Chapter 31 Cholecystitis
Acute Cholecystitis
Pathogenesis
The cause of acute cholecystitis is an impacted gallstone in the outlet of the gallbladder, either in the infundibulum or in the cystic duct (Sjodahl et al, 1978). The impacted gallstone results in gallbladder distension and edema with acute inflammation, which eventually can result in venous stasis and obstruction, followed by thrombosis of the cystic artery. Ultimately, ischemia and necrosis of the gallbladder occur. Because the fundus of the gallbladder is the greatest distance from the cystic arterial blood supply, it is more sensitive to ischemia and is the most common location for necrosis of the gallbladder. The acute inflammation of cholecystitis may be complicated by secondary biliary infection. Positive biliary cultures are found in about 20% of patients with acute cholecystitis (den Hoed et al, 1998), the most common of which are gram-negative bacteria of gastrointestinal origin, such as Klebsiella spp. and Escherichia coli.
Diagnostic Evaluation and Imaging
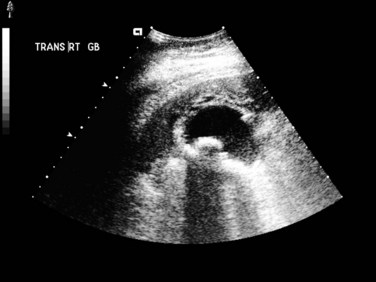
Abdominal US (see Chapter 13) is useful for assessing patients suspected to have acute cholecystitis. Typical findings include gallstones, gallbladder wall thickening (>4 mm), and pericholecystic fluid (Fig. 31.1). In addition, the sonographer can assess for pain and inspiratory arrest when the gallbladder is directly compressed by the US probe (sonographic Murphy sign). Typically, conventional gray scale imaging is used, which is highly sensitive and specific for diagnosing acute cholecystitis, with an overall accuracy of greater than 90% (Soyer et al, 1998). Other techniques of imaging that assess blood flow, such as color velocity imaging, may improve accuracy in selected cases (Soyer et al, 1998; Uggowitzer et al, 1997).
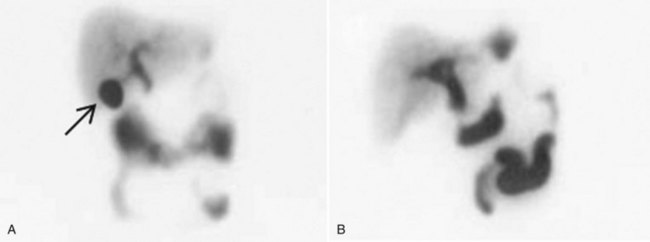
Hepatobiliary scintigraphy (see Chapter 15) is a useful study in selected patients when the diagnosis is uncertain. This nuclear medicine study is performed with derivatives of aminodiacetic acid (hepatoiminodiacetic acid [HIDA], isopropylacetanilido imidodiacetic acid [PIPIDA], or di-isopropylacetanilido iminodiacetic acid [DISIDA]), which are taken up by hepatocytes and secreted in the bile. When the tracer is labeled with technetium, it is possible to visualize biliary function with scintigraphy. A normal scan delineates the biliary tree, including the gallbladder, and shows prompt emptying of the agent into the duodenum. Nonvisualization of the gallbladder on hepatobiliary scan is consistent with acute cholecystitis (Fig. 31.2).
An added utility of this test is that in addition to gallbadder filling or nonfilling, it also evaluates gallbladder emptying. Abnormal emptying is defined as an ejection fraction (EF) of 35% or less on scintigraphy, a finding suggestive of biliary pathology. Middleton and Williams (2001) reported on 141 patients with normal US and scintigraphy with normal gallbladder filling and an EF of 35% or less who underwent cholecystectomy. Of these patients, 95% had significant improvement or complete resolution of symptoms after surgery, and 41% of these patients had cholecystitis on histologic evaluation of the gallbladder.
Hepatobiliary scintigraphy is not useful in patients with poor hepatic function because it requires hepatic excretion of bile, but it is accurate in about 90% of patients and may be more accurate than US alone. Hepatobiliary scintigraphy is more involved, more expensive, and requires a longer time than US; however, it should be reserved for selected cases (Chatziioannou et al, 2000; Kalimi et al, 2001). Mahid and colleagues (2009) have suggested a diagnostic approach that starts with US for patients with biliary symptoms. If no gallstones are definitively identified, this should be followed by esophagogastroduodenoscopy to exclude alternative causes of symptoms, such as peptic ulcer disease or gastritis. If this test result is negative, hepatobiliary scintigraphy should follow.
Computed tomography (CT; see Chapter 16) can also help diagnose acute cholecystitis and provides more detailed anatomic information than US. CT is particularly useful in patients whose symptoms suggest a complication such as pericholecystic abscess or an alternative diagnosis. The CT findings of acute cholecystitis are the same as those seen on US and include wall thickening, pericholecystic stranding, distension of the gallbladder, high-attenuation bile, pericholecystic fluid, and subserosal edema. CT generally is less sensitive than US for diagnosing acute cholecystitis, particularly early in the course, when the imaging findings may be subtle (Fidler et al, 1996; Harvey & Miller, 1999).
Treatment
The definitive treatment for acute cholecystitis is cholecystectomy. From the time this operation was first performed in 1882 by Langenbuch, open cholecystectomy has been the standard of care for patients with acute cholecystitis. With the advent of laparoscopic cholecystectomy in the 1980s, the standard approach has changed such that cholecystectomy is now routinely performed laparoscopically. The benefits of laparoscopic cholecystectomy are discussed in depth elsewhere (see Chapters 33 and 34), but they include a shorter postoperative stay and decreased analgesia requirements (Cox et al, 1993). Although the laparoscopic approach is now standard for most cases, it is interesting to note that two prospective, randomized studies suggested little or no difference in several outcome measures between laparoscopic versus small-incision open cholecystectomy (Majeed et al, 1996; Keus et al, 2008).
Early analysis of the results of laparoscopic cholecystectomy in patients with acute versus chronic cholecystitis showed increased morbidity and mortality rates for patients with simple or complicated acute cholecystitis. Because of the increased morbidity and mortality, acute cholecystitis initially was considered a relative contraindication to laparoscopic cholecystectomy (Flowers et al, 1991). Subsequent reports have shown the improved safety of this technique in the acute setting (Chandler et al, 2000; Johansson et al, 2003; Lai et al, 1998; Lo et al, 1998). The conversion rate to an open procedure is higher for patients with acute cholecystitis compared with patients undergoing elective operations for simple biliary colic (Schirmer et al, 1991), but most patients with acute cholecystitis (>80%) can undergo laparoscopic cholecystectomy successfully (Papi et al, 2004). Retrospective series revealed that risk factors for conversion to open cholecystectomy include obesity (Rosen et al, 2002), elevated white blood cell count (Alponat et al, 1997; Kanaan et al, 2002), and male gender (Kanaan et al, 2002).
Other novel surgical techniques have been proposed to treat patients with acute cholecystitis, including so-called minilaparoscopic cholecystectomy (see Chapter 33), which uses 2- to 3-mm ports (Hsieh, 2003), and minicholecystectomy (Assalia et al, 1997), in which a small (mean, 5.5 cm) incision is used to remove the gallbladder. A prospective, randomized trial demonstrated that minilaparoscopic cholecystectomy resulted in decreased postoperative pain and superior cosmesis when compared with conventional laparoscopic cholecystectomy, with no significant difference in operative time, blood loss, or complications (Novitsky et al, 2005).
Laparoscopic subtotal cholecystectomy (LSC) has also been evaluated as a means of decreasing the conversion rate to open procedure in patients with acute cholecystitis (Horiuchi et al, 2008; Singhal et al, 2009). This procedure involves leaving the posterior wall of the gallbladder when it is significantly difficult to dissect from the liver bed, with cauterization of the remnant mucosa and suturing or stapling of the gallbladder neck in cases of severe inflammation of the triangle of Calot. Indeed, in the face of severe inflammatory change, such an approach is safter than risking injury to the common hepatic duct by pursuing dissection within the porta hepatis. Horiuchi and colleagues (2008) demonstrated a significant decrease in conversion rate to open procedure with the use of these techniques with no increase in postoperative complications. All patients undergoing LSC had temporary subhepatic drains placed in this study. This technique, although innovative, does not have wide clinical applicability because of limited availability of instruments, specialist surgeons trained in their use, or both. Laparoscopic cholecystectomy remains the standard therapy for definitive treatment of patients with acute cholecystitis, with conversion to an open procedure if necessary.
In patients with a high perioperative risk from sepsis or other underlying medical comorbidities, initial treatment of acute cholecystitis with percutaneous cholecystostomy tube placement is preferred (see Chapters 28 and 32). These tubes can be placed using either US or CT guidance (Hatzidakis et al, 2002). This procedure effectively decompresses the gallbladder, evacuating the infected bile and relieving the pain associated with gallbladder distension, and it is associated with a low complication rate (Akyürek et al, 2005; Byrne et al, 2003; Spira et al, 2002; Werbel et al, 1989). In addition, most patients (>80%) improve clinically within a short time (Byrne et al, 2003; Hatzidakis et al, 2002; Vauthey et al, 1993). After stabilization of the patient, and if the clinical situation otherwise warrants, delayed cholecystectomy should be performed, which often can be done laparoscopically (Spira et al, 2002). Akyürek and colleagues (2005) demonstrated decreased hospital stay and cost in high-risk patients undergoing percutaneous cholecystostomy followed by early laparoscopic cholecystectomy compared with those treated conservatively with intravenous (IV) antibiotics and bowel rest followed by delayed cholecystectomy. In high-risk patients in whom general anesthesia is contraindicated, percutaneous stone extraction has been used successfully (Gibney et al, 1987; Wong et al, 1999). More recently, single and repeated percutaneous transhepatic gallbladder aspiration has been shown to be successful in high-risk patients with acute cholecystitis who do not respond to conservative therapies (Tsutsui et al, 2007). This treatment modality is not widely practiced, however.
Timing of Surgery
The optimal interval of time between the diagnosis of acute cholecystitis and definitive treatment with cholecystectomy has been the subject of many prospective randomized trials, nine evaluating open cholecystectomy and five evaluating laparoscopic cholecystectomy (Papi et al, 2004; Siddiqui et al, 2008). The concern in operating on patients with early cholecystitis (typically defined as <3 days) is the potential for increased postoperative complications, including common bile duct injury. The risk of performing cholecystectomy late (weeks after the diagnosis of cholecystitis) is that a subset of patients have recurrent symptoms during the period between diagnosis and surgical treatment, which leads to recurrent hospital admissions and urgent surgery (Papi et al, 2004). In multiple randomized prospective trials evaluating the timing of open cholecystectomy, patients undergoing early operation experienced no increased perioperative morbidity or mortality and had a shorter length of hospital stay compared with patients undergoing delayed operation (Norrby et al, 1983; Van der Linden & Edlund, 1981). In addition, a meta-analysis of these trials demonstrated that more than 20% of patients failed medical management while awaiting definitive treatment, and approximately half of these patients required urgent surgical treatment as a result (Papi et al, 2004). In this same analysis, no increase in morbidity was seen in patients undergoing early definitive treatment with laparoscopic (P = .6) or open (P = .2) cholecystectomy compared with delayed treatment, but a clear difference was seen in length of hospital stay, with patients undergoing delayed treatment requiring a more prolonged hospitalization (Papi et al, 2004). Although it is safe to perform cholecystectomy either early or late after an episode of acute cholecystitis, patients benefit when surgery is performed early.
Performing laparoscopic cholecystectomy in patients with acute cholecystitis poses unique challenges to surgeons because of the potential for increased morbidity, including the most feared complication, common bile duct injury. The concern is that the acute inflammation may obscure the anatomy, leading to an increase in postoperative complications. Five prospective randomized trials have evaluated the outcome of patients with acute cholecystitis undergoing early versus late laparoscopic cholecystectomy (Table 31.1). Although a significant increase in operation time was experienced for those undergoing early compared with delayed cholecystecomy (P = .002), the results of these trials uniformly showed no significant difference in postoperative morbidity or mortality, including common bile duct injury, when surgery is performed early (Siddiqui et al, 2008
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree