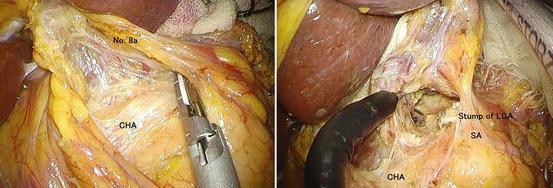
Fig. 17.1
Positions of the equipment and the surgical team and placement of trocars through transumbilical port for the SLS gastrectomy for gastric cancer
17.3.2 Port Setting
An umbilical laparotomy through a 2.5- to 3-cm vertical skin incision into the umbilicus was made by the open method. A wound protector (Lap retractor (Hakko Co., Nagano, Japan)) was applied to this wound. A plastic cover (E-Z access (Hakko Co., Nagano, Japan)) with 4 trocars inserted in a diamond-shaped position (Fig. 17.1) is then placed, and pneumoperitoneum was established. The bottom 12-mm trocar was used for introducing the laparoscope. The main surgeon performed the procedures with a co-axial setting using a conventional straight instrument and an energy device through bilateral trocars. An assistant provided counter-traction to maintain the surgical view using forceps through a top trocar in the umbilical access port.
17.3.3 Procedure
After establishment of the CO2 pneumoperitoneum, a careful exploration of the entire peritoneal cavity was done to examine the metastasis of other organs, such as liver metastasis and peritoneal dissemination.
17.3.3.1 Liver Retraction
Proper liver retraction was a key to the success of the laparoscopic gastrectomy. Our preference is the “V-shape retraction technique” as follows: a straight needle with 2-0 nylon was used to puncture first the upper abdomen and then at the right crus and through the abdominal wall again. It was simple and inexpensive without leaving a scar at the punctured site.
17.3.3.2 Suprapancreatic Lymph Nodes Dissection
Suprapancreatic lymphadenectomy is one of the most important and technically difficult aspects of laparoscopic gastrectomy. Various approaches, such as right-to-left, left-to-right (left-sided approach), and medial-to-lateral (medial approach), have been reported in conventional laparoscopic gastric surgery, which can be applied to the single port approach. In these approaches, dissection is initially performed at the cranial edge of the pancreas and then proceeds in a dorsal-to-cranial direction. The medial approach is quite effective for complete dissection of the lymph nodes, with dissection of the layer between the adipose tissue (including lymphatic tissue and the autonomic nerve sheath of major arteries) and medial transection of the left gastric artery [12]. We commonly use the cranial-to-caudal approach (cranial approach), in which the mobilization of the stomach and pancreas and the dissection of the cranial side of the station no. 9 lymph nodes are performed prior to the medial approach. We believe that prior dissection of cranial connections between the lymph nodes and the plexus celiacus will make it easier to perform cephalad dissection of the suprapancreatic lymph nodes in the conventional approach.
17.3.3.3 The Cranial Approach
The patient was placed in the reverse Trendelenburg position. The assistant introduced the intestinal grasping forceps with gauze from the top trocar to retract the stomach caudad. The main surgeon retracted the liver cephalad for retraction of the hepatogastric ligament. The assistant’s forceps were placed between the surgeon’s bilateral forceps. The procedure was performed smoothly without interference of each instrument in this formation, which is a basic positioning for this surgery (Fig. 17.2). The hapatogastric ligament was then dissected towards the esophagus with preservation of the hepatic branches of the vagus nerve (Fig. 17.2). The mesogastrium was retracted anteriorly using a grasper introduced through the right trocar. The peritoneum was incised at the level of the right crus of the diaphragm (Fig. 17.3). This incision continued downward along the right crus up to the celiac artery. The mesogastrium was retracted anteriorly to expose the posterior space. The plane between Gerota’s fascia and Toldt’s fusion fascia could then be identified. This plane is avascular and easily divided. The dissection continued posterior to the Toldt’s fusion fascia going laterally and caudad. By this dissection, both the pancreatic body and stomach were mobilized.
