Continent Ileostomy
Victor W. Fazio
Myles R. Joyce
Introduction
The continent ileostomy (K-pouch) emerged in response to patient’s desire to avoid an end ileostomy. Patients cited difficulties with leakage; others complained of psychological and body image problems with application of an external device. The planned intermittent evacuation of the continent ileostomy provided a significant improvement in quality of life for motivated patients. However, the popularity for formation of this internal reservoir attenuated with the emergence of ileal pouch-anal anastomosis (IPAA) as the gold standard when desiring restoration of intestinal continuity and continence (1,2). The ileal pouch allows restoration of the normal defecatory pathway. Thus, K-pouch formation is now mainly confined to a few specialized centers. In essence, it is an internal reservoir that stores intestinal contents. It has a nipple valve that prevents leakage of gas and feces. The stoma aperture should be flushed with the skin. It is emptied by interval intubations of the pouch using a soft plastic tube. Since its original description by Nils Kock in 1969 (3), there have been several modifications principally directed at stabilization of the nipple valve.
Most patients who have a continent ileostomy are extremely satisfied with the quality of life it offers and are willing to undergo multiple revisions if it avoids returning to a conventional ileostomy (4). However, it is an operation that should not be entered into lightly by the patient and the surgeon as it is technically challenging, utilizes 40–60 cm of small bowel for construction, requires significant maintenance, and leaves the patient prone to potential fluid and electrolytic disturbances if the reservoir requires subsequent removal.
Indications and Contraindications for Continent Ileostomy Formation
Current indications for formation include patients requiring total proctocolectomy (TPC) with sphincter dysfunction who wish to avoid an end ileostomy; patients with an existing ileostomy who wish to convert to an internal reservoir; patients in whom excision of the sphincter complex is required as part of an oncological resection (selected
patients); and those with a failed pouch in whom salvage pouch surgery (redo pouch) is not feasible or has a low potential for success. Converting a failing ileal pouch to a K-pouch theoretically ensures bowel preservation. In addition, we counsel patients undergoing a planned IPAA of this alternative option if reach is going to be an issue, despite the use of all techniques to ensure that the ileal pouch reaches the anal canal in a tension-free manner. We are particularly conscious of this problem in patients undergoing salvage pouch surgery for pelvic sepsis, tall male patients, and those with a foreshortened mesentery. Patients considering a continent ileostomy should be carefully counseled preoperatively as to the inherent risks and understand that a conventional end ileostomy is associated with fewer problems. Ideally, they should be provided with the option of speaking to patients who have had both a good and a bad result from K-pouch formation. However, it is our experience that the majority of patients, who seek a K-pouch have researched all aspects of care and potential complications. A significant proportion of work in the Cleveland Clinic, Ohio, consists of K-pouch revisions principally for nipple valve dysfunction, which despite improvements remains the Achilles’ heel of the procedure.
patients); and those with a failed pouch in whom salvage pouch surgery (redo pouch) is not feasible or has a low potential for success. Converting a failing ileal pouch to a K-pouch theoretically ensures bowel preservation. In addition, we counsel patients undergoing a planned IPAA of this alternative option if reach is going to be an issue, despite the use of all techniques to ensure that the ileal pouch reaches the anal canal in a tension-free manner. We are particularly conscious of this problem in patients undergoing salvage pouch surgery for pelvic sepsis, tall male patients, and those with a foreshortened mesentery. Patients considering a continent ileostomy should be carefully counseled preoperatively as to the inherent risks and understand that a conventional end ileostomy is associated with fewer problems. Ideally, they should be provided with the option of speaking to patients who have had both a good and a bad result from K-pouch formation. However, it is our experience that the majority of patients, who seek a K-pouch have researched all aspects of care and potential complications. A significant proportion of work in the Cleveland Clinic, Ohio, consists of K-pouch revisions principally for nipple valve dysfunction, which despite improvements remains the Achilles’ heel of the procedure.
Contraindications to continent ileostomy formation include patients who have lost a significant proportion of small bowel from preceding surgery, those with recrudescent Crohn’s disease, those with psychological problems, and those who are excessively obese. Obese patients often have a shortened, thickened mesentery, which is a problem when creating the nipple valve and is a risk factor for valve slippage. In addition, the increased abdominal girth gives problems with reach when creating the exit conduit. The presence of intra-abdominal desmoid disease in patients with familial adenomatous polyposis (FAP) is also a contraindication.
The technique and pouch design for K-pouch construction often varies among institutions and depends on whether one is forming a de novo pouch following TPC or whether one is converting an existing failed pouch to continent ileostomy. The majority of techniques have evolved with time. The overall goal is to create a functional reservoir with an eventual capacity of 500–1,000 ml, which is continent to gas and feces. The exit conduit should be easily intubated to empty reservoir contents. CT enterography will help to exclude proximal small-bowel Crohn’s disease, especially in patients with indeterminate colitis.
The patient requires marking by the surgeon or an experienced enterostomal therapist. In contrast to an end ileostomy, the stoma may be placed relatively low in the abdomen. The chosen site is most often below the belt line and above the pubic hairline, as when successful it does not require an external appliance. The patient is either placed supine or in a modified lithotomy position depending on the indication for surgery. Ureteric catheters are placed in patients undergoing redo pelvic surgery where we insert ureteric stents. In patients with an existing K-pouch undergoing salvage surgery the K-pouch is emptied of all contents. This measure reduces the potential for intraoperative spillage when mobilizing or opening the pouch, which is risky as the pouch wall is generally very thin.
Surgical Technique
The abdomen is entered via a lower midline laparotomy incision taking care to avoid enterotomies. In patients with preceding surgery and dense adhesions, hydrodissection may be required to identify tissue planes, reducing potential for enterotomies. The traditional technique for pouch construction used two 12–15-cm loops of terminal ileum.
An additional 15 cm of ileum was used distal to the pouch with 12 cm used for nipple valve intussusception and remainder was used to construct the exit conduit. The bowel loops are aligned in a U-shaped fashion with approximation of the antimesenteric borders performed using continuous 2-0 chromic catgut or polyvinyl suture (5). The limbs are then opened on the antimesenteric borders with the posterior wall constructed using a second layer of continuous absorbable suture to approximate the mucosa (Fig. 42.1).
An additional 15 cm of ileum was used distal to the pouch with 12 cm used for nipple valve intussusception and remainder was used to construct the exit conduit. The bowel loops are aligned in a U-shaped fashion with approximation of the antimesenteric borders performed using continuous 2-0 chromic catgut or polyvinyl suture (5). The limbs are then opened on the antimesenteric borders with the posterior wall constructed using a second layer of continuous absorbable suture to approximate the mucosa (Fig. 42.1).
The authors favor an S-shaped reservoir, which requires the addition of a third limb (Fig. 42.2) (6). In considering the S-pouch design, we believe that separating the afferent limb from the exit conduit allows for easier pouch rotation if needed in the future. We devote 20 cm of the terminal ileum to the nipple valve and exit conduit. Intussuscepting 12 cm of the efferent limb gives a 6 cm valve with 8 cm remaining for the exit conduit. Similar to the U-shaped design the three limbs are opposed with seromuscular sutures, bowel is opened on the antimesenteric border, and mucosal approximation is completed (Fig. 42.3 A and B).
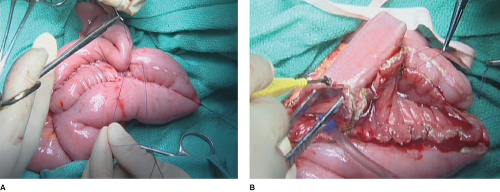 Figure 42.3 A. Aligning the three limbs of the S-pouch. B. Opening the aligned loops on the antimesenteric border. |
It took Nils Kock several years and some modifications before discovering that intussusception of a component of the exit conduit achieved continence. In the original design no valve was created and later attempts involved mobilizing the rectus abdominus muscle to produce functional obstruction. The original technique for keeping the valve intussuscepted consisted of inserting several rows of sutures through the two limbs over a Hegar’s dilator. There have been several modifications since including the Barnett continent ileostomy (7). The authors’ technique consists of intussuscepting a portion of the exit conduit using a Babcock forceps, to create the nipple valve, which is approximately 6 cm in length. Prior to intussusception the peritoneum of the efferent limb is stripped from its adjacent mesentery, which may also be defatted using electrocautery. This reduces its bulk and improves the ability to intussuscept the future valve.
The critical step then involves stabilization of the valve, which the authors perform using three to four applications of a transverse stapler (reusable PI 55, Covidien, Norwalk, CT) (Fig. 42.4 A and B) (8). The pin must be removed from the stapler as if left in place it will likely give rise to a fistula. Care must be taken not to damage the blood supply to the nipple. The anterior portion of the pouch is then closed starting at the apex of the nipple valve. The authors use 2/0 Vicryl sutures and incorporate the anterior portion of the nipple valve in the initial part of the anterior closure. When the anterior closure reaches the apex of the nipple valve we provide further stabilization by the application
of an additional fire of the transverse stapler over the sutured layer (Fig. 42.5). Anterior closure of the pouch is then completed. A silicone catheter tube is then inserted into the pouch and the capacity plus valve integrity is tested (Fig. 42.6



of an additional fire of the transverse stapler over the sutured layer (Fig. 42.5). Anterior closure of the pouch is then completed. A silicone catheter tube is then inserted into the pouch and the capacity plus valve integrity is tested (Fig. 42.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




