Anatomy and Embryology of the Anus, Rectum, and Colon
Ana Garza
Robert W. Beart Jr.
In anatomy, it is better to have learned and lost than never to have learned at all.
—W. SOMERSET MAUGHAM: Of Human Bondage
Although the need for an understanding of colonic, anorectal, and pelvic anatomy is consistent with the objective of a comprehensive textbook on colon and rectal surgery, little emphasis is placed on these subjects in training programs today. The most extensive observations had been made as early as 1543 by Andreas Vesalius through anatomic dissections. Several aspects, however, remain controversial. Anatomy of this region, especially that of the rectum and anal canal, is so intrinsically related to its physiology that much can be appreciated only in the living. Therefore, it is a region in which the colorectal surgeon has an advantage over the anatomist through in vivo dissection, physiologic investigation, and endoscopic examination. More recently, the accumulated experience with diverse operative techniques such as the ileoanal procedure has added to advances in our understanding of continence and has demanded more in-depth knowledge of the anatomy and physiology of the large intestine.33,51,52,57,121,122 and 123
▶ EMBRYOLOGY
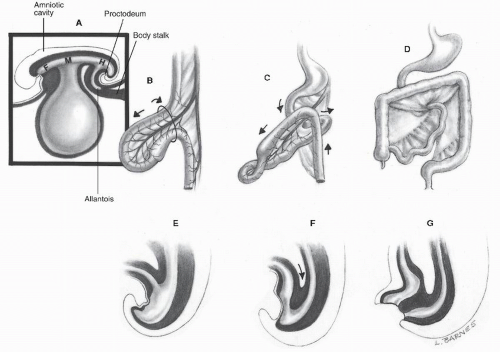
The primitive gut tube develops from the endodermal roof of the yolk sac. At the beginning of the third week of development, it can be divided into three regions: the foregut in the head fold; the hindgut with its ventral allantoic outgrowth in the smaller tail fold; and, between these two portions, the midgut, which at this stage opens ventrally into the yolk sac (Figure 1-1). After the stages of physiologic herniation, return to the abdomen, and fixation, the midgut progresses below the major pancreatic papilla to form the small intestine, the ascending colon, and the proximal two-thirds of the transverse colon. This segment is supplied by the midgut (superior mesenteric) artery, with corresponding venous and lymphatic drainage.106 The sympathetic innervation of the midgut and likewise the hindgut originates from T8 to L2 via splanchnic nerves and the autonomic abdominopelvic plexuses. The parasympathetic outflow to the midgut is derived from the 10th cranial nerve (vagus) with preganglionic cell bodies in the brain stem.
The distal colon (distal third of the transverse colon), the rectum, and the anal canal above the dentate line are all derived from the hindgut. Therefore, this segment is supplied by the hindgut (inferior mesenteric) artery with corresponding venous and lymphatic drainage. Its parasympathetic outflow comes from S2, S3, and S4 via splanchnic nerves.
The dentate line marks the fusion between endodermal and ectodermal tubes, where the terminal portion of the hindgut or cloaca fuses with the proctodeum, an ingrowth from the anal pit. The cloaca originates at the portion of the rectum below the pubococcygeal line, whereas the hindgut originates above it. Before the fifth week of development, the intestinal and urogenital tracts terminate in conjunction with the cloaca. At the sixth week, the urorectal septum migrates caudally, and the two tracts are separated. The cloacal part of the anal canal, which has both endodermal and ectodermal elements, forms the anal
transitional zone after breakdown of the anal membrane.106 During the 10th week, the anal tubercles, a pair of ectodermal swellings around the proctodeal pit, fuse dorsally to form a horseshoe-shaped structure and anteriorly to create the perineal body. The cloacal sphincter is separated by the perineal body into urogenital and anal portions (external anal sphincter [EAS]). The internal anal sphincter (IAS) is formed later (6th to 12th week) from enlarging fibers of the circular layer of the rectum.66,87 The sphincters apparently migrate during their development; the external sphincter grows cephalad, and the internal sphincter moves caudally. Concomitantly, the longitudinal muscle descends into the intersphincteric plane.66,127
transitional zone after breakdown of the anal membrane.106 During the 10th week, the anal tubercles, a pair of ectodermal swellings around the proctodeal pit, fuse dorsally to form a horseshoe-shaped structure and anteriorly to create the perineal body. The cloacal sphincter is separated by the perineal body into urogenital and anal portions (external anal sphincter [EAS]). The internal anal sphincter (IAS) is formed later (6th to 12th week) from enlarging fibers of the circular layer of the rectum.66,87 The sphincters apparently migrate during their development; the external sphincter grows cephalad, and the internal sphincter moves caudally. Concomitantly, the longitudinal muscle descends into the intersphincteric plane.66,127
▶ ANATOMY OF THE COLON
The colon, so named from the Greek koluein (“to retard”), is a capacious tube described in humans to be somewhere between the short, straight type with a rudimentary cecum, such as that of the carnivores, and a long, sacculated colon with a capacious cecum, such as that of the herbivores. The colon roughly surrounds the loops of small intestine as an arch. Its length in the adult is variable, averaging approximately 150 cm, about one-fourth the length of the small intestine. Its diameter, which can be substantially augmented by distension, gradually decreases from 7.5 cm at the cecum to 2.5 cm at the sigmoid.
