Fig. 14.1
SITRACC® (Edlo) multichannel platform
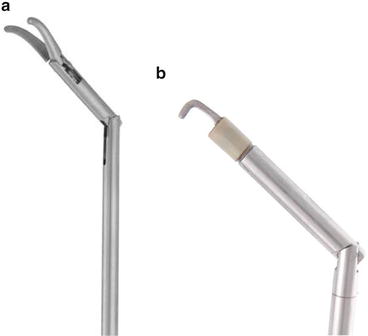
Fig. 14.2
(a, b) Articulated distal extremity; prehension forceps and hook for coagulation
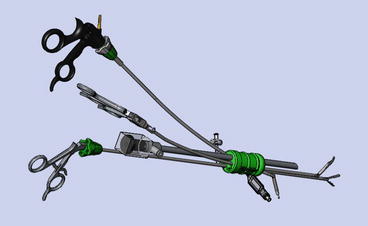
Fig. 14.3
Disposition of internal and external SITRACC® platform (Edlo) and its curved/articulated instruments
14.2 LESS Cholecystectomy: Technique
The SITRACC® platform (Edlo) consists of a multichannel trocar, with three 5-mm openings and one 10-mm opening, which can be changed to a 5-mm opening with the use of a reducer that is provided. Curved, articulated end, and flexible instruments have been specially created for this platform and approach. The use of 5-mm optics, with a minimum angle of 30°, is highly recommended.
The team positions are similar to those for conventional videolaparoscopic cholecystectomy, except the surgeon must stand more caudal to the patient, on the patient’s left side. The camera person also stands on the left side (Fig. 14.4).
Fig. 14.4
Positioning of the surgical team
The multichannel trocar is introduced by the open technique through the umbilicus. It must be noted that better aesthetic results can be obtained with a completely perpendicular intra-umbilical incision. With such an incision, the surgical scar is fully hidden within the natural scar.
After introduction of the platform, the distal fixator balloon, which has a dual function (fixation in the abdominal wall and prevention of pneumoperitoneum leakage), must be inflated with approximately 15 mL of air; tension is registered and controlled externally (Fig. 14.5a, b). The entry portals of the platform must remain in the form of a cross, with the largest placed in the lower quadrant.
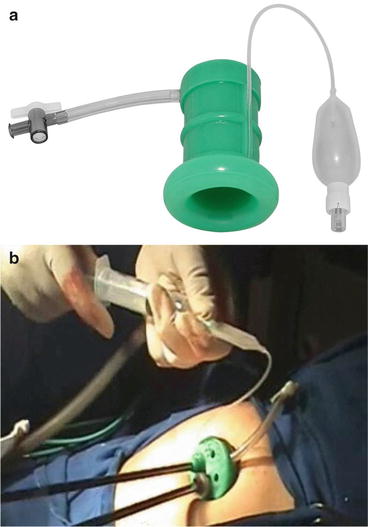
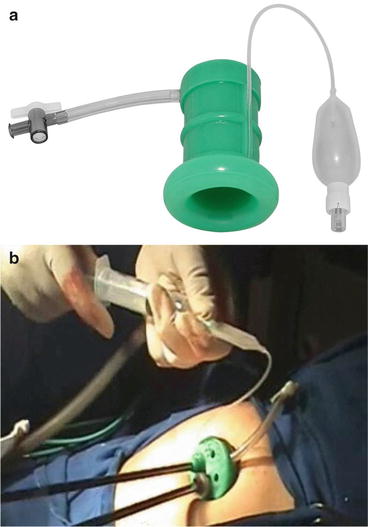
Fig. 14.5
(a) Platform with balloon (b) External insufflation of the balloon
The first instrument introduced is the fully flexible grasper, which must grasp the bottom of the vesicle, pulling it toward the diaphragm and, at the same time, retract the liver to facilitate exposure of Calot’s Triangle (Fig. 14.6).
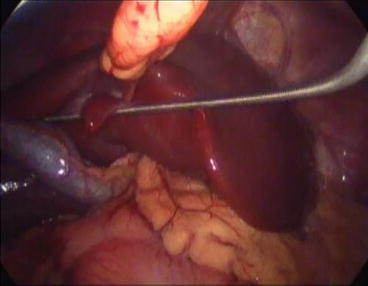
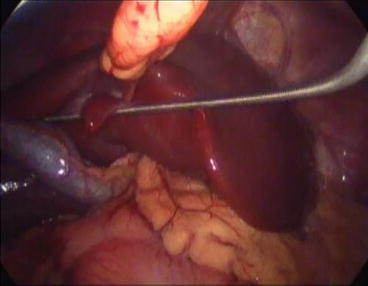
Fig. 14.6
Totally flexible grasper. Note the dual function – to pull the gallbladder and retract the liver
The curved prehension forceps (which remain in the surgeon’s left hand) are introduced through the left entry portal. These forceps must grasp the gallbladder infundibulum and, with lateral and anterior traction, adequately expose Calot’s Triangle so that the cystic duct and artery are properly visualized.
