CHAPTER 15
Antimicrobials for parasitic diseases
5-Nitroimidazoles
Introduction
5-Nitroimidazoles were introduced to medicine in 1960 when metronidazole was used to treat Trichomonas vaginalis. These compounds were soon found to possess a wide spectrum against intestinal protozoa and anaerobic bacteria and Helicobacter pylori.
Mechanism of action
The mechanism of action of these compounds is still not well understood. Presumably the 5-nitro group of drug leads to the breakage of the helical structure of the DNA of the microorganism.
Pharmacology
5-nitroimidazoles can be administered orally, intravenously, rectally or intravaginally. The bioavailability is complete after oral ingestion. The various derivatives vary in the amount of urinary or biliary elimination of the compound and its metabolites.
Clinical effectiveness
Spectrum of 5’nitroimidazoles
5-nitroimidazoles are effective against infections by Helicobacter pylori. and anaerobic bacteria (e.g., Clostridium difficile), as well as a large variety of intestinal protozoa among these Entamoeba histolytica, Giardia intestinalis, Trichomonas spp. (Table 15.1). Whereas clinically decreased susceptibility of Entamoeba histolytica sensu stricto is not a frequent problem provided metronidazole is given at a full dose this is not the case in giardiasis. Due to the lack of commercial interest, controlled studies on the efficacy of 5-nitroimidazole are scarce, but clinicians worldwide report that the susceptibility of Giardia is decreasing. Therefore, first and even second therapy attempts with a single drug frequently fail. Unfortunately no systematic study has been undertaken so far to establish a sound algorithm for the therapy of multiresistant giardiasis (Escobedo et al., 2007). Patients who do not clear giardiasis after several treatment attempts should be investigated for immune-suppression e.g., IgA deficiency and HIV infection. Patients with CVID (common variable immune deficiency) are particularly difficult to treat. A tentative algorthithm proposes the use of one 5-nitroimidazole (tinidazole, secnidazole, ornidazole) as first line therapy, and to switch to another 5-nitro-imidazole while adding another substance class (e.g., paromomycine) at the second attempt. If both fail, chloroquine or nitazoxanide may be added and therapy courses extended (Table 15.1)
Table 15.1 Treatment of Entamoeba histolytica and Giardia intestinalis
| Organism | Drug of choice and dose | Alternative |
| Entamoeba histolytica (sensu stricto) | ||
| Intestinal carriage | Paromomycin 25–35 mg/kg/d in 3 divided doses for 5–10 days | 1. Diloxanid furoate 500 mg tid for 10 days or 2. Iodoquinol 650 mg tid for 20 days |
| Invasive E. histolytica s.s. Colitis, amoeboma, extraintestinal amebiasis, liver abscess | Metronidazole 750 mg, tid PO or in severe cases i.v + Paromomycin 25–35 mg/kg/d for 10 days in 3 divided doses for 10 days Only liver abscesses close to the pericardium: drainage + optionally: Chloroquine (salt) 250 mg bid for 7–20 days | Tinidazole 800 mg tid for 3–5 days + Diloxanid furoate 500 mg tid for 10 days or + Iodoquinol 650 mg tid for 20 days Paromomycine |
| Giardia intestinalis | Tinidazole 1 g bid for 2–5 days Ornidazole 500 mg qid for 5 days Secnidazole 1000 mg/d for 3 days Metronidazole 750 mg tid for 3–5 days | resistant (combined two-drug therapy): add Paromomycin 25–35 mg/kg/d for 10 days in 3 divided doses for 10 days or Mebendazole 200 mg tid for 3–5 days or Albendazole 10–15 mg/kg/d for 3 days |
| Multiresistant (combined triple therapy): add: chloroquine (salt) 250 mg bid for 7–20 days or nitazoxanide 500 mg/d bid for 3–10 days |
Toxicity
Side effects of 5-nitroimidazoles if given for less than ten days are usually mild and reversible, and most frequently include nausea, vomiting, metallic taste and intolerance to alcohol. CNS side effects (e.g., dizziness and sleepiness) occur more frequently in metronidazole therapy as compared to the other 5-nitroimidazole derivatives. In long-term high dose therapy leucopenia, agranulocytosis, hallucinations, peripheric polyneuropathy and convulsions have been reported.
All nitroimidazoles are pregnancy category C, not because of embryotoxic and teratogenic effects but of mutagenic and cancerogenic effects with high dose long-term-administration in animals. If possible, 5-nitroimidazoles should not be given during the first trimester. Excretion into breast milk is rapid, and nursing should be suspended during 5-nitroimidazole therapy
Imidazole derivatives with generic and brand names
| Metronidazole: | Flagyl, Clont |
| Tinidazole: | Fasigyne, Simplotan, Tricolam |
| Secnidazole: | Flagentyl |
| Ornidazole: | Tiberal |
| Nimorazole: | Esclama |
Benzimidazoles
Introduction
Benzimidazoles were first developed for veterinary medicine where several compounds are used including albendazole, flubendazole, fenbendazole and triclabendazole. Mebendazole was introduced first into human medicine followed by thiabendazole which, however, was not well tolerated and was replaced in the 1980s by albendazole. Triclabendazole was also widely used in Veterinary Medicine before its introduction in man in the 1990s (Millán et al., 2000; Keiser et al., 2005)
Mechanism of action
All benzimidazoles have a similar mechanism of action on nematodes. These drugs bind to helminth tubules with subsequent inhibition of polymerization to microtubules. Benzimidazoles are usually absorbed several fold if taken with a fatty meal. Albendazole has a more rapid tissue diffusion than mebendazole. Triclabendazole and its active sulfoxide metabolite are primarily excreted in the bile.
Pharmacology
All benzimidazoles are taken orally. Whereas metabolites of mebendazole are inactive, sulfoxide metabolites of albendazole and triclabendazole are highly active.
Clinical effectiveness
Mebendazole is less well absorbed from the intestine than albendazole and undergoes an important first pass effect in the liver with transformation to inactive metabolites. It is inexpensive and particularly useful in intestinal nematode infections, e.g., pinworm, whipworm and hookworm infections (Table 15.2). It has been replaced by albendazole in the treatment of echinococcosis but constitutes an alternative in patients with albendazole hepatitis (Brunetti et al., 2010; Eckert et al., 2011).
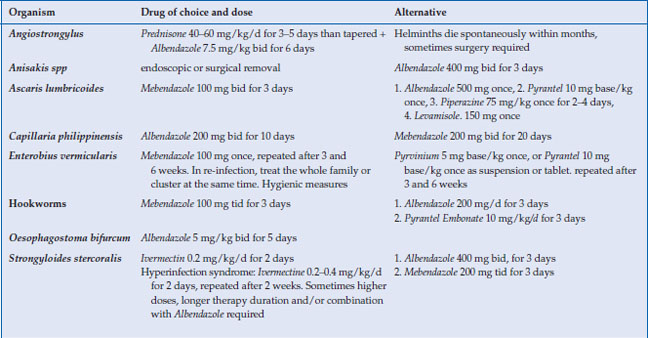
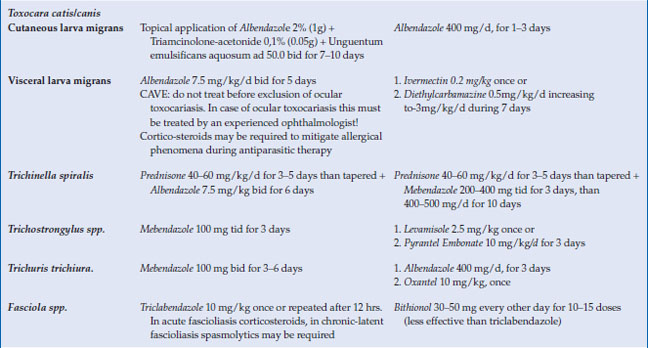
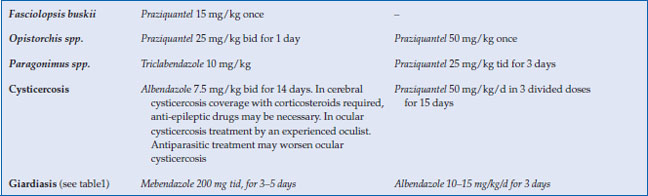
Table 15.2 Indications for benzimidazole compounds and ivermectin. Alternative therapies
Albendazole has a rapid tissue diffusion and a broad spectrum not only against some larval and adult nematodes (hookworms, Ascaris lumbricoides, Loa loa filariae) but also against the metacestode stage of human cestodes (Table 15.2). It is the drug of choice for cysticercosis and echinococcosis. Benzimidazoles have some antiprotozoal activity against G. intestinalis and the microsporidia Encephalitozoon spp. Due to its higher excretion in bile, mebendazole seems to be more effective than albendazole in this respect (Escobedo et al. 2007).
Triclabendazole is the drug of choice for trematode infections due to the large liver flukes Fasciolia hepatica, F. gigantica and the lung flukes Paragonimus spp. In the future, it might play a role in echinococcosis therapy (Richter et al., 2013) (Table 15.2). Triclabendazole is available through the World Health Organization or from the manufacturer (Keiser and Utzinger 2004; Keiser et al., 2005).
Toxicity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






