from above (ie, bile duct exploration), (2) made smaller (ie, lithotripsy), or (3) have a larger passage way (ie, large balloon dilation). All transpapillary intraductal approaches can also be performed via a percutaneous access with similar success rates but added complications of the transhepatic approach (see Fig. 1 ).
Mechanical lithotripsy
Mechanical lithotripsy was first introduced in 1982 by Riemann and colleagues from Erlangen, Germany, and is now the most widely used technique for fragmentation of stones. The lithotripter unit is a strong-wired basket, which entraps the stone and is then pulled slowly via wench back through a metal sheath. The sheath can go through the scope or be applied after stone capture. The latter requires that the basket handle be cut off, the scope withdrawn, and the spiral metal sheath passed over the basket shaft wire. A lithotripter handle with a large screw or wench is used to pull the basket stepwise into the metal coil. The stone is broken into several pieces as the basket filaments cut through the stone ( Fig. 3 ).
The combination of BES and mechanical lithotripsy has a stone removal success rate of 90% to 97% if the papilla is accessible and the stone can be captured by a basket. In 2 studies, mechanical lithotripsy successfully removed 85% to 90% of difficult bile duct stones. Mechanical lithotripsy usually is successful only in stones smaller than 3 cm. The most common reason for unsuccessful mechanical lithotripsy is inability to capture the stones (eg, inadequate space to open the basket). Densely calcified stones are also more likely to fail lithotripsy.
The complication rate of mechanical lithotripsy has been reported as 3.6% in a recent multicenter comprehensive review. The most frequent complication was trapped or broken basket, and the others were wire fracture, broken handle, or perforation/duct injury. To avoid breakage of the traction wire during procedure, only lithotripsy compatible baskets should be used.
Electrohydraulic lithotripsy
An electrohydraulic lithotripsy (EHL) system consists of a bipolar lithotripsy probe and a charge generator. Initiation of a high-voltage spark discharged across the tip of the EHL probe causes expansion of the surrounding fluid that generates shock waves to fragment stones. Although EHL can be performed under fluoroscopic or direct cholangioscopic guidance, direct visualization is strongly preferred to enable proper deployment of the probe at the surface of the stone to avoid ductal injury ( Fig. 4 ). This technique has the advantage of not requiring stone capture before applying energy. Disadvantages of using cholangioscopy for EHL are the need for 2 operators, the use of a fragile intraductal miniscope, and need for simultaneous nasobiliary tube (in some patients) to flush out fragments. Recently, single-operator cholangioscopy has been used to direct EHL therapy for bile duct stones; preliminary results have been encouraging.
Laser lithotripsy
In laser lithotripsy, laser light at a particular wavelength is focused on the surface of a stone to achieve stone fragmentation. An oscillating plasma, consisting of a gaseous collection of ions and free electrons, is created to induce wave-mediated fragmentation of stones. Laser lithotripsy is performed under direct visualization using the cholangioscope or under fluoroscopic guidance. The latter has greater potential to damage the bile duct wall. A recent-generation device can differentiate between the light reflection patterns of the bile duct wall and those of stones. The laser pulses are automatically interrupted when readings indicate that the probe is aimed at tissue rather than stone. Experience with this modality is limited, however. The success rates of bile duct stone clearance with laser lithotripsy have been reported at 64% to 97%.
A new pulsed, solid-state laser system equipped with higher laser energy, double-pulse neodymium:YAG laser (FREDDY) (World of Medicine, Berlin, Germany), has been developed in Germany. This system promises to combine the advantages of dye and solid state lasers, such as reliability, effectiveness, and low cost. Complete stone removal is achieved in 88% to 94%. Transient hemobilia occurred in 15% of the patients, mostly those who underwent the procedure with fluoroscopic guidance alone.
Extracorporeal shock wave lithotripsy
Extracorporeal shock wave lithotripsy (ESWL) generates a shock wave originating outside the body using piezoelectric, electrohydraulic, or electromagnetic systems. A liquid or tissue medium is required to prevent energy attenuation. Because ESWL is painful, general anesthesia or, less frequently, epidural or conscious sedation is required. Because most bile duct stones are not radiopaque and are not visualized by fluoroscopy alone, a nasobiliary tube with contrast injection is required before ESWL. Complete stone clearance rates of 83% to 90% have been reported. A large prospective study reported that overall clearance rate with successful fragmentation was 84.5%, but a single session of ESWL cleared the stones in only 16% of 283 patients with large CBD stones. In 25% of the patients, 4 to 7 sessions of ESWL were needed. Complications of ESWL have been minimal. A limitation is the considerable recurrence rate of bile duct stones after ESWL reported in 12.7% to 28% of patients on 1- to 3-year follow-up.
Mother and baby choledochoscopy and intraductal lithotripsy
Intraductal EHL or laser lithotripsy is best performed under direct visual control using the mother and baby scope system. An older system consisted of a jumbo size duodenoscope with a 5.5-mm working channel and a baby scope of 4.7 mm in diameter. The EHL or laser probe is passed into the bile duct through the instrument channel of a baby scope for fragmenting stones. Newer baby scopes are smaller, with a 3.2-mm diameter and a 1-mm instrument channel. Such small diameter scopes can be inserted through a standard therapeutic duodenoscope with a 4.2-mm instrument channel. The mother and baby endoscopic system has several limitations, such as its technical difficulty, its time-consuming nature, and the need for an additional endoscopic unit and 2 skilled endoscopists.