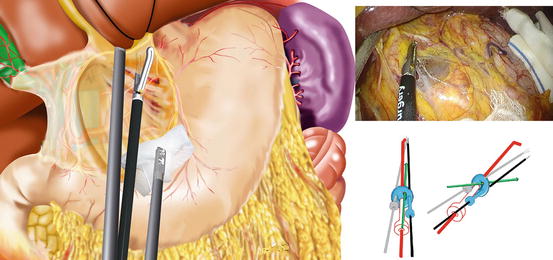
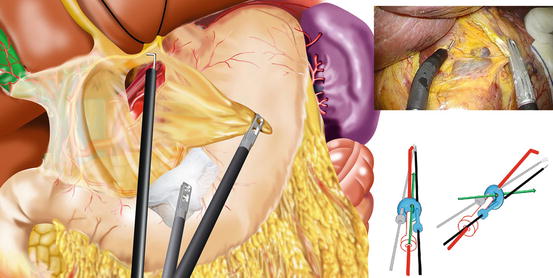
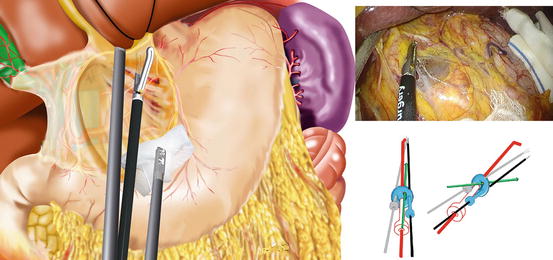
Fig. 17.2
The hepatogastric ligament is dissected with the aid of caudal counter-traction by the assistant’s forceps with gauze, preserving the hepatic branches of the vagus nerve
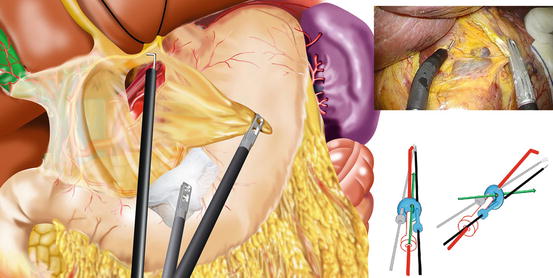
Fig. 17.3
In the cranial approach, the mesogastrium is tented ventro-laterally, and the peritoneum is incised along the right crus of the diaphragm. The plane is dissected between Gerota’s fascia and Toldt’s fusion fascia to mobilize the stomach and pancreas from the retroperioneum
The left gastric artery was carefully grasped and retracted in a ventro-lateral direction. The adipose tissue including the station no. 9 lymph nodes was separated from the outer layer of plexus celiacus, and we identified the three branches of the celiac artery—the left gastric artery, the common hepatic artery, and the splenic artery. If possible, the left gastric artery should be skeletonized distally, clipped, and divided at its origin using a vessel-sealing device or laparoscopic coagulation shears (Fig. 17.4). This adequate separation of the lymph nodes from the nerve increased the movability of the lymph nodes and facilitated the following caudal-to-cranial dissection of the suprapancreatic lymphadenectomy (Fig. 17.5).
