Anatomy of the Genitourinary Tract: Introduction
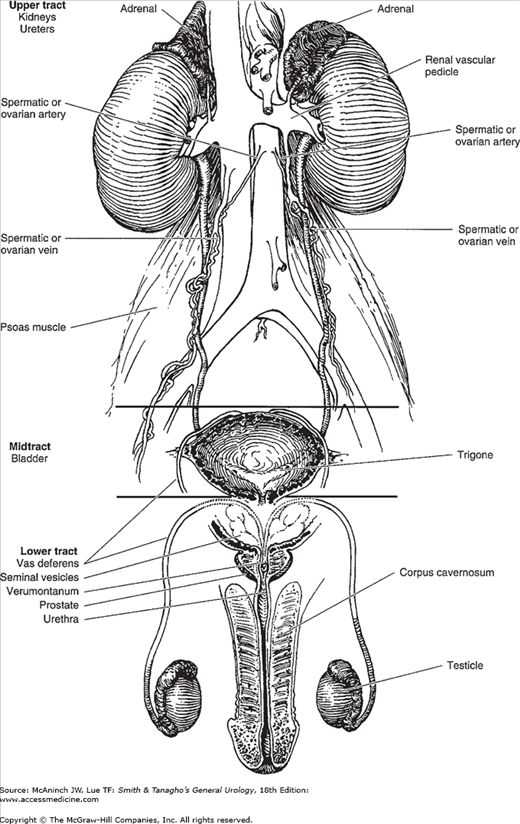
Urology deals with diseases and disorders of the male genitourinary tract, the female urinary tract, and the adrenal gland. These systems are illustrated in Figures 1–1 and 1–2.
Adrenals
Each kidney is capped by an adrenal gland, and both organs are enclosed within Gerota’s (perirenal) fascia. Each adrenal weighs about 5 g. The right adrenal is triangular in shape; the left is more rounded and crescentic. Each gland is composed of a cortex, chiefly influenced by the pituitary gland, and a medulla derived from chromaffin tissue (Avisse et al, 2000; O’Donoghue et al, 2010).
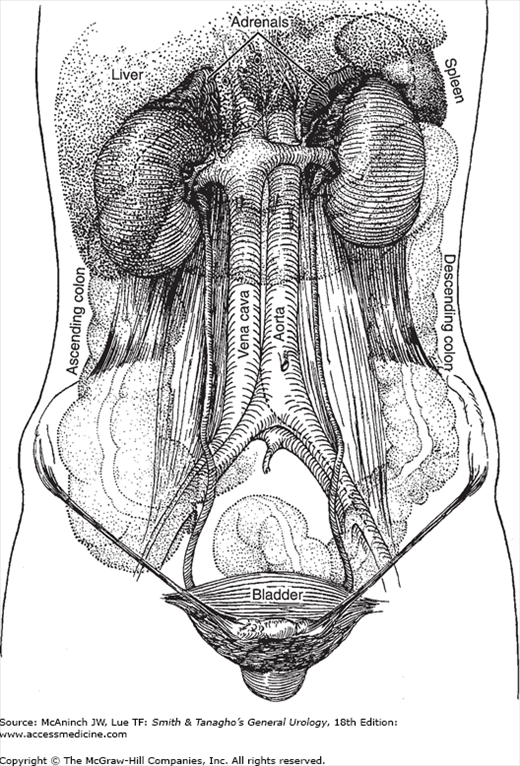
Figure 1–2 shows the relation of the adrenals to other organs. The right adrenal lies between the liver and the vena cava. The left adrenal lies close to the aorta and is covered on its lower surface by the pancreas. The spleen lies superior and lateral to it.
The adrenal cortex, which makes up 90% of the mass, is composed of three distinct layers: the outer zona glomerulosa, the middle zona fasciculata, and the inner zona reticularis. The medulla lies centrally and is made up of polyhedral cells containing eosinophilic granular cytoplasm. These chromaffin cells are accompanied by ganglion and small round cells.
Each adrenal receives three arteries: one from the inferior phrenic artery, one from the aorta, and one from the renal artery.
Blood from the right adrenal is drained by a very short vein into the vena cava; the left adrenal vein terminates in the left renal vein.
Kidneys
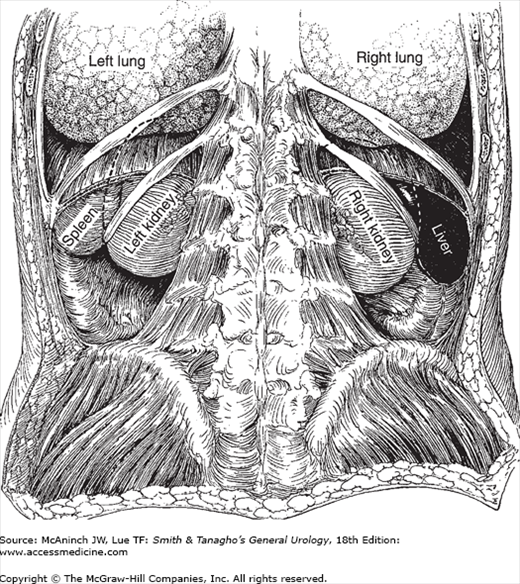
The kidneys lie along the borders of the psoas muscles and are therefore obliquely placed. The position of the liver causes the right kidney to be lower than the left (Figures 1–2 and 1–3). The adult kidney weighs about 150 g each.
The kidneys are supported by the perirenal fat (which is enclosed in the perirenal fascia), the renal vascular pedicle, abdominal muscle tone, and the general bulk of the abdominal viscera (Rusinek et al, 2004). Variations in these factors permit variations in the degree of renal mobility. The average descent on inspiration or on assuming the upright position is 4–5 cm. Lack of mobility suggests abnormal fixation (eg, perinephritis), but extreme mobility is not necessarily pathologic.
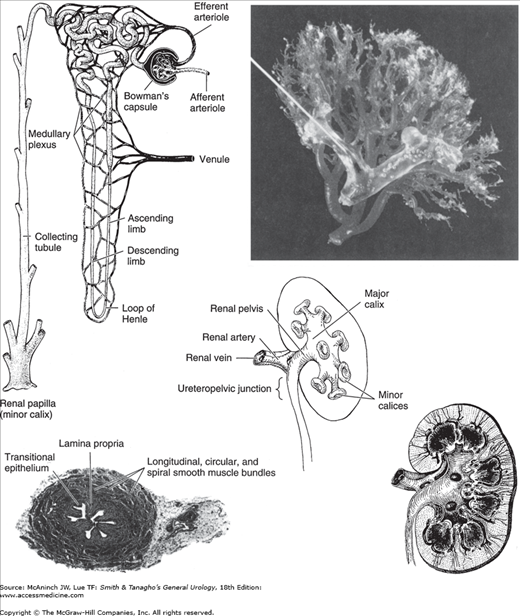
On longitudinal section (Figure 1–4), the kidney is seen to be made up of an outer cortex, a central medulla, and the internal calices and pelvis. The cortex is homogeneous in appearance. Portions of it project toward the pelvis between the papillae and fornices and are called the columns of Bertin. The medulla consists of numerous pyramids formed by the converging collecting renal tubules, which drain into the minor calices at the tip of the papillae.
Figure 1–4.
Anatomy and histology of the kidney and ureter. Upper left: Diagram of the nephron and its blood supply. (Courtesy of Merck, Sharp, Dohme: Seminar. 1947;9[3].) Upper right: Cast of the pelvic caliceal system and the arterial supply of the kidney. Middle: Renal calices, pelvis, and ureter (posterior aspect). Lower left: Histology of the ureter. The smooth-muscle bundles are arranged in both a spiral and a longitudinal manner. Lower right: Longitudinal section of kidney showing calices, pelvis, ureter, and renal blood supply (posterior aspect).
Figures 1–2 and 1–3 show the relations of the kidneys to adjacent organs and structures. Their intimacy with intraperitoneal organs and the autonomic innervation they share with these organs explain, in part, some of the gastrointestinal symptoms that accompany genitourinary disease (Glassberg, 2002).
The functioning unit of the kidney is the nephron, which is composed of a tubule that has both secretory and excretory functions (Figure 1–4). The secretory portion is contained largely within the cortex and consists of a renal corpuscle and the secretory part of the renal tubule. The excretory portion of this duct lies in the medulla. The renal corpuscle is composed of the vascular glomerulus, which projects into Bowman’s capsule, which, in turn, is continuous with the epithelium of the proximal convoluted tubule. The secretory portion of the renal tubule is made up of the proximal convoluted tubule, the loop of Henle, and the distal convoluted tubule.
The excretory portion of the nephron is the collecting tubule, which is continuous with the distal end of the ascending limb of the convoluted tubule. It empties its contents through the tip (papilla) of a pyramid into a minor calyx.
The renal stroma is composed of loose connective tissue and contains blood vessels, capillaries, nerves, and lymphatics.
Usually there is one renal artery, a branch of the aorta that enters the hilum of the kidney between the pelvis, which normally lies posteriorly, and the renal vein. It may branch before it reaches the kidney, and two or more separate arteries may be noted (Budhiraja et al, 2010). In duplication of the pelvis and ureter, it is common for each renal segment to have its own arterial supply.
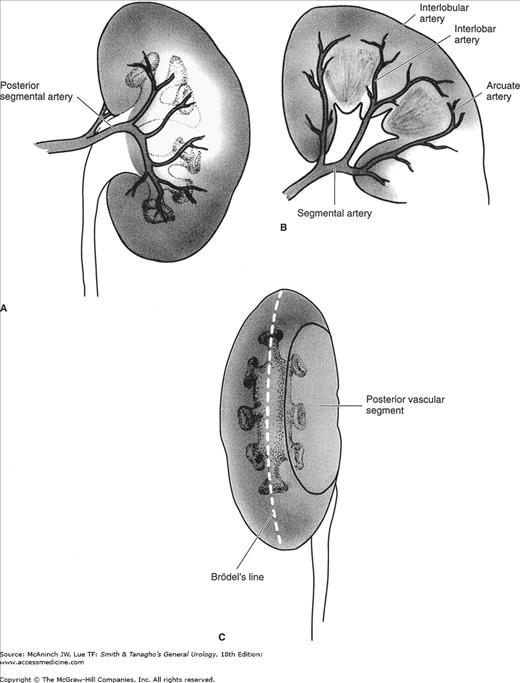
Figure 1–5.
A: The posterior branch of the renal artery and its distribution to the central segment of the posterior surface of the kidney. B: Branches of the anterior division of the renal artery supplying the entire anterior surface of the kidney as well as the upper and lower poles at both surfaces. The segmental branches lead to interlobar, arcuate, and interlobular arteries. C: The lateral convex margin of the kidney. Brödel’s line, which is 1 cm from the convex margin, is the bloodless plane demarcated by the distribution of the posterior branch of the renal artery.
The renal artery divides into anterior and posterior branches. The posterior branch supplies the midsegment of the posterior surface. The anterior branch supplies both upper and lower poles as well as the entire anterior surface. The renal arteries are all end arteries.
The renal artery further divides into interlobar arteries, which travel in the columns of Bertin (between the pyramids) and then arch along the base of the pyramids (arcuate arteries). These arteries then divide as interlobular arteries. From these vessels, smaller (afferent) branches pass to the glomeruli. From the glomerular tuft, efferent arterioles pass to the tubules in the stroma.
The renal veins are paired with the arteries, but any of them will drain the entire kidney if the others are tied off.
Although the renal artery and vein are usually the sole blood vessels of the kidney, accessory renal vessels are common and may be of clinical importance if they are so placed to compress the ureter, in which case hydronephrosis may result.
The renal nerves derived from the renal plexus accompany the renal vessels throughout the renal parenchyma.
Calices, Renal Pelvis, and Ureter
The tips of the minor calices (8–12 in number) are indented by the projecting pyramids (Figure 1–4). These calices unite to form two or three major calices that join to form the renal pelvis (Sozen et al, 2008).
The pelvis may be entirely intrarenal or partly intrarenal and partly extrarenal. Inferomedially, it tapers to join the ureter.
The adult ureter is about 30 cm long, varying in direct relation to the height of the individual. It follows a rather smooth S curve. Areas that stones are often impacted are (1) at the ureteropelvic junction, (2) where the ureter crosses over the iliac vessels, and (3) where it courses through the bladder wall.
The calices are intrarenal and are intimately related to the renal parenchyma.
If the pelvis is partly extrarenal, it lies along the lateral border of the psoas muscle and on the quadratus lumborum muscle; the renal vascular pedicle is just anterior to it. The left renal pelvis lies at the level of the first or second lumbar vertebra; the right pelvis is a little lower.
On their course downward, the ureters lie on the psoas muscles, pass medially to the sacroiliac joints, and then swing laterally near the ischial spines before passing medially to penetrate the base of the bladder (Figure 1–2). In females, the uterine arteries are closely related to the juxtavesical portion of the ureters. The ureters are covered by the posterior peritoneum; their lowermost portions are closely attached to it, while the juxtavesical portions are embedded in vascular retroperitoneal fat (Koff, 2008).
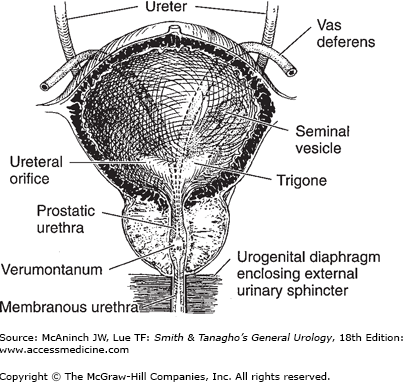
The vasa deferentia, as they leave the internal inguinal rings, sweep over the lateral pelvic walls anterior to the ureters (Figure 1–6). They lie medial to the latter before joining the seminal vesicle and penetrating the base of the prostate to become the ejaculatory ducts.
The walls of the calices, pelvis, and ureters are composed of transitional cell epithelium under which lies loose connective tissue (lamina propria). External to these are a mixture of helical and longitudinal smooth muscle fibers. They are not arranged in definite layers. The outermost adventitial coat is composed of fibrous connective tissue.
The renal calices, pelvis, and upper ureters derive their blood supply from the renal arteries; the midureter is fed by the internal spermatic (or ovarian) arteries. The lowermost portion of the ureter is served by branches from the common iliac, internal iliac (hypogastric), and vesical arteries.
The veins of the renal calices, pelvis, and ureters are paired with the arteries.
The lymphatics of the upper portions of the ureters as well as those from the pelvis and calices enter the lumbar lymph nodes. The lymphatics of the midureter pass to the internal iliac (hypogastric) and common iliac lymph nodes; the lower ureteral lymphatics empty into the vesical and hypogastric lymph nodes.
Bladder
The bladder is a hollow muscular organ that serves as a reservoir for urine. In women, its posterior wall and dome are invaginated by the uterus. The adult bladder normally has a capacity of 400–500 mL.
When empty, the adult bladder lies behind the pubic symphysis and is largely a pelvic organ. In infants and children, it is situated higher (Berrocal et al, 2002). When it is full, it rises well above the symphysis and can readily be palpated or percussed. When overdistended, as in acute or chronic urinary retention, it may cause the lower abdomen to bulge visibly.
Extending from the dome of the bladder to the umbilicus is a fibrous cord, the median umbilical ligament, which represents the obliterated urachus. The ureters enter the bladder posteroinferiorly in an oblique manner and at these points are about 5 cm apart (Figure 1–6). The orifices, situated at the extremities of the crescent-shaped interureteric ridge that forms the proximal border of the trigone, are about 2.5 cm apart. The trigone occupies the area between the ridge and the bladder neck.
The internal sphincter, or bladder neck, is not a true circular sphincter but a thickening formed by interlaced and converging muscle fibers of the detrusor as they pass distally to become the smooth musculature of the urethra.
In males, the bladder is related posteriorly to the seminal vesicles, vasa deferentia, ureters, and rectum (Figures 1–7 and 1–8). In females, the uterus and vagina are interposed between the bladder and rectum (Figure 1–9). The dome and posterior surfaces are covered by peritoneum; hence, in this area, the bladder is closely related to the small intestine and sigmoid colon. In both males and females, the bladder is related to the posterior surface of the pubic symphysis, and, when distended, it is in contact with the lower abdominal wall.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree