Fig. 10.1
Spectrum of alcoholic liver disease and main modifying factors. The percentage represents the patients who progress from one stage to the next
Alcohol-induced steatosis is characterized by the accumulation of fat (mainly triglycerides, phospholipids, and cholesterol esters) in hepatocytes. The natural history of simple steatosis is not well known, but is considered to be a benign condition. Whether it predisposes to extrahepatic consequences such as diabetes or cardiovascular disease is unknown. It has been estimated that a third of patients with steatosis will develop hepatic inflammation (ASH) if they are persistent in drinking abusively [18]. ASH is a syndrome characterized by inflammatory cell infiltration of the liver (mostly PMN) and hepatocellular injury. ASH includes a spectrum of diseases ranging from mild damage to severe, life-threatening injury [17, 19]. Patients with ASH can develop progressive fibrosis. Liver fibrosis represents a wound-healing response to repeated liver injury. The persistence of ASH over a long period may accelerate the progression of fibrosis, yet the precise natural history of this condition is not well known [20]. The most advanced stage of fibrosis is micronodular cirrhosis, which may be mixed with macronodular in some patients [21]. The clinical course of alcoholic cirrhosis is similar to other types of liver disease. Alcoholic cirrhosis can rapidly progress to end-stage liver disease if the patients continue drinking. Due to immune paralysis, ALD cirrhotics are predisposed to severe infections that carry bad prognoses [22].
Patients with advanced ALD and active drinking can develop an episode of superimposed AH [13]. AH is a life-threatening condition characterized by an abrupt increase in bilirubin and other parameters of liver synthetic dysfunction as well as severe portal hypertension. In severe cases and in patients with liver cirrhosis, AH leads to severe complications related to liver failure and portal hypertension and carries a high short-term mortality [17].
The modifying factors for ALD are not well known and are based on few retrospective studies that identified several risk factors for the susceptibility of ALD. These include gender, obesity, drinking patterns, dietary factors, non-sex-linked genetic factors, and cigarette smoking [19, 23, 24]. Female sex is a well-documented risk factor for susceptibility to ALD, likely due to lower levels of gastric alcohol dehydrogenase, a higher proportion of body fat, and the presence of estrogens. The amount and type of alcohol consumed, drinking patterns, dietary factors, and cigarette smoking have been shown to influence the risk of developing ALD cirrhosis [25]. Current attention is being paid to the deleterious effects of “binge drinking,” which is particularly common in [26] the young population [27]. Obesity is , another factor that can synergistically accelerate fibrosis progression and cirrhosis development in heavy drinkers [28, 29]. The mechanisms of such interactions are not well described. In the experimental setting, a high-fat diet exacerbated several of the pathogenic consequences of alcohol, including ER stress and macrophage activation [30]. The genetic factors that influence an individual’s susceptibility to the development of advanced ALD are largely unknown. Variations in genes encoding antioxidant enzymes rather than cytokines and alcohol-metabolizing enzymes seem to play a role [24]. As occurs in NAFLD, adiponutrin (PNPLA3) is a major modifier of ALD [26]. Finally, chronic drinking synergistically accelerates progression of liver diseases in the presence of comorbid factors such as hepatitis virus B or C and/or HIV infection, nonalcoholic fatty liver disease, hemochromatosis, etc. For example, it is well documented that alcohol consumption and viral hepatitis often coexist and synergistically accelerate the progression of liver fibrosis, cirrhosis, and HCC [31, 32].
Diagnostic Approaches in ALD
Clinical, Analytical, and Imaging Diagnosis of ALD
Diagnosis of early-stage ALD is based on the combination of clinical, laboratory, and imaging findings. With adequate history of excessive drinking and analytical evidence for liver disease, the diagnosis of ALD can be established without the need of histological confirmation in most cases. Unfortunately, symptoms often develop only after severe, life-threatening liver disease has already developed. There is an urgent need to develop programs for the early detection of ALD in primary care centers and alcohol addiction clinics. A careful medical history from the patient and close relatives is needed to obtain information on the amount, frequency, duration, and type of drinking. Obtaining an accurate alcohol use history in patients with suspected ALD can be difficult, since many patients underreport their alcohol consumption. In some cases, speaking with the patient’s family or close friends may help in obtaining a more precise history. Underreporting should be suspected if stigmata of alcoholism, compatible laboratory findings, or other affected organs are present. A structured questionnaire should be administered to obtain more qualitative information about a patient’s alcohol consumption and problems. Among the different existing questionnaires, the AUDIT (Alcohol Use Disorder Inventory Test) remains the “gold standard” tool [33].
At physical exam, patients with steatosis may have a normal examination or hepatomegaly. Patients with AH typically present with jaundice, and patients who have developed cirrhosis may have peripheral stigmata of liver disease, splenomegaly, or signs of hepatic decompensation. Physical examinations may also show evidence of chronic alcohol consumption (vascular ectasia, parotid hypertrophy, Dupuytren’s contracture, sarcopenia, signs of peripheral neuropathy, rhinophyma, etc.) (Table 10.1). These signs can be useful to identify ALD in patients that underreport the abusive alcohol consumption.
Table 10.1
Physical examination findings in patients with alcohol use disorder
Abdominal wall collaterals |
Ascites |
Cutaneous telangiectasias |
Digital clubbing |
Disheveled appearance |
Dupuytren’s contractures |
Gynecomastia |
Hepatomegaly |
Jaundice |
Malnutrition |
Palmar erythema |
Parotid enlargement |
Peripheral neuropathy |
Rhinophyma |
Spider angiomata |
Splenomegaly |
Testicular atrophy |
For patients with a history of alcohol misuse and evidence of liver disease, further laboratory tests should be done to exclude other etiologies and to confirm diagnosis. Laboratory tests that should be obtained in patients with suspected ALD include liver function tests, a complete blood count, serum albumin, and coagulation studies (prothrombin time, INR). There are no laboratory tests that reliably differentiate ALD from other causes of liver disease. The most common pattern of liver biochemical test abnormality in ALD is a disproportionate elevation of the aspartate aminotransferase (AST) compared with the alanine aminotransferase (ALT) , resulting in a ratio of AST to ALT greater than 1 [34, 35]. AST to ALT ratio >2 is highly suggestive of ALD, although it can also be found in advanced cirrhosis of any etiology [36]. A typical finding in patients with ALD is elevated γ-glutamyl-transpeptidase (GGT). However, GGT activity is not specific for ALD and can be also elevated by other conditions such as cholestatic liver disease, cardiac insufficiency, and drugs such as antifungals or anticonvulsants. Another biomarker indicative of alcohol abuse is carbohydrate-deficient transferrin (CDT) [37]. A combined index including GGT and CDT can be useful in detecting hazardous alcohol intake [38].
Among imaging techniques , abdominal ultrasound is the most widely used in patients with ALD. Ultrasound can detect hepatic steatosis if it affects 30 % of the liver [39, 40]. In severe ALD, Doppler ultrasound can detect the presence of a cirrhotic liver as well as signs of portal hypertension (splenomegaly, changes in portal vein flow, presence of collaterals and ascites). Moreover, it is the technique of choice for the screening of portal vein thrombosis and HCC. More sophisticated techniques such as abdominal CT scan and magnetic resonance imaging (MRI) are more accurate than ultrasonography for evaluating steatosis, but are not cost-effective [41]. They are used for a more precise diagnosis of HCC or when there is suspicion of biliary obstruction. Of note, imaging studies cannot establish alcohol as the specific etiology of a given chronic liver disease.
Noninvasive Diagnosis of ASH and Fibrosis
In the last decade there have been major advances in noninvasive techniques to assess the severity of a liver disease. Because patients with ASH and fibrosis are at high risk for developing cirrhosis, it is important to detect these progressive forms of ALD. Several serum tests developed for the noninvasive assessment of viral hepatitis have also been tested in patients with ALD [42]. They include serum biomarkers and elastography. The AST to platelet ratio index has a limited value in the diagnosis of fibrosis in ALD [43]. More sophisticated serum tests such as FibroTest®, FibrometerA®, Hepascore®, and ELF have been evaluated in patients with ALD [44–47]. FibroTest® is a marker panel composed of alpha-2-macroglobulin, haptoglobin, GGT, ApoA1, and bilirubin, corrected for age and sex [48]. It has high diagnostic accuracy for the detection of significant fibrosis in patients with ALD [44]. Importantly, the ELF test may predict clinical outcomes in patients with chronic liver disease, but its efficacy was not validated in larger cohorts of ALD patients [47]. The AshTest estimates the presence of ASH from the patient’s levels of α2-macroglobulin, haptoglobin, ApoA1, total bilirubin, GGT, ALT, and AST [49]. In heavy drinkers, AshTest represents a potential noninvasive marker to estimate of the presence of ASH [49].
The measurement of liver stiffness by transient elastography (Fibroscan® ) represents a major advance in the noninvasive assessment of the degree of liver fibrosis including patients with ALD [50, 51]. This device was recently approved by the FDA. In patients with ALD, liver stiffness correlates with the degree of fibrosis [52]. However, inflammation, cholestasis, or liver congestion may affect liver stiffness measurement independently of the degree of fibrosis [53]. Elevated liver stiffness values in patients with ALD and AST serum levels >100 U/L should be interpreted with caution due to the possibility of falsely elevated liver stiffness as a result of superimposed ASH [42]. Moreover, recent alcohol consumption can also elevate liver stiffness, perhaps related to the vasodilatory effects of alcohol [54]. Thus, the correct interpretation of liver stiffness requires a timely abdominal ultrasound and actual transaminase levels and alcohol consumption. Controlled attenuation parameter (CAP) is run on the Fibroscan platform. Preliminary results suggest that CAP is reproducible and quantitative with an AUROC up to 90 % for fatty liver [55].
Liver Biopsy
Liver biopsy is rarely indicated in patients with high suspicion of ALD, though it is the most accurate method to establish the severity of liver injury in ALD [56, 57]. Liver biopsy can be done percutaneously but often requires a transjugular approach in patients with advanced ALD due to coagulopathy. The morphological features of ALD encompass four elementary lesions: macrovesicular steatosis, centrilobular ballooning of hepatocytes, neutrophil infiltrate that predominates in the lobules, and variable degrees of liver fibrosis [58]. Macrovesicular steatosis is the most frequent pattern of alcohol-induced liver injury [58]. Neutrophil infiltration is typically first seen in zone 3 (perivenular). As the disease progresses, the histologic changes also affect zone 2 and even zone 1 (periportal) hepatocyte. The presence of neutrophils is a hallmark of ASH. Mallory-Denk bodies are eosinophilic accumulations of intracellular protein aggregates within the cytoplasm of hepatocytes. They represent condensations of intracellular “intermediate filaments” or cytokeratins that are normal components of the hepatocyte cytoskeleton [59]. They are not specific to ASH and can be seen in nonalcoholic steatohepatitis (NASH) [60]. Alcoholic fibrosis is typically located in pericentral and perisinusoidal areas and first appears in the zone 3 area [61], and there is underlying cirrhosis in many cases [17, 19]. Patients with ALD can develop a particular pattern of liver fibrosis (chicken wire) due to massive pericellular and perisinusoidal deposition of collagen fibers (Fig. 10.2).