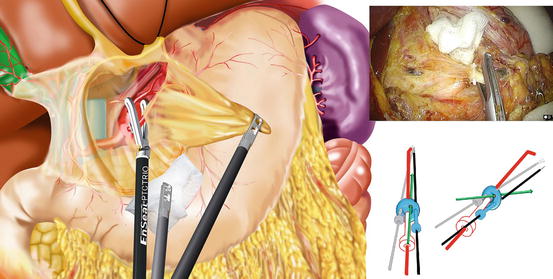
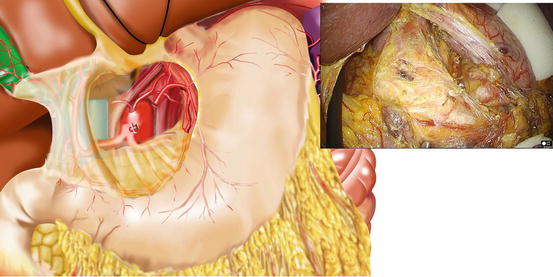
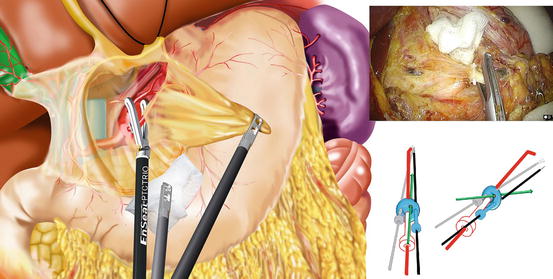
Fig. 17.4
The left gastric artery is clipped and divided at its origin
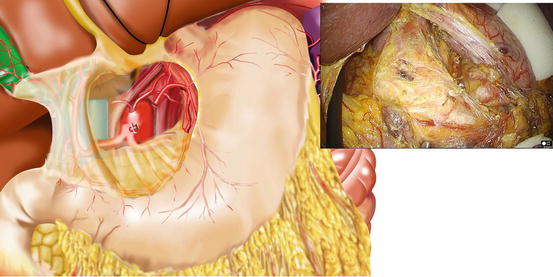
Fig. 17.5
The cranial approach is completed by exposing the celiac plexus. The cranial side of no. 9 lymph node is separated from the nerve ganglion
17.3.3.4 Dissection of No. 5 Lymph Nodes and Division of Right Gastric Artery
The assistant introduced the intestinal grasping forceps with gauze from the top trocar to retract the duodenum caudad and stretch the hepatoduodenal ligament. The main surgeon retracted the right gastric artery in a ventro-lateral direction. The ventral peritoneum was initially incised along the duodenum, and the opening window was spread. Under continuous traction, the peritoneum was incised cephalad along the right edge of the proper hepatic artery up to its bifurcation. Using a combination of gentle force and sharp dissection, the right gastric artery with lymph nodes was swept ventrally and the hepatic plexus swept dorsally. Then the right gastric artery was divided using a vessel-sealing device or laparoscopic coagulating shears (Fig. 17.6).
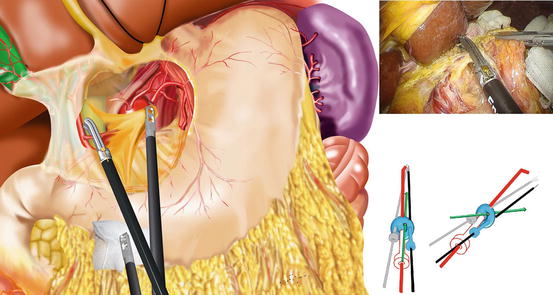
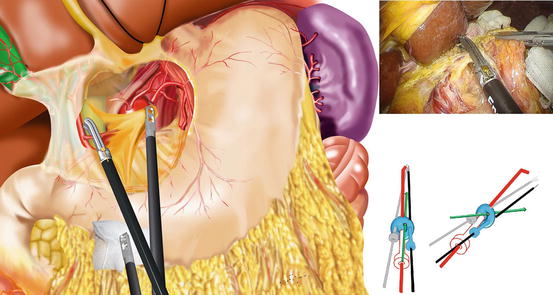
Fig. 17.6
The right gastric artery is retracted ventro-laterally and divided using a vessel-sealing device
17.3.4 Dissection of the Suprapancreatic Lymph Nodes
The assistant introduced the intestinal grasping forceps with gauze from the top trocar to retract and rotated the pancreas in a dorsocaudal direction. After the suprapyloric lymph nodes were separated from the right gastric artery, the main surgeon provided traction by using the right hand grasper to pick up the cut edge of the peritoneum. The peritoneum was incised toward the left side along the cranial edge of the pancreas, while the adipose tissue with lymph nodes was separated cephalad and laterally from the hepatic plexus and splenic plexus. If the proper plane is entered posteriorly, no bleeding will occur, and the connective tissue in this plane can be divided easily. This plane directly connects the previous dissection plane from the cranial approach, providing a wide space for lymphadenectomy (Fig. 17.7). Dissection continued in a medial-to-lateral direction by applying ventrolateral traction with a grasper along the bilateral celiac ganglion.