SpyGlass SpyScope (Boston Scientific, Natick, MA, USA) is a new partially disposable, less-expensive, single-operator endoscope that has been recently introduced into the endoscopic arena. It includes a baby scope, which is 10F in diameter, has a 4-way tip deflection, and has a 1.2-mm working channel. The baby scope houses the SpyGlass optical fiber, an independent accessory channel, and a separate channel for water irrigation ( Fig. 5 ). It can be used perorally or percutaneously. EHL can be readily applied by this system. Recent studies showed rate of stone clearance at 87% to 100% as well as usefulness in histologic diagnosis of bile duct stricture.
Direct peroral cholangioscopy
The goal of this most recent stone management tool, direct peroral cholangioscopy, is to avoid mother and baby scope system limitations. Direct peroral cholangioscopy uses an ultraslim upper endoscope with a 4.9- to 6-mm tip diameter and greater than 140 cm length and is conducted by a single endoscopist. The procedure generally requires a large sphincterotomy, a terminal CBD greater than 10 mm diameter, placement of a guide wire or anchoring balloon into a peripheral bile duct via standard ERCP, passage of the direct cholangioscope over the anchoring balloon/wire, removal of the anchoring wire, and then use of intraductal lithotripsy. A nasobiliary drain for flushing out fragments may be needed. An overtube may be needed to prevent intragastric bowing. Experience is limited, but recent studies show feasibility and clinical usefulness. Limitations of the technique included limited availability of such prototype endoscopes, limited experience to date, and tendency for the endoscope to fall back into the duodenum.
Supplemental endoscopic papillary large balloon dilation
Use of a large-diameter (12 to 20 mm) dilation balloon after near-maximal or limited BES has been introduced as an adjunctive tool to enlarge a papillary orifice for the removal of large or difficult bile duct stones ( Fig. 6 ). The concept is to combine the advantages of sphincterotomy with those of balloon dilation. Theoretically, risk of perforation or bleeding would be reduced by performing a less than maximal sphincterotomy, and risk of pancreatitis from balloon dilation would be reduced by first separating the biliary and pancreatic orifices with biliary sphincterotomy.
Data regarding supplemental endoscopic papillary large balloon dilation (EPLBD) are relatively limited. Most of the studies regarding EPLBD are retrospective analyses or have limited numbers of patients enrolled. In a multicenter study, Attasaranya and colleagues reported efficacy of EPLBD using large-diameter balloons (≥12 mm) after sphincterotomy in 103 patients with large CBD stones at 5 ERCP referral centers in the United States. The combined technique had a success rate of 95% and a complication rate of 6%. Failure of complete stone clearance occurred in 5 procedures (5%). Short-term complications were documented in 6 patients (5.4%), including a single case of cystic duct perforation. Two patients had complications of hemorrhage, including 1 patient who had severe bleeding requiring vascular coil embolization, but none had procedure-related pancreatitis. Heo and colleagues from Korea randomized 200 consecutive patients with bile duct stones of mean 15 mm in diameter in equal numbers to partial BES plus large balloon dilation (12- to 20-mm balloon diameter) or full BES alone. Outcomes were similar in terms of overall successful stone removal, large (>15 mm) stone removal, and need for mechanical lithotripsy assistance. Overall complications were also similar between the 2 groups. Pancreatitis occurred in 4% of the large balloon dilation group whereas none of the patients developed perforation or bleeding. Other recent studies have reported similar results for large/difficult bile duct stones with a complete stone removal rate at 95% to 100%, overall complication rate at 3.8% to 8.3%, and low incidence of pancreatitis. A preliminary report from Korea noted 2 fatal complications, 1 due to perforation and the other from massive bleeding, in a series of 166 patients. Although their multivariate analysis could not identify clear risk factors for complications, the size of balloons used in this study was likely larger than in other studies and may have been larger than the native duct in some cases.
Details of the method not yet standardized include optimal size of balloon, duration of dilation, and extent of sphincterotomy. Use of a balloon that is equal to or smaller in diameter than the native distal bile duct seems logical, because use of a larger balloon might be expected to tear the sphincter and possibly the duct as well, resulting in the cases of bleeding and perforation that have been observed. Additionally, it seems logical that achieving best results would require adapting a balance of size of sphincterotomy and balloon dilation to each patient’s anatomy, the size and burden of stones, the shape and size of the papilla, and presence of the papilla in or adjacent to diverticula. Patients with distal CBD stenosis or a relatively narrow “normal” CBD are probably at higher risk of complications after balloon dilation. Therefore, it seems prudent to limit dilation to 2 to 3 mm larger than the native duct diameter.
This technique may be helpful in patients with difficult papillary anatomy, such as those with small papilla or intra- or peridiverticular papilla. Its role in patients with coagulopathy, however, or other risks for bleeding remain to be investigated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