The instruments for dissection/sectioning are then introduced under direct visualization, through the right entrance. These instruments, which may vary according to the circumstance and the surgical strategy, include the articulated hook, articulating dissector forceps, and curved scissors. It should be noted that, at certain times during the surgery, conventional rigid laparoscopic instruments may be needed. These can be used in a hybrid way, especially in cases of advanced inflammation and/or adhesion, because they provide greater strength for dissection.
The elements of the pedicle are then dissected and isolated, with movement facilitated by the distal articulation of the dissector instrument (Fig. 14.7). The cystic duct and pedicle vessels are then doubly clipped with 5-mm clips. If the cystic duct is particularly wide, a 10-mm clip applicator (LT400) can be used through the south entry portal. In this case, the reducer is removed, and the 5-mm optic is placed laterally. The curvature of the scissors helps greatly here (Fig. 14.8).
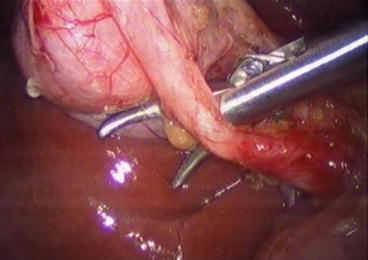
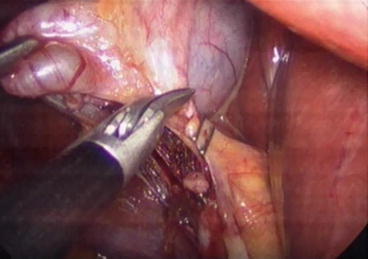
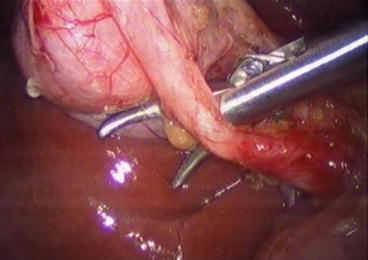
Fig. 14.7
Isolation of the cystic duct by forceps for articulated dissection
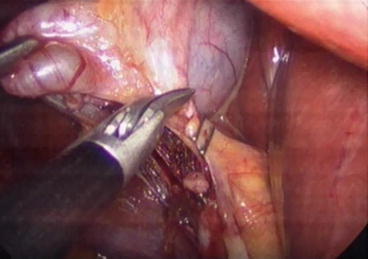
Fig. 14.8
Section of the clipped cystic duct
The gallbladder is then dissected from the liver bed by means of a coagulation hook with distal articulation (Fig. 14.9). This device allows adequate and ample movement for this step. After dissection of the gallbladder, hemostasis is established, and the organ is removed through the interior of the platform after the distal balloon is deflated (Fig. 14.10).
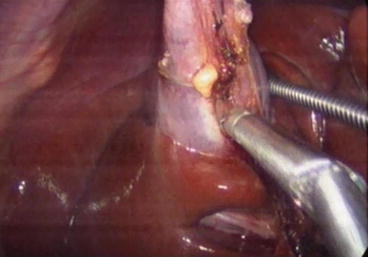

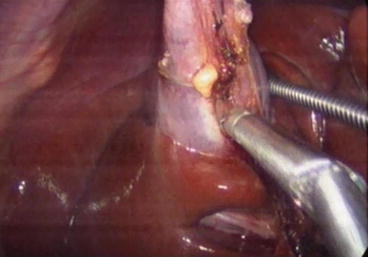
Fig. 14.9
Dissection of the gallbladder by the articulating hook

Fig. 14.10
Removal of the gallbladder inside the platform; the balloon is deflated posteriorly
In difficult cases, it is possible to make use of a trocar of 5-mm or even 2-mm and positioned in the right hypochondrium to facilitate exposure of Calot’s Triangle through traction at the bottom of the vesicle. When necessary, a Penrose drain can be inserted through the platform and removed via the same trocar.
14.3 LESS Cholecystectomy: Results
A multicenter study [23] performed in 2008 and reported the next year, involved nine Brazilian surgery services in several cities and culminated in the performance of 81 LESS cholecystectomies. Ten surgeries required placement of an extra trocar in the right hypochondrium, due to technical difficulties. Three of the LESS procedures were converted to conventional videolaparoscopy.
Our personal experience with the LESS approach, using the SITRACC® platform, includes 172 cholecystectomies performed at the Red Cross Hospital/Positivo University, Curitiba, Brazil between October 2008 and June 2013, under approval of the institution’s Ethics in Research Committee. All patients had symptomatic gallstones. Eight procedures required an additional portal of 5 mm in the right hypochondrium and, in four cases, full conversion to what we call conventional videolaparoscopy was required (all because of “difficult infundibulum”). There were no conversions to open surgery. The average operative time was 43 minutes, and all patients were released 24 hours after the surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