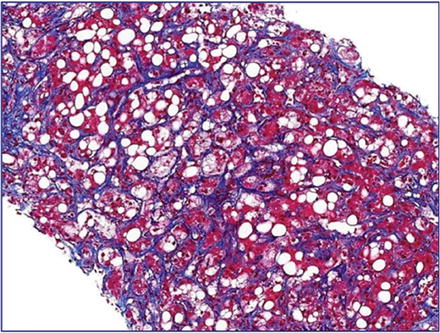
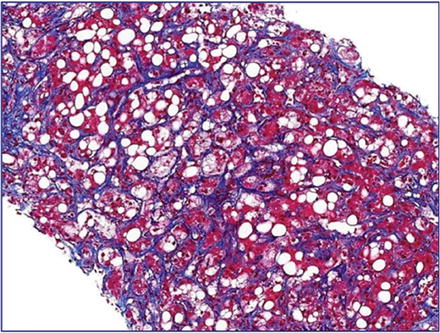
Fig. 10.2
Panlobular fibrosis in a patient with severe alcoholic liver disease showing a typical “chicken wire” pattern
The clear indications of liver biopsy are not established; however, it should be considered in patients with severe AH requiring specific medical therapy and in patients with other coexisting factors contributing to liver disease. Relying on clinical criteria alone carries a 10–50 % risk of misclassifying patients as having or not having AH [62, 63]. Therefore, the recently published EASL Practical Guidelines on Alcoholic Liver Disease recommends a liver biopsy, if available, in patients with suspected severe AH [64]. In patients with the clinical syndrome of AH and any one of the followings factors, liver biopsy is specially recommended: (1) hypotension/massive bleeding at admission, (2) sepsis at admission, (3) suspicion of malignant liver disease based on clinical and/or imaging criteria, (4) uncertain assessment of alcohol drinking history, (5) cocaine use in the last 3 months, and (6) recent use of a potential hepatotoxic substance. Future studies should identify noninvasive markers capable of estimating the presence of AH without the need of a liver biopsy.
Diagnosis of Alcoholic Cirrhosis
Alcoholic cirrhosis can be silent for many years, and therefore it can only be diagnosed if analytical and imaging studies are performed. Often, patients with alcoholic cirrhosis are diagnosed upon the development of a clinical complication. Patients who have decompensated cirrhosis may report jaundice, weakness, peripheral edema, abdominal distension, or symptoms of gastrointestinal bleeding. Cirrhotic patients usually have stigmata of chronic liver disease such as palmar erythema, spider angiomata, and gynecomastia. Asterixis is seen in patients with hepatic encephalopathy. A low number of platelets are indicative of cirrhosis or advanced fibrosis in chronic liver disease. Thrombocytopenia may result from primary bone marrow hypoplasia or splenic sequestration. Leukopenia and anemia develop later in the disease course [65]. In patients with ALD, anemia is typically megaloblastic. Albumin levels fall and INR increases as the synthetic function of the liver declines.
Specific imaging features indicating the presence of alcoholic cirrhosis include a nodular appearance of the liver, higher volume index of the caudate lobe, frequent visualization of the right posterior hepatic notch, and smaller size of regenerative nodules of the liver [66]. In early cirrhosis without major macroscopic changes, the sensitivity of imaging studies is less than 70 %. Thus, ultrasound findings are useful to confirm the presence of alcoholic cirrhotic livers, but a negative result cannot fully rule out cirrhosis. As described above, noninvasive techniques can be useful to detect the presence of cirrhosis, as well as a liver biopsy in special cases. Of note, noninvasive tests including elastography are not specific enough to detect the presence of esophageal varices, so an upper endoscopy is indicated in all patients with the diagnosis of liver cirrhosis.