Anatomic differences between the small and large intestines include position; caliber; degree of fixation; and, in the colon, the presence of three distinct characteristics: the taeniae coli, the haustra, and the appendices epiploicae. The three taeniae coli, anterior (taenia libera), posteromedial (taenia mesocolica), and posterolateral (taenia omentalis), represent bands of the outer longitudinal coat of muscle that traverse the colon from the base of the appendix to the rectosigmoid junction where they merge. The muscular longitudinal layer is actually a complete coat around the colon, although it is considerably thicker at the taeniae.35 The haustra or haustral sacculations are outpouchings of bowel wall between the taeniae; they are caused by the relative shortness of the taeniae, about one-sixth shorter than the length of bowel wall.83 The haustra are separated by the plicae semilunares or crescentic folds of the bowel wall, which give the colon its characteristic radiographic appearance when filled with air or barium. The appendices epiploicae are small appendages of fat that protrude from the serosal aspect of the colon (Figure 1-2).
Cecum
The cecum is the segment of the large bowel that projects downward as a blind pouch (Latin caecus, “blind”) below the entrance of the ileum. It is a sacculated organ of 6 to 8 cm in both length and breadth, usually situated in the right iliac fossa. The cecum is almost entirely, or at least in its lower
half, invested with peritoneum. However, its mobility is usually limited by a small mesocecum. In approximately 5% of individuals, the peritoneal covering is absent posteriorly; it then rests directly on the iliacus and psoas major muscles.41 Alternatively, an abnormally mobile cecum-ascending colon, resulting from an anomaly of fixation, can be found in 10% to 22% of individuals.98 In this case, a long mesentery is present, and the cecum may assume varied positions. This lack of fixation may predispose to the development of volvulus (see Chapter 28).
half, invested with peritoneum. However, its mobility is usually limited by a small mesocecum. In approximately 5% of individuals, the peritoneal covering is absent posteriorly; it then rests directly on the iliacus and psoas major muscles.41 Alternatively, an abnormally mobile cecum-ascending colon, resulting from an anomaly of fixation, can be found in 10% to 22% of individuals.98 In this case, a long mesentery is present, and the cecum may assume varied positions. This lack of fixation may predispose to the development of volvulus (see Chapter 28).
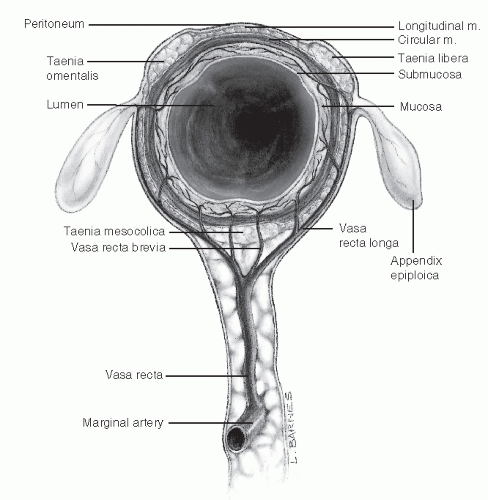 FIGURE 1-2. Cross section of the colon and mesocolon demonstrates the arrangement of the vasa recta and their branches. |
The ileum terminates in the posteromedial aspect of the cecum; the angulation between these two structures is maintained by the superior and inferior ileocecal ligaments. These ligaments, along with the mesentery of the appendix, form three pericecal recesses or fossae: superior ileocecal, inferior ileocecal, and retrocecal (Figure 1-3). Viewed from the cecal lumen, the ileocecal junction is represented by a narrow, transversely situated, slitlike opening known as the ileocecal valve or the valve de Bauhin. At either end, the two prominent semilunar lips of the valve fuse and continue as a single frenulum of mucosa. A competent ileocecal valve is related to the critical closed-loop type of colonic obstruction. However, ileocecal competence is not always demonstrated on barium enema studies. Instead of preventing reflux of colonic contents into the ileum, the ileocecal valve regulates ileal emptying. The ileocecal valve seems to relax in response to the entrance of food into the stomach.48
As in the gastroesophageal junction, extrasphincteric factors apparently play a role in the prevention of reflux from the colon to the ileum. The ileocecal angulation has been emphasized by Kumar and Phillips.61 They filled the ascending colon with saline solution in a retrograde fashion and found that the ileocecal junction was competent to pressures up to 80 mm Hg in 12 of 14 human autopsy specimens. In this group, removal of mucosa at the ileocecal junction or a strip of circular muscle did not impair competence to pressures above 40 mm Hg, but division of the superior and inferior ileocecal ligaments rendered the junction incompetent in all specimens. Furthermore, surgical reconstruction of the ileocecal angle restored competence in four of them.
Appendix
The vermiform appendix is an elongated diverticulum that arises from the posteromedial aspect of the cecum about 3 cm below the ileocecal junction. Its length varies from 2 to 20 cm
(mean, 8 to 10 cm), and it is approximately 5 mm in diameter. The confluence of the three taeniae is a useful guide in locating the base of the appendix. The appendix, because of its great mobility, may occupy a variety of positions, possibly at different times in the same individual: retrocecal (65%), pelvic (31%), subcecal (2.3%), preileal (1.0%), and retroileal (0.4%) (Figure 1-4).116 Some authors have found, however, that in 85% to 95% it lies posteromedial on the cecum toward the ileum.106 The mesoappendix, a triangular fold attached to the posterior leaf of the mesentery of the terminal ileum, usually contains the appendicular vessels close to its free edge.
(mean, 8 to 10 cm), and it is approximately 5 mm in diameter. The confluence of the three taeniae is a useful guide in locating the base of the appendix. The appendix, because of its great mobility, may occupy a variety of positions, possibly at different times in the same individual: retrocecal (65%), pelvic (31%), subcecal (2.3%), preileal (1.0%), and retroileal (0.4%) (Figure 1-4).116 Some authors have found, however, that in 85% to 95% it lies posteromedial on the cecum toward the ileum.106 The mesoappendix, a triangular fold attached to the posterior leaf of the mesentery of the terminal ileum, usually contains the appendicular vessels close to its free edge.
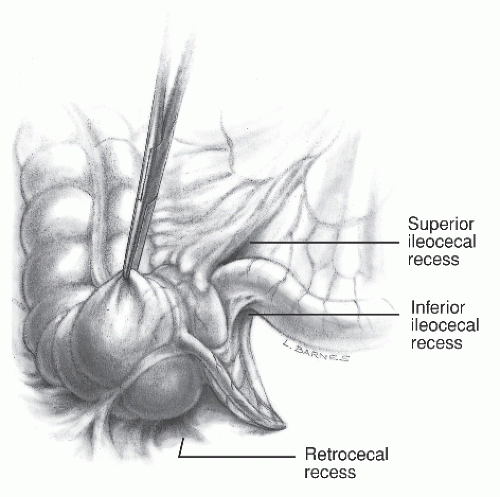 FIGURE 1-3. Ileocecal region. The superior ileorectal, inferior ileocecal, and rectocecal recesses are shown. |
Ascending Colon
The ascending colon, extending from the level of the ileocecal junction to the right colic or hepatic flexure, is approximately 15 cm long. It ascends laterally to the psoas muscle and anteriorly to the iliacus, the quadratus lumborum, and the lower pole of the right kidney. The ascending colon is covered with peritoneum anteriorly and on both sides. In addition, fragile adhesions between the right abdominal wall and its anterior aspect, known as Jackson’s membrane, may be present.86 Like the descending colon on its posterior surface, the ascending colon is devoid of peritoneum, which is instead replaced by an areolar tissue (fascia of Toldt), resulting from an embryologic process of fusion or coalescence of the mesentery to the posterior parietal peritoneum.106 In the lateral peritoneal reflection, this process is represented by the white line of Toldt, which is more evident at the descending sigmoid junction. This line serves as a guide for the surgeon when the ascending, descending, or sigmoid colon is mobilized.
At the visceral surface of the right lobe of the liver and lateral to the gallbladder, the ascending colon turns sharply medially and slightly caudad and ventrally to form the right colic (hepatic) flexure (see Figure 22-39). This flexure is supported by the nephrocolic ligament and lies immediately ventral to the lower part of the right kidney and over the descending duodenum.
Relationship to Ureters
In resections of the right and left colon, identification of the ureters is usually necessary to avoid injury to their abdominal or pelvic portions.74 On both sides, the ureters rest on the psoas muscle in their inferomedial course; they are crossed obliquely by the spermatic vessels anteriorly and the genitofemoral nerve posteriorly. The right ureter lies lateral to the inferior vena cava and is crossed anteriorly by the right colic and ileocolic arteries, the root of the mesentery, and the terminal ileum. In its pelvic portion, the ureter crosses the pelvic brim in front of or a little lateral to the bifurcation of the common iliac artery, and it descends abruptly between the peritoneum and the internal iliac artery. Before entering the bladder in the male, the vas deferens crosses lateromedially on its superior aspect. In the female, as the ureter traverses the posterior layer of the broad ligament and the parametrium close to the side of the neck of the uterus and upper part of the vagina, it is enveloped by the vesical and vaginal venous plexuses and is crossed above and lateromedially by the uterine artery.
Transverse Colon
The transverse colon is the longest segment of the large bowel (45 cm long). It crosses the abdomen, usually with an inferior curve immediately caudad to the greater curvature of the stomach. The transverse colon is relatively fixed at each flexure. In between, it is completely invested with peritoneum and suspended by a transverse mesocolon having an average width of 10 to 15 cm and providing variable mobility; the nadir of the transverse colon may reach the hypogastrium. The greater omentum is fused on the anterosuperior aspect of the transverse colon. Therefore, an intercoloepiploic dissection is necessary to mobilize this portion of the colon or to enter the lesser sac of the peritoneum. The left colic (splenic) flexure is situated beneath the lower angle of the spleen and firmly attached to the diaphragm by the phrenocolic ligament, which also forms a shelf to support the spleen (see Figure 23-49). Because of the risk for hemorrhage, mobilization of the splenic flexure should be approached with great care, preceded by dissection upward along the descending colon and medially to laterally along the transverse colon toward the splenic flexure (see Chapter 23). This flexure, when compared with the hepatic flexure, is more acute, higher, and more deeply situated.
Descending Colon
This segment of the large intestine courses downward from
the splenic flexure to the brim of the true pelvis, a distance of approximately 25 cm. The segment of descending colon between the iliac crest and the brim of the true pelvis is also known as the iliac colon.41 Like the ascending colon, the descending colon is covered by peritoneum only on its anterior and lateral aspects. Posteriorly, it rests directly against the left kidney and the quadratus lumborum and transversus abdominis muscles. However, the descending colon is narrower and more dorsally situated than the ascending colon.
Sigmoid Colon
The sigmoid colon, extending from the lower end of the descending colon at the pelvic brim to the proximal limit
of the rectum, varies dramatically in length (15 to 50 cm; mean, 38 cm) and configuration. More commonly, the sigmoid colon is a mobile, ω-shaped loop completely invested by peritoneum. The mesosigmoid is attached to the pelvic walls in an inverted V shape, resting in a recess known as the intersigmoid fossa. The left ureter lies immediately underneath this fossa and is crossed on its anterior surface by the spermatic, left colic, and sigmoid vessels.
of the rectum, varies dramatically in length (15 to 50 cm; mean, 38 cm) and configuration. More commonly, the sigmoid colon is a mobile, ω-shaped loop completely invested by peritoneum. The mesosigmoid is attached to the pelvic walls in an inverted V shape, resting in a recess known as the intersigmoid fossa. The left ureter lies immediately underneath this fossa and is crossed on its anterior surface by the spermatic, left colic, and sigmoid vessels.
Rectosigmoid Junction
Both the anatomy and function of the rectosigmoid junction have been matters of substantial controversy. O’Beirne postulated that because the rectum is usually emptied and contracted, the sigmoid plays a role in continence as the fecal reservoir.88 Subsequently, a thickening of the circular muscular layer between the rectum and sigmoid was described and diversely termed the sphincter ani tertius,54 rectosigmoid sphincter,73 and pylorus sigmoidorectalis,16 and it has probably been mistaken for one of the transverse folds of the rectum.53,91 Balli considered the rectosigmoid junction to be one of the functional sphincters of the colon.5 The rectosigmoid junction has been considered, at least externally, an indistinct zone, a region that to some surgeons comprises the last 5 to 8 cm of sigmoid and the uppermost 5 cm of the rectum.31,41 However, surgeons as well as anatomists have divergent opinions. Others have considered it a clearly defined segment because it is the narrowest portion of the large intestine; in fact, it is usually characterized endoscopically as a narrow and sharply angulated segment.14,105 Stoss, in a study of 39 human cadavers, found the rectosigmoid junction situated 6 to 7 cm below the sacral promontory.110 Macroscopically, it has been identified as the point where the taenia libera and the taenia omentalis fuse to form a single anterior taenia and where both haustra and mesocolon terminate. With microdissection, this segment is characterized by conspicuous strands of longitudinal muscle fibers that are more prominent than in the sigmoid and less so than in the rectum. Additionally, curved interconnecting fibers between the longitudinal and circular muscle layers have been noted, resulting in a delicate syncytium of smooth muscle that allows synergistic interplay between the two layers. Stoss concluded, based on the anatomic definition of a sphincter as “a band of thickened circular muscle that closes the lumen by contraction and of a longitudinal muscle that dilates it,” that the rectosigmoid cannot be considered as such.67,110 Still, this segment may be regarded as a functional sphincter because mechanisms of active dilation and passive “kinking” occlusion do exist.108
Rectum
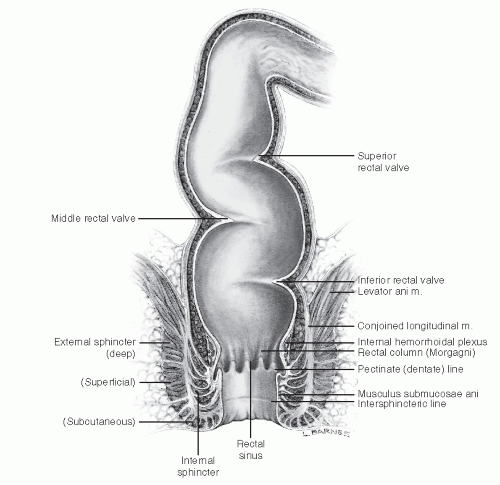
The rectum is believed to be 12 to 15 cm in length, but both the proximal and distal limits are debatable (Figure 1-5).127 For example, the rectosigmoid junction is considered to be
at the level of the third sacral vertebra by anatomists but at the coalescence of taeniae coli by surgeons. Likewise, the distal limit is regarded to be the muscular anorectal ring by surgeons and the dentate line by anatomists. The rectum occupies the sacral concavity and ends 2 to 3 cm anteroinferiorly from the tip of the coccyx. At this point, it angulates backward sharply to pass through the levators and becomes the anal canal. The median sacral vessels and the roots of the sacral nerve plexus lie posterior to the rectum. Anteriorly, in women, the rectum is closely related to the uterine cervix and posterior vaginal wall; in men, it lies behind the bladder, vas deferens, seminal vesicles, and prostate.
