This article explores in detail the issue of the alleged decline in semen quality. The impetus for a comprehensive re-evaluation at this time is threefold: (1) the potential impact of a real decline in semen quality and subsequent human fertility is a priori critical to human welfare; (2) governments have begun to enact “anti-endocrine disruptor” legislation that is based, in part, on selected portions of the published data about semen quality; and (3) confusion and misinformation about semen quality remain widespread in lay and professional circles.
Much has been made in the medical and lay literature of an alleged decline in human sperm counts worldwide. More than 100 articles have appeared in the peer-reviewed literature in the past 50 years on this topic. As discussed in more detail later, these articles vary widely in the quality of their methodology and their fundamental results. Most studies have found no decline, an increase, or mixed results in assessing changes in sperm parameters. A few studies have shown an unambiguous decline. It is from the latter studies, however, that the lay media and various advocacy groups have drawn the “findings” supporting theories that purport to explain the “decline” in sperm counts. The primary theory supported by these groups is that minute environmental levels of chemicals acting as “hormone mimics” or “endocrine disruptors” are responsible for this alleged deterioration. The term “endocrine disruptor” refers to chemical substances that exhibit some degree of estrogen-like activity. Although there is no question that estrogenic compounds can be potent modulators of biochemical and physiologic function in high doses, the implication that in utero or adult exposure to low levels of environmental “endocrine disruptors” produces clinically detectable effects in humans is highly uncertain.
Data from the handful of peer-reviewed articles showing a decline in sperm counts and other semen parameters have been quoted often enough in the media and even among researchers that this “fact” has achieved the quality of a paradigm. A dispassionate review of the research to date, however, firmly repudiates not only the alleged connections between “endocrine disruptors” and declines in semen quality but also the declines themselves. Far from being a worldwide and well-proved phenomenon, declines in semen quality are, at best, a highly local phenomenon with an unknown cause and, at worst, a collective artifact arising from the observation of a highly variable physical attribute (sperm counts) with a relatively low-resolution tool (retrospective analysis of nonrandomized study populations).
This article explores in detail the issue of the alleged decline in semen quality. The impetus for a comprehensive re-evaluation at this time is threefold: (1) the potential impact of a real decline in semen quality and subsequent human fertility is a priori critical to human welfare; (2) governments have begun to enact “anti-endocrine disruptor” legislation that is based, in part, on selected portions of the published data about semen quality; and (3) confusion and misinformation about semen quality remain widespread in lay and professional circles.
Sources of error
At first blush, it might seem almost trivial to obtain for semen quality the same type of widely accepted physiologic norms that have been determined for other bodily fluids and functions, such as blood or blood pressure. A host of difficulties conspire to make semen the least well understood bodily fluid, however, in terms of the distribution of its normal parameters in the general population. Obtaining human semen for scientific analysis is logistically difficult. As many authors have pointed out, the fact that semen is almost universally obtained by masturbation has placed profound limits on the ability of researchers to adequately study this issue. If collection of semen samples were as straightforward as obtaining blood samples, the nature of semen quality changes over time (if any) would have been determined decisively decades ago. A prospective, longitudinal study of semen parameters in a large, multicenter, randomized study of community-dwelling men, although time-consuming and expensive, would provide highly reliable data. Of nearly equal quality would be an analysis of a suitably sized population of randomly selected community-dwelling men analyzed by birth cohort. Unfortunately, neither of these high-quality observational tools has been used to investigate the phenomenon of semen quality because of the logistical and emotional obstacles posed by the means of obtaining semen in a timely and well-controlled manner.
Researchers in the past 50 years have studied populations of men who have provided semen samples for reasons such as donation to sperm banks, evaluation for male factor infertility, prevasectomy evaluation, infertility evaluation for a couple, and donation for use with assisted reproductive techniques, such as in vitro fertilization or intracytoplasmic sperm injection. None of these populations represents a random sample of the population at large, and each presents a selection bias, although some of these study populations are more likely to be biased than others. For example, men who provide semen samples as part of a couple’s infertility evaluation in which the female partner is later determined to be the source of the infertility could plausibly be considered nearly representative of the general male population because their inclusion for testing is unrelated to the semen donor’s potential fertility. Other types of male study populations are more likely to be biased, however. Semen donors, for example, may have been screened for problems known to affect fertility or may have been selected precisely because a prior semen analysis showed a robust fertility. Male donors to in vitro fertilization or intracytoplasmic sperm injection programs are more likely than normal to have low fertility, regardless of the fertility status of their partner.
The lack of truly randomized, community-dwelling study populations has posed fundamental limits on our ability to say what is “normal” in terms of semen parameters and renders illegitimate any attempts to generalize from a particular study of semen or semen change over time to the male population at large.
Another source of potential error in studies of semen quality is the highly variable nature of the subject in question. Attributes such as sperm count, semen volume, and sperm morphology not only vary widely between individuals but also vary widely within individuals. Semen quality is sensitive to the following variables:
- •
Abstinence time (the amount of time since the previous ejaculation). Longer abstinence times lead to higher sperm counts, higher semen volumes, and a higher percentage of sperm displaying abnormal morphology. In turn, abstinence time varies with such things as a man’s age, his current level of sexual activity, and his general health.
- •
Scrotal temperature. The Sertoli cells of the testicles are temperature sensitive and must be several degrees cooler than normal body temperature to function properly. Anything that either temporarily or chronically raises scrotal temperature can depress semen quality . Such phenomena as fever, hot tubs, exposure to high-temperature working conditions, and occupations that require long periods of sitting have been shown to affect sperm quality.
- •
Season. Some, but not all, studies of semen quality have shown seasonal fluctuations in mean sperm counts, with averages highest in springtime and lowest in summer .
- •
Smoking. Chronic smokers show a 13% to 17% decline in sperm counts, according to a meta-analysis of 20 studies . Variations in the incidence of smoking between regions or over time may alter mean sperm counts.
- •
Marijuana use. Various animal, in vitro, and human studies have demonstrated deleterious effects on sperm parameters—including sperm counts—of tetrahydrocannabinol and chronic use of marijuana . Changing regional or temporal trends in the use of marijuana may be a confounding factor in studies of semen quality.
An additional factor that has yet to be explained adequately contributes to the difficulties of scientifically determining population norms for semen and assessing any changes to those norms over time. Semen parameters have been repeatedly shown to vary significantly with geographic region. Even careful studies using identical laboratory methods on similar populations of men recruited for similar reasons have found this effect. For example, a study of 1283 men from three regions of the United States found a mean sperm concentration in California of 72.7 × 10 6 sperm/mL, whereas the mean concentration in Minnesota was 100.8 × 10 6 sperm/mL, and in New York it was 131.5 × 10 6 sperm/mL . As demonstrated in the following sections, failure to take such variation into account can completely invalidate studies of semen characteristics.
Studies of semen quality have been hampered by three fundamental sources of potential error: inability to study a truly random population of community-dwelling men, wide inherent inter- and intrasubject variation in semen parameters, and wide and unpredictable geographic variations in semen quality. The authors of the best studies of semen quality in the past 50 years are cognizant of some or all of these potential sources of error. Some studies, for example, have attempted to control for variables such as abstinence time or have chosen subjects only from the subpopulations of men that are least likely to be biased in comparison to the population at large. Many studies have not taken these potentials sources of error into account, however. The failure to address such errors in some studies has been compounded by additional methodologic or statistical errors.
A flawed pivotal study
Before 1992, several small-scale or regional studies of men seeking medical help for infertility suggested a decline in sperm counts or other semen parameters in primarily European countries . In the same period, however, a large US study found no decline in semen parameters . The divergence in the results of these studies remained a topic of professional discussion and debate during these years but did not reach a wider audience. This thinking changed with the publication in 1992 of a paper by Elisabeth Carlsen and two colleagues from the University of Copenhagen, Denmark . Entitled “Evidence for decreasing quality of semen during past 50 years,” this meta-analysis of 61 previous studies gained worldwide media attention. The attention was caused by the surprising magnitude of the findings (a nearly 50% drop in sperm count from 113 × 10 6 /mL in 1940 to only 66 × 10 6 sperm/mL in 1990) and the fact that the authors suggested a cause for the decline: “compounds with estrogen-like activity or other environmental or endogenous factors.” This study’s findings dovetailed with pre-existing concerns in many quarters about the potential hazards of environmental pollutants, such as herbicides, pesticides, and chemical contamination of all sorts. Although the relevant medical community reacted quickly to the paper with skepticism about its results and criticism of its methodologies, the popular interpretations of the study were unreserved, and subsequent critiques in the medical literature received little, if any, popular notice. As a result, the Carlsen paper has had an impact on the popular imagination and mindset of many environmental advocates that is far out of proportion to its actual scientific value. I argue that the paper has no scientific value. Its primary importance is that it acted as a stimulus for more careful researchers to explore the complex issue of semen quality.