Diagnosis of AH
The diagnosis of AH is made on clinical grounds, based on a history of excessive alcohol use with the typical physical exam and laboratory findings. Liver biopsy may be helpful to establish the presence of ASH and has been endorsed in recent clinical practice guidelines [64, 67]. As detailed above, a biopsy is particularly valuable in the setting of atypical clinical characteristics or when the diagnosis remains in doubt. A transjugular route is often preferred due to frequent coexisting ascites and/or coagulopathy. Infections, particularly spontaneous bacterial peritonitis, must be ruled out as they can present with similar clinical findings (abdominal pain, fever, leukocytosis) and because they are a contraindication to specific therapy with corticosteroids. Serologic evaluation for viral hepatitis should be undertaken as well. Imaging with Doppler ultrasound is important to exclude biliary or vascular disorders and to evaluate for coexisting hepatocellular carcinoma. Contrast-enhanced computed tomography or magnetic resonance imaging is often helpful to confirm ultrasound findings.
Recently, we performed a large multicentric study to develop a histological scoring system capable of predicting short-term survival in patients with AH. The resulting alcoholic hepatitis histological score (AHHS) comprises four parameters that are independently associated with patients’ survival: fibrosis stage, PMN infiltration, type of bilirubinostasis, and presence of megamitochondria. By combining these parameters in a semiquantitative manner, we were able to stratify patients into low, intermediate, or high risk for death within 90 days [68].
Assessment of Extrahepatic Alcohol-Induced Organ Damage
Patients with ALD often have coexisting dysfunction in extrahepatic organs and may have signs of malnutrition, cardiomyopathy, neuropathies, pancreatic dysfunction, and skeletal muscle wasting (sarcopenia). A nutritional assessment is necessary for all patients with ALD due to the association between alcoholism and nutritional deficiencies such as protein, calories, minerals (e.g., zinc), and vitamins (e.g., vitamin D). Long-term excessive alcohol consumption can also be a cause of cardiomyopathy [69]. A history of heavy and prolonged alcohol intake in addition to the signs and symptoms of heart failure is the basis of a diagnosis of alcoholic cardiomyopathy, which can be confirmed by echocardiography. Chronic alcoholic myopathy is defined by muscle atrophy and weakness predominantly in the proximal muscles and may affect 40–60 % of alcoholics [70]. The association between myopathy and neuropathy in alcoholics might be due to direct effects on ethanol/acetaldehyde and ethanol-mediated oxidative stress on muscle and neurons [71]. Although patients with ALD typically do not have concomitant pancreatic disease, patients with chronic abdominal pain or steatorrhea should be worked up to rule out chronic pancreatitis. Acute pancreatitis is one of the most severe complications in patients with alcohol use disorder. Due to the progression of pancreatic fibrosis from ethanol, prolonged drinking may lead to the development of chronic pancreatitis [72]. Chronic pancreatitis is common in alcoholics and poses a risk for the development of pancreatic cancer.
Alcohol abuse is commonly associated with an array of neurological disorders. A complete neurological examination is therefore recommended in patients with ALD. The most common type of central nervous system damage from heavy drinking is brain atrophy, which may lead to dementia [73]. Mild cognitive impairment has been reported in 50–80 % of alcoholics and can be difficult to differentiate from chronic encephalopathy [74]. Wernicke’s encephalopathy is an acute neurological disorder that is caused by thiamine deficiency and manifests in a clinical triad of encephalopathy, oculomotor dysfunction, and gait ataxia. Prevention of this syndrome relies on thiamine administration, particularly for patients receiving intravenous glucose. Alcoholics often present peripheral polyneuropathy, caused by nutritional vitamin B complex deficiency and the direct toxic effect of acetaldehyde. The pathogenesis of this disorder may involve ethanol-induced lipid peroxidation and defective antioxidant mechanisms within the sciatic nerve [75]. Alcoholic polyneuropathy is a gradually progressive disorder of sensory, motor, and autonomic nerves. Symptoms include numbness, paresthesia, burning dysesthesia, pain, weakness, muscle cramps, and gait ataxia. The prognosis of alcohol-induced neurological manifestations is poor since most of the symptoms do not reverse after prolonged abstinence.