at the level of the third sacral vertebra by anatomists but at the coalescence of taeniae coli by surgeons. Likewise, the distal limit is regarded to be the muscular anorectal ring by surgeons and the dentate line by anatomists. The rectum occupies the sacral concavity and ends 2 to 3 cm anteroinferiorly from the tip of the coccyx. At this point, it angulates backward sharply to pass through the levators and becomes the anal canal. The median sacral vessels and the roots of the sacral nerve plexus lie posterior to the rectum. Anteriorly, in women, the rectum is closely related to the uterine cervix and posterior vaginal wall; in men, it lies behind the bladder, vas deferens, seminal vesicles, and prostate.
JOHN HOUSTON (1802-1845)
 |
Born in the north of Ireland, Houston was adopted by a physician uncle. He attached himself to one of the first native Dublin anatomists and became a curator of the museum of the Royal College of Surgeons in Ireland in 1824. In 1826, he received his medical degree from Edinburgh University. On the establishment of the City of Dublin Hospital in 1832, Houston became one of its surgeons. He was regarded as an acute observer of disease and an excellent clinical surgeon. In 1830, he published the report in which he described the valves that bear his name. He died while lecturing, presumably of complications of an intracranial hemorrhage. (Houston J. Observations of the mucous membrane of the rectum. Dublin Hosp Rep Communications Med Surg. 1830;5:158-165.)
The nonmobilized rectum has three lateral curves: the upper and lower are convex to the right and the middle is convex to the left (Figure 1-5). These curves correspond intraluminally to the folds or valves of Houston.2,53 The two left-sided folds are usually noted at 7 to 8 cm and at 12 to 13 cm, respectively, and the one on the right is generally at 9 to 11 cm. The middle valve is the most consistent in presence and location (also known as Kohlrausch’s plica) and corresponds to the level of the anterior peritoneal reflection. The rectal valves do not contain all the muscle wall layers and do not have a specific function. However, from a clinical point of view, they are an excellent location for performing a rectal biopsy because they are readily accessible with minimal risk for perforation.86 The valves of Houston must be negotiated during proctosigmoidoscopy. However, they are not present after mobilization of the rectum; this is attributed to the 5-cm length gained following complete surgical dissection.
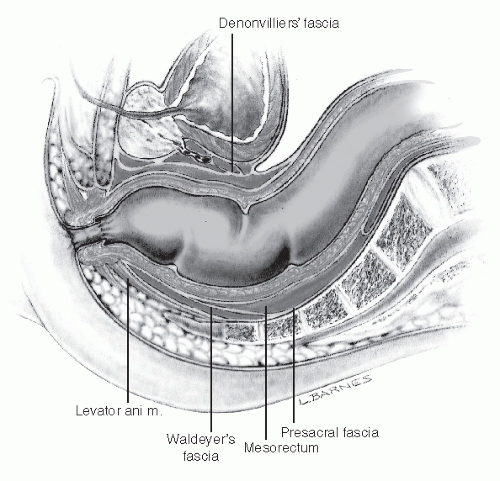 FIGURE 1-6. Lateral view of the male rectum illustrating the mesorectum and its relationship with other pelvic structures. |
The rectum is characterized by the absence of taeniae, epiploic appendices, haustra, or a well-defined mesentery. The prefix “meso,” in gross anatomy, refers to two layers of peritoneum that suspend an organ. Normally, the rectum is not suspended but entirely extraperitoneal on its posterior aspect and close to the sacral hollow. Consequently, the term mesorectum is anatomically inappropriate.18,81 An exception, however, is that a peritonealized mesorectum may be noted in patients with procidentia. Nonetheless, the term mesorectum has gained widespread popularity among surgeons to address the perirectal adipose tissue, which is thicker posteriorly, containing terminal branches of the inferior mesenteric artery, lymph nodes, and enclosed by the fascia propria (Figure 1-6).17,52,59 The mesorectum may be a metastatic site for rectal cancer and is removed during surgery for rectal
cancer (see Chapter 24). Its removal is undertaken without clinical sequelae because no functionally significant nerves pass through it.52 Although it is quite variable, in classical descriptions, the upper third of the rectum is anteriorly and laterally invested by peritoneum; the middle third is covered by peritoneum on its anterior aspect only. Finally, the lower third of the rectum is entirely extraperitoneal because the anterior peritoneal reflection occurs at 9.0 to 7.0 cm from the anal verge in men and at 7.5 to 5.0 cm from the anal verge in women.
cancer (see Chapter 24). Its removal is undertaken without clinical sequelae because no functionally significant nerves pass through it.52 Although it is quite variable, in classical descriptions, the upper third of the rectum is anteriorly and laterally invested by peritoneum; the middle third is covered by peritoneum on its anterior aspect only. Finally, the lower third of the rectum is entirely extraperitoneal because the anterior peritoneal reflection occurs at 9.0 to 7.0 cm from the anal verge in men and at 7.5 to 5.0 cm from the anal verge in women.
The rectum has a wide, easily distensible lumen. The rectal mucosa is smooth, pink, and transparent, which allows visualization of small and large submucosal vessels. This characteristic vascular pattern disappears in inflammatory conditions and in melanosis coli.
Fascial Relationship of the Rectum
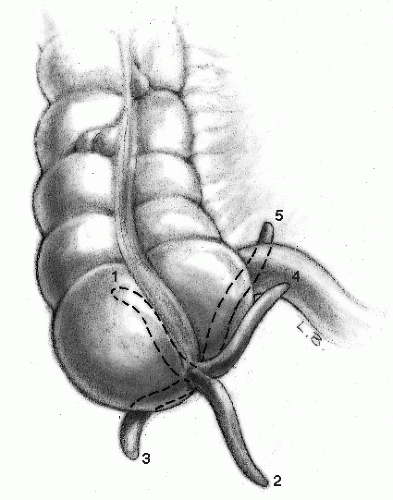
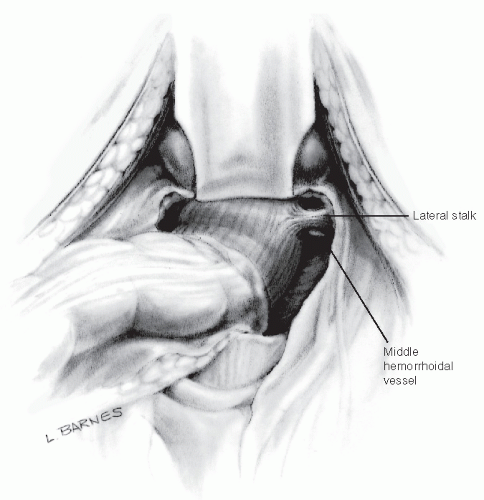
The walls and floor of the pelvis are lined by the parietal endopelvic fascia, which continues on the internal organs as a visceral pelvic fascia. The fascia propria of the rectum is therefore an extension of the pelvic fascia, enclosing the rectum, fat, nerves, and the blood and lymphatic vessels. It is present mainly in the lateral and posterior extraperitoneal portion of the rectum. Distal condensations of this fascia form the lateral ligaments or lateral stalks of the rectum. These are described by Goligher as a roughly triangular structure with a base on the lateral pelvic wall and an apex attached to the lateral aspect of the rectum.41 As pointed out by Church and colleagues, these ligaments have been the subject of anatomic confusion and misconception.20 One such misconception is that they are composed essentially of connective tissue and nerves, and that the middle rectal artery traverses the lateral stalks of the rectum. Minor branches of the middle rectal artery course through the lateral stalks in approximately 25% of cases.13,126 Consequently, division of the lateral stalks during rectal mobilization is associated with a 25% risk for bleeding. Although the lateral stalks do not contain important structures, the middle rectal artery and the pelvic plexus are both closely related, coursing at different angles beneath them in various patients.85 One theoretical concern in ligation of the stalks is leaving behind lateral mesorectal tissue, which may limit adequate lateral or mesorectal margins during cancer surgery (Figure 1-7).17,52,97
The presacral fascia is a thickened part of the parietal endopelvic fascia that covers the concavity of the sacrum and coccyx, nerves, the middle sacral artery, and presacral veins (Figure 1-8). Operative dissection deep to the presacral fascia may cause troublesome bleeding from the underlying presacral veins. The incidence of such hemorrhage has been cited to be as high as 4.6% to 7.0% of resections for rectal neoplasms.57,118,128 These veins are avalvular and communicate via the basivertebral veins with the internal vertebral venous system (Figure 1-8). With the patient in the lithotomy position, this system can attain hydrostatic pressures of 17 to 23 cm H2O, two to three times the normal pressure of the inferior vena cava.118 The adventitia of the basivertebral veins adheres firmly to the sacral periosteum at the level of the ostia of the sacral foramina (mainly at the level of S3-4).118 Despite its venous nature, presacral
hemorrhage can be life threatening. This is a consequence of the high hydrostatic pressure and the difficulty in securing control because of retraction of the vascular stump into the sacral foramen.
hemorrhage can be life threatening. This is a consequence of the high hydrostatic pressure and the difficulty in securing control because of retraction of the vascular stump into the sacral foramen.
