Condition
Examples
Unstable coronary syndromes
Unstable or severe angina (CCS class III or IV)a
Recent MIb
Decompensated heart failure (NYHA functional class IV; worsening or new-onset HF)
Significant arrhythmias
High-grade AV block
Mobitz II AV block
Third-degree AV block
Symptomatic ventricular arrhythmias
Supraventricular arrhythmias (including atrial fibrillation) with uncontrolled ventricular rate (HR > 100 bpm at rest)
Symptomatic bradycardia
Newly recognized ventricular tachycardia
Severe valvular disease
Sever aortic stenosis (mean pressure gradient greater than 40 mmHg, aortic valve area < 1.0 cm2, or symptomatic)
Symptomatic mitral stenosis (progressive dyspnea on exertion, exertional presyncope, or HF)
In the absence of serious comorbidities, a rough assessment of exercise tolerance may be all that is needed to determine if further testing should be pursued. This is especially true when taken in context of the type of surgery you are performing. Anorectal surgery is considered a low-risk operation, regardless of anesthetic technique, and elective abdominal operations are considered intermediate risk operations. Age, as a sole criterion, defines only the need for EKG and chest X-ray for patients over 50. Advanced age alone is not an indication for further cardiac testing. In fact, for patients with good exercise tolerance (>4 METS) (Table 25.2) [2], further testing for any elective procedure is usually unnecessary.
Table 25.2
Estimated energy requirements for various activities
Metabolic equivalent (MET) | Activity |
|---|---|
1 MET | Eat, dress, use the toilet |
Walk indoors around the house | |
Walk a block or 2 on level ground at 2–3 mph? | |
4 MET | Do light housework (dusting, washing dishes) |
Climb a flight of stairs or walk up a hill? | |
Walk on level ground at 4 mph? | |
Run a short distance | |
Do heavy housework (scrubbing floors, lifting/moving furniture) | |
Participate in moderate recreational activities (golf, bowling, dancing, double tennis, baseball or football catch) | |
>10 METS | Participate in strenuous sports (swimming, single tennis, football, basketball, skiing) |
Other significant clinical risk factors should be assessed. A history of ischemic heart disease, compensated or prior CHF, diabetes mellitus, renal insufficiency, or cerebrovascular disease all represent significant comorbidities that may require preoperative evaluation.
Exercise tolerance is an excellent overall assessment of fitness. In the setting of good exercise tolerance, even with multiple clinical risk factors described above, intermediate risk surgery can often be undertaken with acceptable risk. Perioperative heart rate control with beta-blockade should be considered mandatory in anyone with any of the above risk factors, since this has been shown to reduce cardiac morbidity and mortality [3].
When a patient has some of these other significant comorbidities, specific workup may be indicated as per the AHA guidelines [2]:
Pulmonary Disease
The presence of restrictive or obstructive pulmonary disease significantly increases the risk of perioperative pulmonary complications. In these cases, preoperative pulmonary testing to determine volume and diffusion capacity, response to bronchodilators, and a baseline blood gas will help guide postoperative therapy.
Diabetes Mellitus
This is the most common metabolic disease associated with advanced age and is often associated with coronary disease. The presence of insulin-dependent DM increases the risk of perioperative myocardial ischemia and heart failure. Careful attention (both intraoperatively and postoperatively) to glucose management with insulin infusions and tight glycemic control has been found to significantly reduce postoperative wound infection in CABG patients, and this paradigm can be applied to major abdominal surgery.
Renal Failure
Renal failure is associated with an increased risk of perioperative cardiac morbidity [4]. In addition, preoperative levels of creatinine >1.5–2 mg/dl is associated with an increased risk of postoperative renal failure, cardiac complications, and increased mortality.
Hematologic Disorders
Preoperative anemia can impose cardiac stress, worsen ischemia, and exacerbate preexisting CHF. In one study looking at patients undergoing prostate and major vascular surgery, a hematocrit <28 % was associated with an increased risk of perioperative ischemia and postoperative complications.
Anorectal Problems
Key Concept: In any patient with anorectal complaints, baseline function of the sphincter complex should be taken in to account when considering surgical options.
Examining and documenting sphincter tone and determining whether alterations in continence are present are imperative when evaluating older patients with anorectal complaints. Laurberg showed that in the elderly, there is significantly decreased baseline sphincter tone [5], decreased rectal sensation and distensibility, and increased perineal laxity in women [6]. Unfortunately, there has been no data showing any consistently reproducible predictive factors for postoperative changes in continence based on preoperative examination or physiologic testing.
Yet, there are some major points you should keep in mind when evaluating older patients with anorectal complaints:
(a)
When considering hemorrhoidectomy in the elderly, as with younger patients, initial management should be conservative when possible.
(b)
In the elderly, anorectal complaints are often centered on mucus seepage and soilage. Though dietary changes, bowel management (i.e., fiber, Imodium), and skin protection are successful first-line treatments, in most cases, patients with prolapse or large hemorrhoids will likely benefit from surgery.
(c)
In our experience, the best predictor of postoperative function after surgery is preoperative function.
(d)
A careful history, with special attention to bowel habits and continence, is crucial. If preoperative soilage or seepage is the major complaint, it is important to ascertain whether this is due to mucosal prolapse or true sphincter dysfunction.
Fecal Incontinence (FI)
Key Concept: FI occurs much more commonly than thought. While a full evaluation is helpful, most often by simply focusing on medical management in the elderly patient, you will provide the most benefit.
Fecal incontinence (FI) is a socially disabling disorder, which is far more prevalent in the elderly. Estimates at the rate of FI ranged from 2 to 17 % in a community setting, but these are likely underreported. A more recent HMO-population based study found reported rates of FI as high as 36 %. In the elderly, rates of FI are significantly higher, especially in the nursing home setting, where rates range from 33 % to as high as 65 % [7].
Management of FI depends on the etiology. A complete history, focusing on the details of bowel habits, diet and medication, as well as prior anorectal surgical and obstetric history, will often elucidate the etiology of the disorder and guide treatment. In the elderly, the differential diagnosis is quite long, including cognitive and neurologic diseases, chronic constipation with overflow, senescent physiologic changes, rectal prolapse, or iatrogenic or obstetric injury. Treatment is almost always geared towards the underlying condition, and optimization of bowel habits is crucially important in this population. It is also important to protect the perineal skin, as seepage of intestinal contents can often lead to severe maceration and breakdown if not properly attended too.
Rectal Prolapse
Key Concept: Procidentia, or true rectal prolapse, when encountered as an etiology for FI, is probably best treated surgically with a perineal approach.
Oftentimes, patients with FI will have diminished sphincter control due to long-standing (and previously unreported and undiagnosed) full-thickness rectal prolapse (Fig. 25.1). We advocate a perineal proctectomy in the elderly as this is well tolerated and avoids the morbidity of an abdominal operation (Fig. 25.2). In patients with significant comorbidities, it can even be performed under a spinal anesthetic or in the left lateral decubitus position to minimize intraoperative complications.

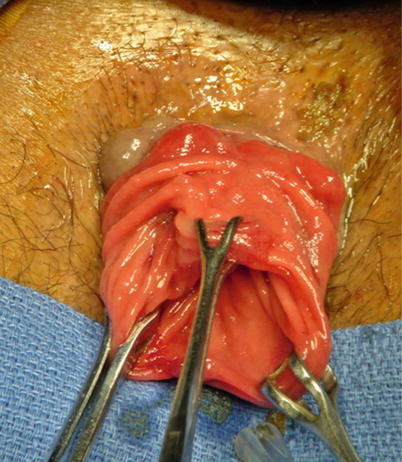

Fig. 25.1
Full-thickness rectal prolapse
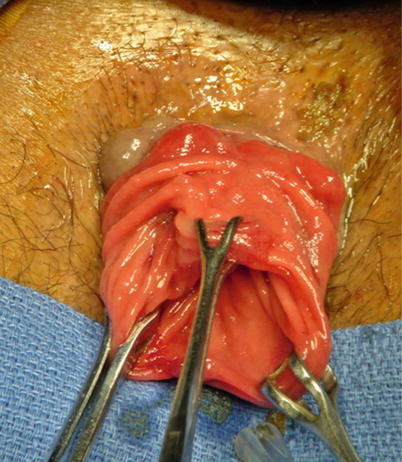
Fig. 25.2
Perineal approach to rectal prolapse
Sacral Nerve Stimulation (SNS)
Key Concept: SNS has an evolving role in FI for failed medical management and with its good preliminary results and trial period to confirm efficacy, may soon be a first–line treatment modality in this cohort.
Ultimately, symptoms of FI should be managed conservatively when possible. Considerations for surgery in the elderly have changed significantly in recent times. Historically, once conservative measures and biofeedback fail, and the patient was considered a suitable candidate for surgery, few options remained. Often, in men with profound FI, in the absence of a sphincter injury, fecal diversion remained the only option. In women with known sphincter injuries, sphincteroplasty was an option. However, this is a significantly morbid procedure with a difficult recovery and has fairly poor long-term results. More recently, the paradigm has undergone a significant shift. Sacral nerve stimulation, a modality that has had a decade of known efficacy in urinary incontinence, was recently approved for use by the FDA for fecal incontinence (Fig. 25.3). The indication included fecal incontinence in the presence of known sphincter injuries of up to 60°. Although the efficacy of SNS in treating FI has been known since it has been used for urinary incontinence for more than a decade, it was not until 2011 when the FDA finally approved FI as an independent indication for treatment. The initial studies showed significant success rates, defined as at least a 50 % reduction in fecal incontinence symptoms, in 60–100 % of patients. In the initial publication of the SNS study group, 133 patients underwent test simulation with a 90 % success rate. Even at 3 years of follow-up, 86 % of patients reported a greater than 50 % reduction in the number of incontinent episodes per week, and perfect continence was achieved in 40 % of the patients [8].


Fig. 25.3
Sacral nerve stimulation (SNS). Needle finding the correct sacral level
There are several advantages of this new approach – it is low risk, with a reported infection rate of less than 10 %, and no major morbidities reported. It works even in patients with sphincter defects, so that there is no further need to subject them to high risk of morbidity and poor long-term results with sphincteroplasty. Finally, because there is a test phase built into the implantation process, patients will know whether or not it works before they ever have a permanent implant placed. We suspect that this will have a long-term effect on the paradigm of treatment for fecal incontinence and that sacral nerve stimulation will become first-line therapy after conservative measures and behavioral modification have failed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