Clinical End Points in Patients with ALD
The most effective therapy for all patients with ALD, regardless of the disease stage, is prolonged abstinence from alcohol. Improved clinical outcomes are observed with abstinence across the spectrum of ALD, from the early to most severe cases [19, 64]. Therefore, prolonged alcohol abstinence is the first and most important clinical end point for patients with ALD. In patients with early asymptomatic phenotypes (fatty liver and ASH with or without mild fibrosis), the clinical end points consist of normalization of laboratory abnormalities and resolution of fibrosis. There are several noninvasive tests to assess the degree of fibrosis; however, none of these tools have been validated in longitudinal studies. As such, there is a clear need to develop noninvasive tools to monitor the response to therapy in patients with early ALD. In contrast, the high short-term mortality of patients with severe ALD, such as decompensated cirrhosis, makes prolonged short-term survival the main clinical end point for these patients. Other important end points include a reduction in the occurrence and severity of clinical complications and the improvement of tests indicative of liver failure (i.e., ABIC or MELD score).
Achieving Prolonged Alcohol Abstinence
Achieving and maintaining alcohol abstinence are the most important treatment goal for patients with ALD, since abstinence improves patient survival and prognosis [76, 77]. Abstinence is also critical for patients with advanced disease who may eventually require liver transplantation, because patients who actively engage in alcohol consumption are not eligible for most programs. The life event of AH should be used to initiate early interventions to achieve abstinence. Referral to addiction specialists or rehabilitation is recommended. Early referral from hospitalization, as well as the use of a multidisciplinary team including an addiction therapist, increases patient adherence and the number of patients who achieve prolonged abstinence (unpublished observations).
With initial abstinence achieved, prolonged maintenance becomes the primary goal for patients with ALD. In addition to addiction counseling and rehabilitation, anticraving drugs may help prevent alcohol relapse. Disulfiram is frequently prescribed for the treatment of alcoholism [78], but is not recommended in patients with advanced ALD due to its potential severe hepatotoxicity [79]. Acamprosate and naltrexone also reduce the withdrawal effects of and the craving for alcohol, but they can also cause hepatotoxicity [80, 81]. Baclofen, a GABA-B receptor agonist, has been found to be effective in the maintenance of abstinence. Importantly, a study involving patients with liver cirrhosis found that a 12-week course of baclofen effectively maintained abstinence by reducing the craving for alcohol without causing hepatotoxicity [82]. This study was recently confirmed [83], suggesting that baclofen is the only fully safe anticraving drug for patients with ALD.
Slowing Disease Progression in Patients with Early Forms of ALD
There are few studies assessing strategies to slow down or even reverse fibrosis progression in patients with ALD. The lack of studies is influenced by intrinsic difficulties in performing clinical trials in patients with an active addition (e.g., poor compliance). Moreover, patients enrolled in clinical trials are likely to reduce their alcohol intake, which can attenuate fibrosis progression. The fact that placebo-treated patients in large trials showed reduction in fibrosis supports this assumption [84]. To date, the only effective therapy to reverse fibrosis in patients with ALD is abstinence from alcohol. Total abstinence from alcohol consumption enhances the clinical outcome of liver disease, this being the most important factor in determining long-term survival in alcohol-related cirrhosis [85]. There are few systematic reports indicating that alcohol abstinence is the main determinant of outcome in patients with compensated ALD [86]. Moreover, isolated reports indicate that alcohol abstinence is followed by fibrosis regression [87]. Disease progression of patients with ALD is heavily influenced by both genetic and environmental factors. Prospective studies are needed to uncover the genetic and environmental factors involved in fibrosis resolution.
There are three critical steps needed to develop new antifibrotic therap ies for patients with ALD. First, it is important to define the patient population in terms of alcohol consumption. Patients unable to completely stop drinking but likely to be compliant during the clinical trial should be identified. Second, clinical trials should incorporate noninvasive markers of liver fibrosis to monitor the response to therapy, since performing paired biopsies in placebo-treated patients is not ethical. And, third, antifibrotic drugs that target key pathogenic drivers in ALD should be selected. The ideal antifibrotic drug should be relatively cheap, well tolerated over prolonged periods, and not associated with hepatotoxicity or HCC development. Large well-designed clinical trials with this and other targeted therapies should be tested in patients with ALD.
Improving Survival in Patients with Alcoholic Cirrhosis
Once liver cirrhosis is established, abstinent patients may present a slower disease progression than those actively consuming alcohol. Moreover, patients with persisting alcohol intake may develop some degree of ASH that may lead to a higher risk of decompensation (conditions such as ascites, hepatic encephalopathy, variceal bleeding, or renal dysfunction) or to the development of HCC. Management of alcoholic cirrhosis focuses on alcohol abstinence, nutritional therapy rich in calories and proteins [88], and prophylaxis of cirrhosis complications. Regarding clinical decompensations, there is no evidence supporting different management strategies in alcoholic cirrhosis compared to other causes of cirrhosis other than the encouragement of alcohol intake cessation.
Improving Survival in Patients with AH
Alcoholic hepatitis carries high short-term mortality (around 30–50 % at 3 months). Treatment of patients with AH has not substantially improved in the last decades. Therefore, the main goal in the management of AH is to improve short-term mortality. Several prognostic models have been developed to identify patients with AH who are at high risk of death within 1–3 months of their hospitalization. The most widely used is Maddrey’s discriminant function (DF) [89]. The DF value ≥32 is indicative of a high risk of short-term mortality (35 % at 1 month) and is the basis for patient selection for specific therapy with corticosteroids. Additional predictive models include the Model for End-Stage Liver Disease (MELD), the Glasgow AH score, the ABIC score, and the Lille model (www.lillemodel.com) [90–92]. Finally, histological assessment using the recently developed AHHS is able to stratify patients into low, intermediate, or high risk for death within 90 days [68].
General measures for the management and treatment of complications related to AH have not been shown to improve survival, but they should be considered as part of the standard of care. Patients with severe AH may require admission to an intensive care unit. The airway should be protected in patients with acute alcoholic intoxication or an advanced degree of hepatic encephalopathy. Benzodiazepines are generally contraindicated in these patients, but might be necessary in the case of severe alcohol withdrawal. There is a potential risk of Wernicke’s encephalopathy among alcoholic and malnourished patients; thus, the administration of vitamin B complex is recommended. Nutritional support improves liver function, and short-term follow-up studies suggest that improved nutrition might improve survival times and histological findings in patients with AH [88, 93, 94]. In patients without encephalopathy, oral supplements and/or feeding through a nasogastric tube is preferred over total parenteral nutrition in order to avoid gram-positive bacterial infections.
Corticosteroids are widely used as the first-line therapy and improve short-term survival in patients with severe AH [95]. The response to prednisolone can be assessed based on the change in bilirubin after 1 week of therapy and quantified using the Lille score [96]. For those with a poor response as indicated by a Lille score ≥0.45, stopping therapy can be considered, as there is likely no benefit to continuing steroids in this setting. Pentoxifylline reduced mortality in patients with severe AH [97] and is typically reserved as a second-line agent for patients with contraindications to corticosteroid therapy (i.e., uncontrolled infection, GI bleeding). However, in a large randomized controlled trial (STOPAH) that included more than 1000 patients, presented during the 2014 AASLD meeting, pentoxifylline was not better than placebo in terms of short-term mortality [98].
Unfortunately, there are no available rescue therapies for patients not responding to standard therapy. The combination of prednisolone and pentoxifylline offers no benefit [99]. A recent randomized trial showed that the combination of N-acetylcysteine with prednisolone reduced 1-month mortality (8 % vs. 24 %) and the incidence of hepatorenal syndrome and infection [100]. The favorable safety profile of N-acetylcysteine makes it a potential option, in combination with corticosteroids, for patients with severe disease. There is a clear need to develop novel targeted therapies for patients not responding to existing drugs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