Although the Carlsen paper already has been thoroughly “discredited in a number of professional articles” , its stature as a pivotal study warrants a summary of its major weaknesses:
- •
Variability across the 61 studies in the methods and protocols used for sperm collection and measurement
- •
Inability to control for period of abstinence in study subjects
- •
Inability to control for lifestyle factors, such as cigarette smoking or recreational drug use
- •
Failure to include studies that were available and conducted within the time period of the meta-analysis that fail to show a decline or report sperm concentrations higher than other studies included in the meta-analysis from the same time period
- •
Failure to account for geographic variation among studies (Of the studies from before 1970, all were from the United States, and 80% of these were from New York, where sperm counts (then and now) are the highest. After 1970, only three studies were from the United States, and many were from third-world countries, where sperm counts were low. A reanalysis of the Carlsen meta-analysis that accounts for this geographic variation shows no decline in sperm counts [ Fig. 1 ].)
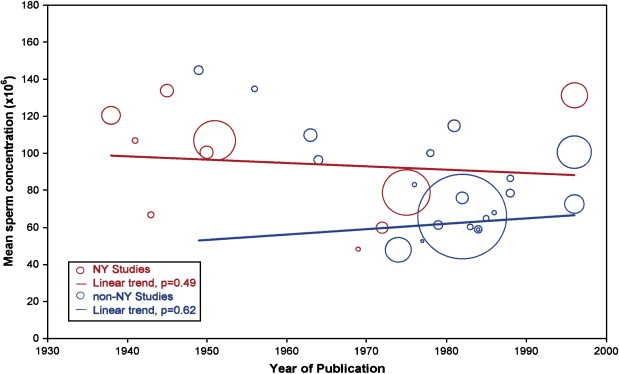
Fig. 1
Re-analysis of data from Carlsen et al shows no decline in sperm counts ( blue regression line ) when data from New York are excluded. Bubble size corresponds to number of men in study. ( From Saidi J, Chang D, Goluboff E, et al. Declining sperm counts in the United States? A critical review. J Urol 1999;161:460–2; with permission.)
- •
Use of an inappropriate statistical analysis. A comprehensive statistical reanalysis of the Carlsen study showed that the linear regression model used was inappropriate because the data distribution was highly nonuniform—most data were collected between 1970 and 1990. When quadratic or spline regression models were used (even when the data were uncorrected for geographic variation) the data show mean sperm counts increasing since 1940.
Any of these weaknesses alone would serve to cast the results of a scientific study in doubt. Taken together, they justify a deep skepticism regarding the Carlsen study and a removal of the study from consideration in any review of evidence supporting a decline in sperm counts or other semen parameters.
A flawed pivotal study
Before 1992, several small-scale or regional studies of men seeking medical help for infertility suggested a decline in sperm counts or other semen parameters in primarily European countries . In the same period, however, a large US study found no decline in semen parameters . The divergence in the results of these studies remained a topic of professional discussion and debate during these years but did not reach a wider audience. This thinking changed with the publication in 1992 of a paper by Elisabeth Carlsen and two colleagues from the University of Copenhagen, Denmark . Entitled “Evidence for decreasing quality of semen during past 50 years,” this meta-analysis of 61 previous studies gained worldwide media attention. The attention was caused by the surprising magnitude of the findings (a nearly 50% drop in sperm count from 113 × 10 6 /mL in 1940 to only 66 × 10 6 sperm/mL in 1990) and the fact that the authors suggested a cause for the decline: “compounds with estrogen-like activity or other environmental or endogenous factors.” This study’s findings dovetailed with pre-existing concerns in many quarters about the potential hazards of environmental pollutants, such as herbicides, pesticides, and chemical contamination of all sorts. Although the relevant medical community reacted quickly to the paper with skepticism about its results and criticism of its methodologies, the popular interpretations of the study were unreserved, and subsequent critiques in the medical literature received little, if any, popular notice. As a result, the Carlsen paper has had an impact on the popular imagination and mindset of many environmental advocates that is far out of proportion to its actual scientific value. I argue that the paper has no scientific value. Its primary importance is that it acted as a stimulus for more careful researchers to explore the complex issue of semen quality.
Although the Carlsen paper already has been thoroughly “discredited in a number of professional articles” , its stature as a pivotal study warrants a summary of its major weaknesses:
- •
Variability across the 61 studies in the methods and protocols used for sperm collection and measurement
- •
Inability to control for period of abstinence in study subjects
- •
Inability to control for lifestyle factors, such as cigarette smoking or recreational drug use
- •
Failure to include studies that were available and conducted within the time period of the meta-analysis that fail to show a decline or report sperm concentrations higher than other studies included in the meta-analysis from the same time period
- •
Failure to account for geographic variation among studies (Of the studies from before 1970, all were from the United States, and 80% of these were from New York, where sperm counts (then and now) are the highest. After 1970, only three studies were from the United States, and many were from third-world countries, where sperm counts were low. A reanalysis of the Carlsen meta-analysis that accounts for this geographic variation shows no decline in sperm counts [ Fig. 1 ].)