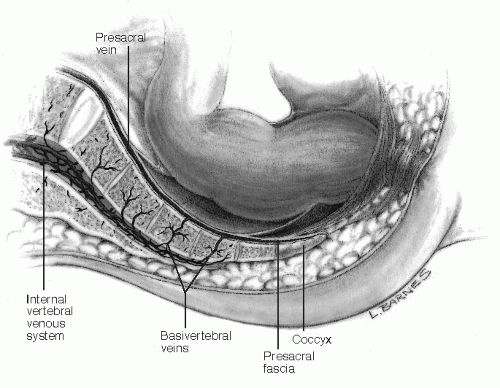 FIGURE 1-8. Sagittal section of the pelvis showing the fascial relationships of the rectum and the presacral and vertebral venous system. |
The rectosacral fascia is an anteroinferiorly directed thick fascial reflection from the presacral fascia at the S4 level to the fascia propria of the rectum just above the anorectal ring.23 The rectosacral fascia, an important landmark during posterior rectal dissection, is classically known as the fascia of Waldeyer, but this is a misnomer because Wilhelm Waldeyer first described all of the pelvic fascia, not particularly emphasizing the rectosacral fascia.20,23 Anteriorly, the extraperitoneal rectum is separated from the prostate and seminal vesicles or vagina by a tough fascial investment, the visceral pelvic fascia of Denonvilliers.114 Therefore, three structures lie between the anterior rectal wall and the seminal vesicles and prostate: the anterior mesorectum, the fascia propria of the rectum, and Denonvilliers’ fascia (Figure 1-6). A general consensus has been reached regarding the anatomic plane of posterior and lateral rectal dissection. However, anteriorly the matter is more controversial. Most would accept
the appropriateness of dissection in the plane between Denonvilliers’ fascia and the fascia propria. The use of the terms close rectal, mesorectal, and extramesorectal have been suggested to describe the anterior planes.69 The close rectal plane, also known as the perimuscular plane, lies immediately on the rectal musculature, inside the fascia propria of the rectum. However, it is more difficult to navigate, bloodier than the mesorectal plane, and consequently is not considered a true anatomic plane. The mesorectal plane represents the continuation of the same plane of posterior and lateral dissection of the rectum. It is the appropriate anterior plane for most rectal cancers, a natural anatomic plane that is familiar to colorectal surgeons. Finally, the extramesorectal plane involves resection of Denonvilliers’ fascia, with exposure of the prostate and seminal vesicles. This plane is associated with a high risk of both parasympathetic and sympathetic injury to the periprostatic plexus. In addition, dissection in this plane generally predisposes to an increased risk of intraoperative hemorrhage.
the appropriateness of dissection in the plane between Denonvilliers’ fascia and the fascia propria. The use of the terms close rectal, mesorectal, and extramesorectal have been suggested to describe the anterior planes.69 The close rectal plane, also known as the perimuscular plane, lies immediately on the rectal musculature, inside the fascia propria of the rectum. However, it is more difficult to navigate, bloodier than the mesorectal plane, and consequently is not considered a true anatomic plane. The mesorectal plane represents the continuation of the same plane of posterior and lateral dissection of the rectum. It is the appropriate anterior plane for most rectal cancers, a natural anatomic plane that is familiar to colorectal surgeons. Finally, the extramesorectal plane involves resection of Denonvilliers’ fascia, with exposure of the prostate and seminal vesicles. This plane is associated with a high risk of both parasympathetic and sympathetic injury to the periprostatic plexus. In addition, dissection in this plane generally predisposes to an increased risk of intraoperative hemorrhage.
HEINRICH WILHELM GOTTFRIED VON WALDEYER-HARTZ (1836-1921)
 |
Waldeyer was born on October 6, 1836 in Helen an der Weser, Germany, the son of an estate manager and a school teacher. He received his early education at Paderborn. In 1856, he entered the University of Göttingen to study mathematics and natural sciences. However, through his acquaintance with the anatomist Friedrich Henle, whose lectures he attended, he began the study of medicine. Waldeyer attended the University of Göttingen from 1856 to 1859. As a Prussian, he could not complete his studies, and he transferred to Greifswald, where he became an assistant in the Anatomical Institute. He then moved on to Berlin to pursue his great interest in anatomy, obtaining his doctorate in 1861. There followed a series of appointments to the University of Königsberg and the University of Breslau. In 1868, at the age of 32, he was appointed to the chair of pathology at Breslau. His work at this time was chiefly concentrated on the diagnosis of early cancer. In 1887, he was one of the German doctors called upon to diagnose Emperor Frederick III’s vocal cord tumor. In 1872, Waldeyer went to the University of Strasbourg as chair of anatomy. He remained there for 11 years, returning in 1883 to Berlin, where he eventually taught anatomy to more than 20,000 students. He published numerous papers on a wide variety of anatomic subjects, including studies of the urogenital system, anthropology, and topographical observations of the pelvis (Waldeyer’s fascia). Today, Wilhelm von Waldeyer-Hartz is remembered as the founder of the neuron theory, coining the term “neuron” to describe the cellular unit of the nervous system (1891). He also coined the term “chromosome” (1888) to describe the bodies in the nucleus of cells. Waldeyer remained at the University of Berlin until he was 80 years old. He died in Berlin on January 23, 1921. (With appreciation to Faisal Aziz, MD. Figure courtesy of the National Library of Medicine.)
CHARLES-PIERRE DENONVILLIERS (1808-1872)
 |
Son of a landlord, Denonvilliers was born in Paris on February 4, 1808. He studied medicine at the Paris Faculty, from which he graduated in 1835. His first post was that of surgeon to the Bureau Central (1840). In 1842, he became chief of the School of Practical Anatomy of the Hôtel-Dieu, and in 1856 he achieved the position as professor of surgery at the same institution. Denonvilliers’ interests resided more in anatomy than in surgery. Through the years, he made numerous and varied contributions to the field, including a description of the fascia for which he achieved eponymous immortality. In 1836, Denonvilliers reported to the Société Anatomique concerning an “aponeurosis” as follows: “Behind the prostate and between the seminal vesicles and the rectum, there is a distinct membranous layer, which I call prostatoperitoneal.” In 1858, Denonvilliers was awarded the important position of inspector general of Public Instruction for Medicine. Through this role, he has been credited with modernizing the French medical curriculum by the development of new concepts in the teaching of physiology, pathology, and surgery. His extensive work in the field of descriptive and surgical anatomy led to the publication of numerous articles and textbooks as well as to the elaboration of innovative surgical techniques, particularly in the field of reconstructive plastic surgery. His professional activity ceased in 1864 with the death of his prematurely born son, a tragedy from which he never fully recovered. Thought to be a great loss to the field of medical science by his contemporaries, Denonvilliers died of a stroke on July 5, 1872. (With appreciation to Keith P. Meslin, MD.)
Anal Canal
Although representing a relatively small segment of the digestive tract, the anal canal is anatomically unique, with a complex physiology that accounts for both its vital role in continence and its susceptibility to a variety of diseases. In the literature, two definitions are found to describe the anal canal. The “surgical” or “functional” anal canal extends for approximately 4 cm from the anal verge to the anorectal ring. This definition correlates with both digital and sonographic assessment, but it does not correspond to either the embryologic or histologic architecture of the anal canal. The “anatomic” or “embryologic” anal canal is shorter (2 cm), extending from the anal verge to the dentate line (see Figure 11-2). The latter is the level that corresponds to the proctodeal membrane.87,127
The anus or anal orifice is an anteroposterior cutaneous slit that, along with the anal canal, remains virtually closed at rest. This is the result of tonic circumferential contraction of both the sphincters and the anal cushions. Posteriorly, the anal canal is related to the coccyx and anteriorly to the urethra (in the male) and to the perineal body and the lowest part of the posterior vaginal wall (in the female). Laterally, the ischiorectal fossa is situated on either side. The fossa contains fat and the inferior rectal vessels and nerves, which cross it to enter the wall of the anal canal.
Epithelium
The lining of the anal canal consists of an upper mucosal and a lower cutaneous segment. The dentate (pectinate) line describes the “saw-toothed” junction of the ectoderm and the endoderm. It therefore represents an important landmark between two distinct origins of venous and lymphatic drainage, nerve supply, and epithelial lining.125 Above the dentate line, the intestine is innervated by the sympathetic and parasympathetic systems, with venous, arterial, and lymphatic drainage to and from the hypogastric vessels. Distal to the dentate line, the anal canal is innervated by the somatic nervous system, with blood supply and drainage from the inferior hemorrhoidal system. These differences are important when the classification and treatment of hemorrhoids are considered.
The pectinate or dentate line corresponds to a line of anal valves that represent remnants of the proctodeal membrane. Above each valve, there is a little pocket known as an anal sinus or crypt. These crypts are connected to a variable number of glands, with an average of six (range, 3 to 12 crypts per patient [see Figures 25-1 and 25-2]).43,68 The anal glands are more concentrated in the posterior quadrants. More than one gland may open into the same crypt, whereas half the crypts have no communication. The anal gland ducts enter the submucosa in an outward and downward route; two-thirds enter the IAS, and half of them terminate in the intersphincteric plane (see Figures 25-3 and 13-1).68 The anal glands were first
described by Chiari in 1878, but it was not until 1961 that Parks addressed their role in the pathogenesis of fistulous abscess19,93 (see Chapters 13 and 14). Obstruction of these ducts, presumably by accumulation of foreign material in the crypts, may lead to abscesses and fistula.93
described by Chiari in 1878, but it was not until 1961 that Parks addressed their role in the pathogenesis of fistulous abscess19,93 (see Chapters 13 and 14). Obstruction of these ducts, presumably by accumulation of foreign material in the crypts, may lead to abscesses and fistula.93
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree