Fig. 24.1
(a, b) The Bascom cleft lift procedure. Compressing the buttocks together will allow marking of the diseased area and deep cleft that will require excision (Courtesy of Dr. Bascom)
You may find yourself saying “Okay, so what?” First, pilonidal disease is a common problem seen in a colorectal surgical practice. Most of the time, these patients are referred from internal medicine, family practice, dermatologists, and general surgeons for evaluation and treatment, in part, because of frustration with recurrent disease and also due to its chronic nature and/or the failure of either conservative and/or prior surgical therapy. Many patients have been treated with antibiotics, an in-office incision and drainage, or even pilonidal cystectomy. They are also just as frustrated because of the intermittent infections or chronic draining sinus that limits their activity, whether it is purulent or blood and foul odor. The majority of these patients are in the second decade of life: they are often now in college and have been dealing with pilonidal disease since high school, and it’s not getting better. You, the true (or deemed) “colorectal specialist” are then confronted with a disgruntled patient and a benign disease that has become a social nuisance to them. I have a very long discussion with these patients (and their parents) about the different surgical approaches to this disease; many are familiar with these therapies—through family members, other patients, and in many cases online research. They usually want to schedule their surgery during spring or summer break, because they do not want to interrupt their education or externships for an operation.
My Approach (Dr. Orangio)
I recommend to these patients re-excision and the utilization of the VYAF, for several reasons: (1) they have a limited window for surgery and postoperative wound care; (2) they do not have the “privacy” or “facilities” or “personal” support to manage an open pilonidal wound that requires packing when they return to school; (3) they want minimal discomfort and the shortest recovery time. These patient criteria are the reason to offer this younger patient population and alternative to pilonidal cystectomy and secondary wound healing. They must be counseled about the “scarring” that remains post-VYAF because it is significant.
A Case of Recurring Draining Sinuses
A 26-year-old male with a 10-year history of pilonidal disease presented with a previous incision and drainage of pilonidal abscesses and now with multiple residual draining pilonidal sinuses. My approach is to place all patients in the prone jackknife position and use general anesthesia with intravenous antibiotics (second- or third-generation cephalosporin). The gluteal cleft and gluteal areas are shaved bilaterally and prepped utilizing povidone. On examination, this patient has complex disease with multiple deep midline and lateral sinus tracts. I mark the excision site prior to beginning (Figs. 24.2 and 24.3).



Fig. 24.2
Recurrent pilonidal disease with extensive midline tunneling and lateral tracts

Fig. 24.3
Excision boundaries for recurrent pilonidal disease
An elliptical incision was performed with en bloc excision of all sinus tracts and scar, leaving a wound that is to the left of midline and down to the presacral fascia (Fig. 24.4). Although some surgeons prefer to keep the base of the ulcer in place, I feel this is a chronic wound and should be removed. The site for the V–Y advancement flap (VYAF) is marked and measured: 12 cm long and 10 cm wide (Fig. 24.5). The flap is dissected down to the level of the gluteal fascia, but not including the gluteal fascia. Then the medial and lateral portions of the flap are then dissected from the gluteal fascia leaving at least a 4–5 cm “vascular pedicle” (Figs. 24.6 and 24.7). It is important here not to cone in and ensure you are keeping your flap of equal and proper thickness to avoid any devascularized areas. Remember this will need to move, so adequate dissection and mobilization without compromising blood supply is key. With the vascular pedicle isolated, the VYAF can easily slide past the midline to allow for anchoring to the presacral fascia and to the contralateral wound margin, which is to the left of the midline. This will obliterate the infra-gluteal cleft and move the incision off of the midline to aid in healing (Figs. 24.8 and 24.9). Check the viability of the flap again. Ensure it is healthy at this stage or not under tension that you can still rather easily do something about. The margins of the wound and VYAF are approximated with subcuticular absorbable sutures and a “fluff” dressing is applied (Figs. 24.10, 24.11, and 24.12). I do not use drains, although some people like to use them to evacuate the fluid that may collect early on. The patient remains in the hospital for 24–48 h and is encouraged not to lie on their back and to sit up straight while sitting and eventually while driving. The patient is discharged and followed up in 10, 30, and 60 days postoperatively.


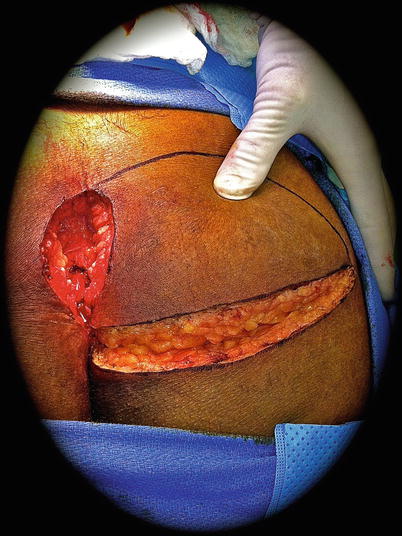
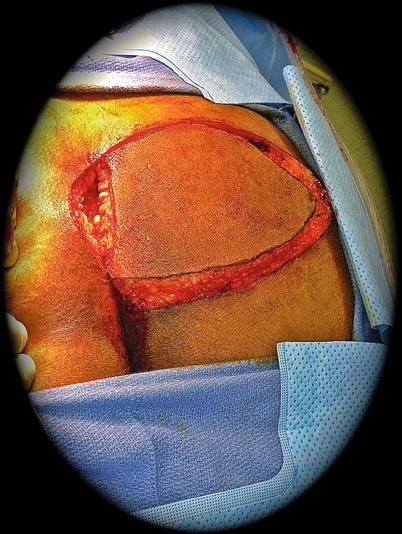
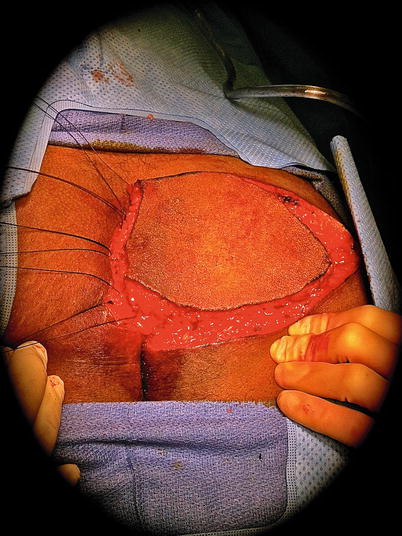

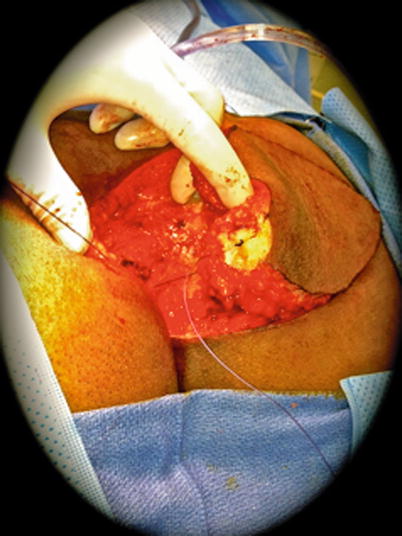
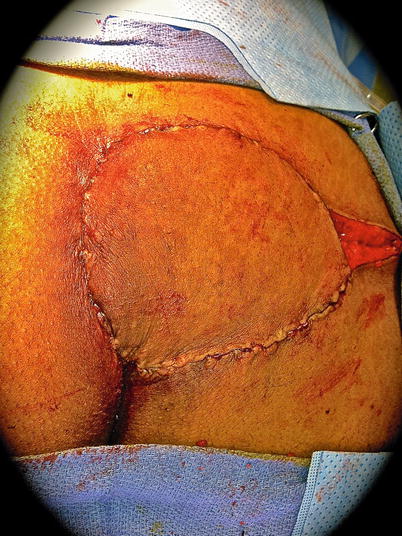


Fig. 24.4
Defect following excision of recurrent disease

Fig. 24.5
Measuring out the dimensions for the V–Y advancement flap
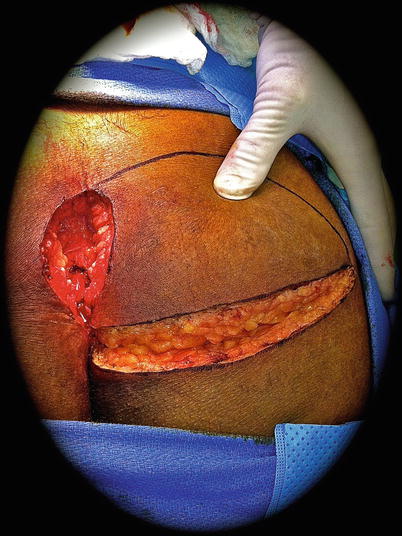
Fig. 24.6
Constructing the V–Y pedicle
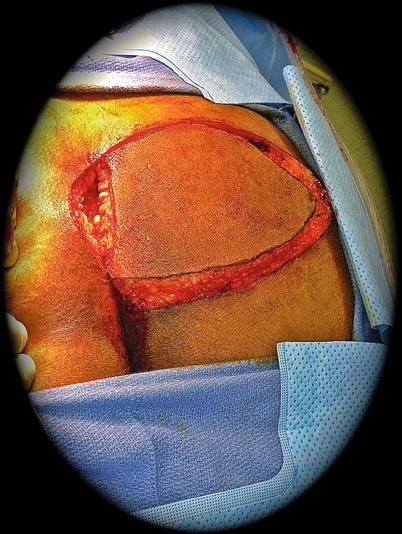
Fig. 24.7
Completed well-vascularized pedicle. Note the thickness of the pedicle
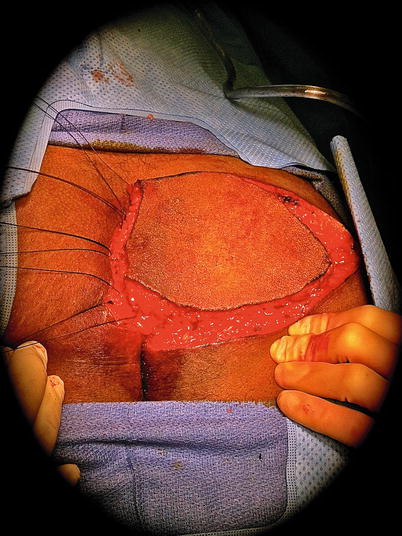
Fig. 24.8
Anchoring sutures in place

Fig. 24.9
Pedicle able to slide past the midline to obliterate the cleft
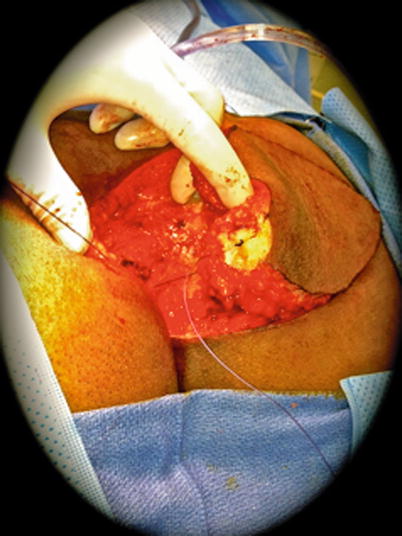
Fig. 24.10
Deep and subcuticular sutures in place on the flap
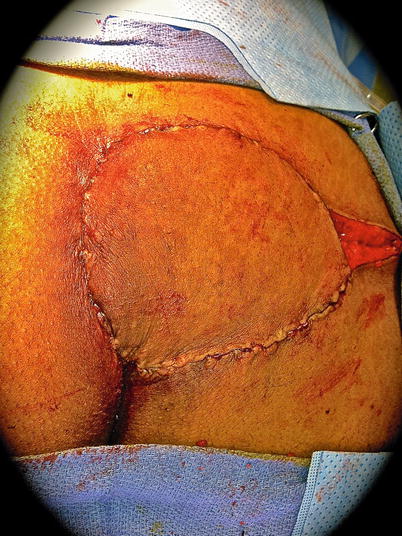
Fig. 24.11
Pedicle sutured in place leaving only the lateral defect

Fig. 24.12
Completed pedicle
Healing by Secondary Intention (Dr. Abcarian)
Key Concept: Healing by secondary intention has the benefit of lower recurrence rates but requires effort and time on both you and your patient for successful eventual healing.
Surgeons generally desire healing of all wounds in the earliest possible time. This is the basis of primary closure of all surgical wounds. The problem with pilonidal cyst closure by any surgical technique is its relatively high failure rate. Why do closures after pilonidal cystectomy fail? This conundrum has plagued surgeons throughout the years. In the pre-antibiotics era, Kleckner surveyed the then American Proctologic Society® in 1936 and found a recurrence rate of 33 % [12]. In 1977, Eftaiha and Abcarian reviewed all the available literature on the subject and reported a recurrence rate of 34 %. Conversely, excision of pilonidal cyst and allowing healing by secondary intention had a recurrence rate of 3 % [13]. So it seemed that all available surgical techniques of closure and use of antibiotics had made no significant reduction in recurrence rates.
In his 1963 textbook, Gabriel listed several criteria where he believed a pilonidal cystectomy wound should not be closed due to high failure rate. These included previous closures, free discharge of pus, hirsutism, secondary openings off the midline, and cysts greater than 7.5 cm (Fig. 24.13) [14]. Even now, it seems unlikely that wide excisions, undermining skin flaps and technically complicated plastic closure (Z-plasty, V–Y advancement flaps, etc.), will yield generally lasting results in the presence of the patient-/disease-related criteria spelled out by Gabriel decades ago.


Fig. 24.13
Extensive pilonidal disease in a patient with multiple risk factors for recurrence
Other causes of recurrence (and in many cases persistence) following both primary closure and healing by secondary intention of these wounds include (A) inadequate eradication of all the midline pits, which is the source of pilonidal infection. In the case illustrated in the earlier section of this chapter by Dr. Orangio, one can clearly see intact midline pits (Fig. 24.2, which should have been previously eradicated) in addition to midline draining abscess and secondary opening to the left of and posterior to the prior surgical incision. (B) The lateral (horizontal) tension on the intergluteal cleft with a longitudinal midline incision and closure that is essentially unavoidable. This mechanical factor must also play a role in the failure of flaps, even despite good mobilization. We can try to overcome this by instructing the patient to remain less active after a flap closure, but certainly absolute bed rest with the potential for deep vein thrombosis and life-threatening or lethal pulmonary embolism must be condemned. (C) The wide and deep dissection of tissues required for both excision and construction of flaps in the presence of infection that increases the risk of failure secondary to localized sepsis. This unfortunately cannot be overcome by a short course of broad-spectrum antibiotics. In fact, prolonged use of these antibiotics predisposes to an ever-increasing incidence of antibiotic-related complications such as Clostridium difficile colitis. (D) Finally, obesity makes the management and care of the open wound difficult.
So what is wrong with leaving the wound open after pilonidal cystectomy? These wounds, irrespective of size, cause very little pain and disability, and I have found it generally easy to care for (bathing and packing a coarse 4 × 4 gauze to separate the edge and keep the wound dry). Changing of the gauze three to four times daily will debride the open wound and prevent collection of infected discharge in the cleft. I’ve found that the best way to dry the wound after bathing is the use of a hair dryer on the cool setting. The anatomic distance of these wounds from the anus allows for painless bowel movements, and patients are uniformly happier than those having undergone excisional hemorrhoidectomy.
In many cases the correct operation has been done. The cyst is completely excised without deepening the excision down to the sacrococcygeal fascia. A small 3 × 4 cm cyst excised in total will leave a 4 × 5 cm defect, while carrying the excision down to the fascia opens up and expands the wound by 50–100 % of the original size [13]. In some cases there are lateral tracts or pockets of disease that may require additional excision; however, these can often close just fine with secondary intention (Figs. 24.14, 24.15, and 24.16).




Fig. 24.14
Recurrent pilonidal disease (Courtesy of W. Brian Sweeney, MD)

Fig. 24.15
Resulting wound after excision (Courtesy of W. Brian Sweeney, MD)

Fig. 24.16
Wound after near-complete closure with secondary intention (Courtesy of W. Brian Sweeney, MD)
Open wounds begin the “picture frame” shrinkage 2 weeks postoperatively and will need to be inspected on regular biweekly basis. The surgeon must take time to shave all edges of the open wound to prevent growth of hair into the wound during the healing process (Fig. 24.17). Also as the wound becomes shallower, the dressing gauze must be inserted into the wound to prevent patchy adherence of the wound edges. This is easy to instruct the patient because the only painful area is the skin surrounding the defect and not the depth of the wound. Small wounds ~3 × 4 cm typically heal in 4–6 weeks, while larger ones such as 4 × 6 cm may need up to 8–10 weeks for complete healing. Application of antibiotics, astringents, or anesthetic ointments is not helpful and may actually contribute to maceration of the wound by adding moisture.


Fig. 24.17
The shaved wound after excision of the pilonidal disease
In 1977 Rosenberg recommended reverse taping to pull the wound edges laterally and flatten the deep wound in very obese patients [15]. Although logically sound, it is difficult for the patient to tolerate the constant pulling sensation and interference of reverse taping with ambulation and daily activities. The current use of wound VAC® (LifeCell, New Jersey) has essentially made this technique obsolete. Yet, wound VACs are also cumbersome and need nursing or wound care professionals to change the foam pads at least every 48–72 h (especially in that location). Despite these drawbacks, with utilization of portable suction machines, this has allowed the patient to be able to ambulate and even return to work (Figs. 24.18 and 24.19).



Fig. 24.18
Nonhealing pilonidal wound. Seton placed initially due to recurrent subcutaneous abscesses (Courtesy of Eric K. Johnson, MD)

Fig. 24.19
Negative pressure suction device in place in the apical portion of the wound following nonhealing with flap closure. This wound healed without further incident (Courtesy of Eric K. Johnson, MD)
In my opinion, the success rate of flaps represented in the literature is simply unbelievable (e.g., 100 % success rate of Limberg flaps in 102 patients presented by Urhan) [6]. In addition, the reported complication rates of V–Y-plasty are clearly unacceptable. If followed carefully and long enough, the 9.3 % infection rate and 7 % hematoma will inevitably grow with the number of recurrence/persistence of the disease [6].
My Approach (Dr. Abcarian)
If the purpose of the treatment of pilonidal sinus is an early return to duty (i.e., front line such as in the armed forces), I believe the Karydakis technique used on young military personnel offers the least complicated and most satisfactory procedure with low recurrence rate [5]. If not, I leave all pilonidal cystectomy wounds open, see the patient every 2 weeks, and shave the wound. Once healed, I recommend using depilatory cream to prevent hair growth in the vicinity of the healed wound once a month for an entire year. This plan has resulted in healing of an overwhelming majority of recurrent pilonidal cyst patients that have been referred to me throughout the years. I believe in the wisdom of Gabriel and his admonition of primary closure in infected, hairy, recurrent pilonidal with side branching to secondary openings off midline. I would only add obesity to his list.
Point: Counterpoint
Key Concept: There are many ways to approach the same disease process. You need to have a sound rationale behind what you do and never stop listening to (and learning from) other people’s opinions and experiences.
Dr. Abcarian and Dr. Orangio
1.
Dr. Abcarian it appears that you essentially only utilize “healing by secondary intention” of pilonidal cystectomy wounds?
Abcarian: That is correct.
2.
I (Dr. Orangio) feel that for a subpopulation of patients with pilonidal disease who have failed “healing by secondary intention” or have recurrent pilonidal disease, the utilization of fasciocutaneous flaps should be included in the surgeon’s armamentarium of options. The literature is quite supportive of this approach. Why do you disagree?
Abcarian: I have taken care of too many failed fasciocutaneous flaps in my 40 years of practice, and these are literally nightmares.
3.
Would you agree with me that recurrent pilonidal disease is secondary to inadequate primary excision?
Abcarian: In some cases yes, in others it is inadequate postoperative wound care by the patient and the surgeon.
4.




Why do you think that some patients have prolonged healing or even “nonhealing?” Do you feel this is because of poor compliance by the patient or not enough postoperative care by the primary surgeon?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








