Fig. 23.1
Thrombosed external hemorrhoid
Thrombosed external hemorrhoids will usually present acutely after a bout of straining, constipation, or diarrhea. The pain will be associated with a swelling that is painful to sit upon. The time course is usually 1 week or less for the pain if untreated and a few weeks for the clot to be absorbed. When symptomatic, office excision of the external hemorrhoid containing the clot—rather than making an incision through the external skin to enucleate the clot—gives both better short-term relief of pain and prevents recurrence at the site of that particular hemorrhoid. When there is hemorrhoidal crisis, with circumferential thrombosis of all or most of the external hemorrhoids, treatment should be performed in an operating room setting (Fig. 23.2).


Fig. 23.2
“Hemorrhoidal crisis,” with circumferential thrombosis of internal and external hemorrhoids
Anal Fissure (Fig. 23.3)

Fig. 23.3
Anal fissure and sentinel tag
Acute pain that occurs after every bowel movement, particularly a bout of hard constipated stools, and is sometimes associated with spotting of blood, is typical of an anal fissure. Fissures are normally diagnosed clinically by their classic appearance involving visible internal anal sphincter fibers, rolled edges, sentinel pile, and hypertrophied internal papillae (when chronic, see Fig. 23.3). Acutely they may be seen as a superficial tear in the anoderm. Anal fissure pain can become chronic if not treated and may also be a result of associated sphincter spasm. The chronicity is typically not from the fissure being refractory in these situations but rather long lasting due to lack of treatment. Patients at times try to self-medicate with over-the-counter remedies for many months without success. The gold standard treatment is lateral internal sphincterotomy. Most patients (and physicians) prefer to first try conservative measures (i.e., bulking agents, sitz baths, calcium channel blockers, glyceryl trinitrate, botulinum toxin) before sphincterotomy. Anal fissures, even after a competently performed lateral internal sphincterotomy, may occasionally persist as causes of pain if the fissure does not heal. Management options for persistent fissure include botulinum toxin injection, contralateral internal sphincterotomy, or cutaneous advancement flap down into the anal canal.
Anorectal Abscess/Fistula (Fig. 23.4)

Fig. 23.4
Perianal abscess
Abscesses, which are commonly treated with antibiotics alone in the primary care arena or emergency department in the mistaken hope that they will resolve, invariably need surgical drainage if they don’t drain spontaneously. For smaller, superficial perianal abscesses, drainage can generally easily be done in an office setting, using local anesthesia. It is our practice to remove an ellipse of skin overlying the abscess, to ensure a large enough opening to provide adequate drainage, and to delay premature cutaneous healing, which results in early recurrence of the abscess. The practices of “breaking up loculations,” or “packing the wound so it will heal,” are unnecessary and potentially detrimental by obstructing egress of purulence. It is sufficient to place a gauze pad over the wound. Larger abscesses, such as ischiorectal and/or horseshoe abscesses, are best treated in the operating room, using similar principles. Recurrence of abscess or persistence of drainage after operative treatment almost always indicates a fistula in ano. A fistula is itself rarely a cause of anal pain. However, persistent drainage can cause pruritus which itself may be irritating and be thought of as chronic pain.
Acute or Chronic Anal Pain
Key Concept: Several other disease processes may present with acute or chronic anal pain; however, most are still easily diagnosed with a thorough history and clinical examination. Radiographic and endoscopic ancillary tests are required in select scenarios.
Less common conditions, which are less obvious than the above, but may produce either acute or chronic discomfort, include:
Anal Crohn’s Disease (Fissures, Fistulae) (Fig. 23.5)

Fig. 23.5
Perianal Crohn’s disease (Courtesy of W. Brian Sweeney, MD)
While even simple fistulae can sometimes cause pain, generally from undrained components of abscesses related to their origins, this is more likely to be the case with anal Crohn’s disease and more complex fistulae. Furthermore, there may be pain from associated inflammation of the anus and rectum (proctitis). Evaluation is typically best performed with an examination under anesthesia, with emphasis on avoidance of fistulotomy, placement of setons through the known fistulae, and a careful search made for undrained areas, which can be opened and drained. Patients with anal Crohn’s disease often have chronic anal pain related to unrelenting inflammation and irritation. Sphincter spasm is common as well. These patients are not usually candidates for sphincterotomy and may heal poorly from anal procedures.
Hidradenitis Suppurativa (Fig. 23.6)

Fig. 23.6
Hidradenitis suppurativa
Hidradenitis suppurativa is a smoldering, uncomfortable cutaneous condition, arising from one or more of the sebaceous glands of the perineum. It is thought to represent a disorder of sebaceous gland metabolism, with similar lesions in the axillae and groins. When attempting to differentiate hidradenitis from other sources of perineal pathology, it is often helpful to perform a detailed examination of the skin adjacent to the anal verge. As this small circular area is devoid of hair and glands, disease in this location is not hidradenitis. Doxycycline, clindamycin, and Keflex are the most common antibiotics used, when given long term, for management of these lesions, while nonsteroidal anti-inflammatory drugs and immunosuppressants. For larger, more painful or nonresponsive lesions, conservative excision is often curative. At times, operative drainage of an acute cutaneous or deeper abscess is indicated [1].
Pruritus Ani (Fig. 23.7)

Fig. 23.7
Pruritus ani
While the anus is a particularly sensitive region, discrimination of sensations is not always clear. Patients can report itching, burning, and pain symptoms interchangeably. Though the predominant symptom in pruritus ani is itching, pain can be reported, and in severe cases, tiny linear and radial ulcerations are typically seen on a bed of lichenified, chronically irritated skin. Pain from this source must be distinguished from anal fissures, ulcers of an infectious nature, or other common sources of anal pain as described above. Pruritus ani generally responds to discontinuation of chemical and mechanical irritants such as use of soaps or shampoos, salves, hemorrhoid creams or flushable wipes, excessive scrubbing, excessive wiping with dry toilet paper, and scratching. The latter—avoidance of scratching—is often the most difficult for patients, though absolutely required to stop the cycle of perpetual itching and irritation. In addition, efforts should be made to avoid perianal moisture, which is thought to perpetuate the process. Use of creams and ointments generally is counterproductive for this reason. Recommendations of cotton or cornstarch to keep the area drier during the day are often helpful. Also, if stools are loose and/or frequent, attention to normalizing these characteristics can diminish irritation and requires much less perianal cleaning after bowel movements. This can be achieved with decreasing excess water intake and/or increasing dry fiber in the diet, such as by using fiber tablets or wafers (Table 23.1).
Table 23.1
Initial management of pruritus ani
Diminish local trauma | Avoid soap, scrubbing, and scratching |
Use damp toilet paper to gently pat the anal area clean. Do not use “baby wipes,” etc. | |
Diminish perianal moisture | 1. Use a small amount of cotton, and/or some corn starch powder, applied to the anal area, and kept there all day to absorb moisture |
2. Consider seepage of mucus or fecal matter as a possibly ongoing source of moisture. Possibilities include frequent stools, especially loose stools, diminished sphincter tone, or prolapsing hemorrhoidal or rectal mucosa. | |
3. Avoid creams, ointment, and other emollients which serve only to keep the area moist and are counterproductive |
There are a few rare patients who suffer from chronic irritation bordering on pain despite following the advised bowel and hygiene instructions. For pruritus symptoms which persist despite patients’ strict adherence to these guidelines, consider biopsy to rule out other conditions such as lichen sclerosus et atrophicus, Bowen’s or Paget’s disease, or similar entities, which may require dermatologic referral and/or a different therapeutic strategy.
Retrorectal Tumors
Because of the rarity of these lesions, and consequentially the failure to consider these in the differential diagnosis, delays in diagnosis occur more commonly than not. While these are often palpable on deep digital examination, a CT or MRI is necessary to further characterize them as benign or malignant and to plan therapy even if palpable. In general, biopsy is not routinely required, and virtually all of these require resection. A more detailed discussion is presented in Bailey et al., Colorectal Surgery (Fig. 23.8) [2].


Fig. 23.8
Retrorectal tumor
Bicycle Seat Issues
Serious cyclists may experience pain and/or numbness in the ischial tuberosities, perineum, or genitalia. It is worthwhile to inquire about this and other similar avocations that may require prolonged sitting in the evaluation of a patient with symptoms of this nature. The condition is usually related to pressure on perineal nerves. Numerous adjustments in seat design and position are available to prevent or treat such issues [3]. In addition, anti-chafing creams are routinely helpful to avoid any accompanying skin breakdown and irritation that can be a source of constant irritation.
Prostatitis
Pain in the anterior rectum in the region of the prostate may be from inflammatory, neurological, or bacterial origin and may be acute or chronic. This may be associated with urinary symptoms and/or sexual dysfunction. This may lead to pelvic floor pain as well. Pain with palpation of the prostate is often diagnostic in the setting of normal anal and rectal tissues. A combination of alpha-blockers and antibiotics is generally used by urologists to treat the condition, to whom referral is recommended [4]. Patients sometimes say it feels like a dull ache in the pelvis or as if they are sitting on a saddle. The bacteriology will differ depending on the age group, with sexually transmitted organisms such as chlamydia predominating in younger men, while multiple bacteria including gram-negative rods are more common in older men. In either case, often a prolonged course of antibiotics is required to completely clear the infection and avoid chronic prostatitis that is hallmarked by chronic pain but minimal objective evidence of prostatic inflammation.
Constipation
Sometimes patients associate anorectal pain with large and/or dry bowel movements (dyschezia). Anal fissures are commonly associated with this symptom and should be sought, but overdistension of the sphincter mechanism alone, without the presence of a fissure, may be an issue for some. Attention to improving bowel consistency with bulk laxatives and/or osmotic laxatives may give effective long-term relief. Regardless of whether or not a fissure is seen, hypertonicity of the sphincter can often be felt on exam, and treatment is the same, regardless.
Gynecological Sources
Gynecologic causes of pelvic pain, such as endometriosis, enterocele, rectocele, ovarian diseases, ectopic pregnancies, or fallopian tube abnormalities, typically do not cause anal pain. Rather, they result in deep-seated abdominal or pelvic pain, constipation, or defecation outlet dysfunction. Though they may be broadly included in the discussion of the differential diagnosis of anal pain, the reader is referred to one of several available gynecological textbooks where they are best addressed.
Proctitis/Pouchitis
Proctitis is inflammation of the rectum secondary to infections, postradiation, diversion, chemical irritation (corrosive or disinfectants), or inflammatory bowel diseases. Proctitis is usually associated with rectal bleeding, and diagnosis is generally readily made using office sigmoidoscopy (Fig. 23.9). By contrast, pouchitis occurs in 30–50 % of patients undergoing a restorative ileal pouch-anal anastomosis following total proctocolectomy for chronic ulcerative colitis (Fig. 23.10) [5]. Typically bacterial overgrowth in the pouch results in an inflammatory response. Inflammation can also occur in the remnant mucosa of the anus (i.e., “cuffitis”). Pouchitis and proctitis may be associated tenesmus, or with painful sensations in the pelvis, and is classically associated with a sharp rise in the number of bowel movements each day. It is our experience that some patients develop pouchitis from overcompensating with antidiarrheals, in an effort to diminish the frequency of bowel movements below about 3/ day.
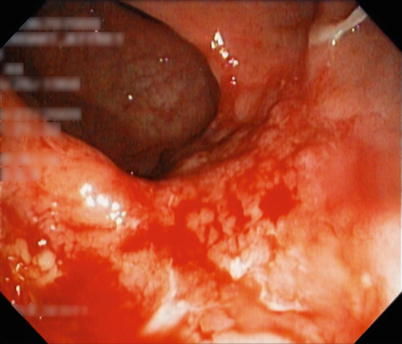

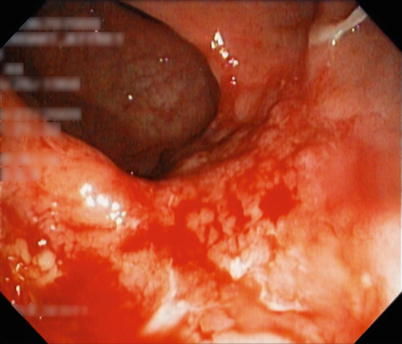
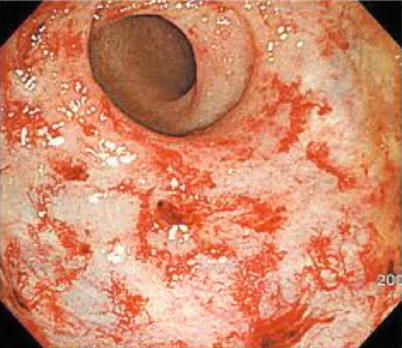
Fig. 23.9
Proctitis

Fig. 23.10
Pouchitis (With permission from Science SourceÆ, registered trademark of Photo Researchers, Inc. Images and Text. Copyright © 2013 Photo Researchers, Inc. All Rights Reserved)
Treatment of pouchitis is generally with antibiotics (metronidazole or ciprofloxacin are the most commonly used). Probiotics are sometimes used in an effort to prevent pouchitis, but there are very limited data on the efficacy of this practice. Other more recalcitrant bouts of pouchitis require steroids, chronic cyclical courses of antibiotics, or even immunosuppressants or diversion. Proctitis is best managed by addressing the cause and may include anti-inflammatory agents or antibiotics as indicated given the underlying etiology. Proctitis resulting from radiation therapy is addressed in the section below.
Radiation
Radiation effects in the perianal area are occasionally painful and must be distinguished from pruritus ani, from dermatoses such as lichen sclerosus et atrophicus, and from Bowen’s or Paget’s diseases. Since the radiation to this area is usually given for anal or distal rectal, vulvar, and prostatic malignancies, the differential diagnosis should include a careful search for recurrence of these cancers. The radiation effects that cause pain include anoderm thinning, proctitis, sphincter injury, and stenosis. It is our practice to first attempt sucralfate suppositories (these can be made by compounding pharmacies). If bleeding persists, then dilute 10 % formalin placed topically. For more resistant sources of bleeding, laser therapy or argon beam coagulation are occasionally needed to destroy the damaged tissue (Fig. 23.11) [6].