■ The perineum is positioned flush with the edge of the operating room table.
■ The pelvis is supported with a folded sheet to lift the entire perineum and facilitate exposure during the perineal dissection.
■ The arms are placed in a neutral position and supported with suitable armrests.
■ The anus is closed with a purse-string monofilament suture (0-Prolene with circle taper 1 [CT-1] Ethicon needle, or equivalent).
■ For the abdominal phase of the operation, the surgeon stands by the patient’s right side, with his or her assistant standing at the patient’s left side. A second assistant, if available, stands in between the patient’s legs. The scrub nurse stands at the surgeon’s right side, by the patient’s right leg (FIG 2). The surgeon and the first assistant will switch sides as necessary during the pelvic dissection.
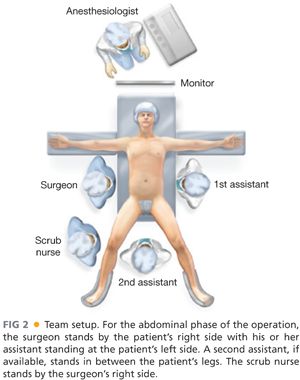
■ During the perineal phase, the surgeon and the first assistant will be situated in between the patient’s legs, with the second assistant by the patient’s right or left side.
TECHNIQUES
EXPOSURE
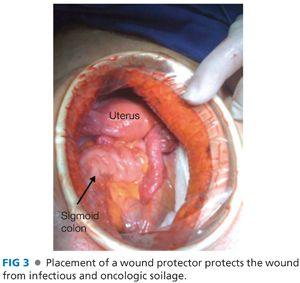
■ Exposure of the abdomen is obtained with a lower midline incision from the umbilicus to the pubic symphysis. A wound protector may be inserted to protect the wound from infectious and oncologic soilage (FIG 3).
■ The abdomen should be fully explored for the presence of gross metastatic disease.
■ Care should be taken to evaluate all peritoneal surfaces, the entire gastrointestinal tract, the omentum, and the liver.
■ Any concerning lesions away from the primary tumor should be biopsied and evaluated by intraoperative cryosection.
■ A self-retaining retractor is positioned to optimize exposure of the pelvis.
■ Two short Richardson attachments are used to retract the abdominal wall laterally, in a perpendicular orientation to the incision to avoid undue traction on the femoral nerves at the pelvic inlet (FIG 4).
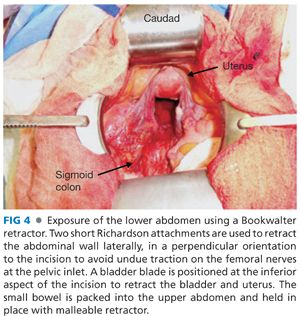
■ A bladder blade is positioned at the inferior aspect of the incision to retract the bladder and uterus. A 2-0 silk, figure-of-eight suture through the fundus of the uterus can facilitate positioning the uterus behind the bladder blade.
■ The small bowel is packed into the upper abdomen; this maneuver is facilitated by not extending the incision beyond what is required to access the origin of the inferior mesenteric artery.
■ A malleable retractor attachment for the Bookwalter and moistened laparotomy pads aid in keeping the small bowel out of the pelvis.
Mobilization of Sigmoid Colon and Transection of the Inferior Mesenteric Artery
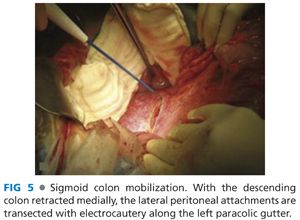
■ The lateral peritoneal attachments to the sigmoid colon are divided, exposing the plane between the sigmoid mesocolon and the retroperitoneum (FIG 5).
■ Mobilization of the sigmoid mesocolon allows for exposure and preservation of the left ureter and gonadal vessels, which should always be identified prior to dividing the inferior mesenteric artery at its origin (FIG 6).
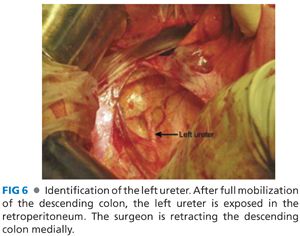
■ The left ureter courses over the left psoas and is located medial to the gonadal vessels; it travels over the left iliac artery at its bifurcation at the pelvic inlet.
■ Direct exposure of the left psoas often indicates an incorrect dissection plane where the ureter and gonadal vessels are mobilized medially with the sigmoid mesocolon.
■ The peritoneal reflection on the right side of the sigmoid mesocolon is incised to complete the dissection of the mesentery away from the retroperitoneum. Again, care must be taken to maintain the ureter in its normal, anatomic position in the retroperitoneum.
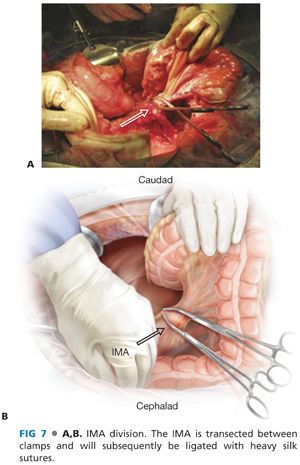
■ The origin of the inferior mesenteric artery (IMA) is identified at its origin off the aorta. The IMA is then ligated between Sarot clamps, incised, and doubly ligated with braided 2-0 suture (FIG 7A,B). High IMA ligation allows for an excellent lymph node harvest.
■ The colon is then transected proximally between the sigmoid and descending colon segments with a linear stapler. The intervening mesentery is divided with an energy device.
Mobilization of the Rectum
■ Once the sigmoid mesocolon is mobilized, dissection along the same anatomic plane between the mesentery and retroperitoneum is continued toward the pelvic inlet where the total mesorectal excision (TME) is initiated.
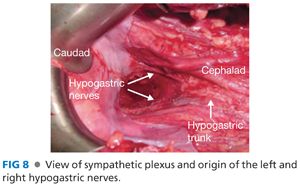
■ The mesorectum is fully mobilized posteriorly using sharp dissection, typically with electrocautery. Care is taken not to injure the left and right hypogastric nerves posteriorly, as they can be intimately associated with the mesorectum (FIG 8).
■ Dissection along the presacral plane is facilitated with anterior traction on the mesorectum provided by the St. Mark’s retractors (FIG 9A,B).
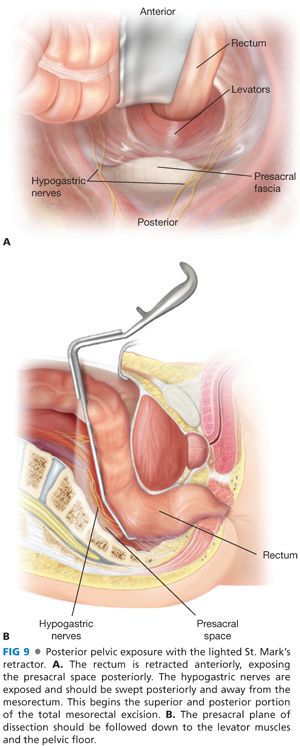
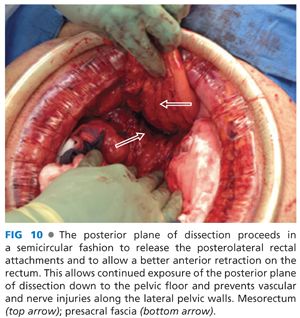
■ As the dissection proceeds posteriorly, the curve of the sacrum and coccyx needs to be followed (FIG 10), as inadvertent injury to the venous plexus of the sacrum posteriorly and hypogastric veins laterally can result that can be very difficult to control. Division of the rectosacral facia exposes the pelvic floor (levator ani).
■ Once the rectum is fully mobilized posteriorly, the lateral mobilization can commence. This phase of the dissection is facilitated by the St. Mark’s retractors, and the dissection proceeds along the avascular mesorectal plane that was initiated posteriorly. The lateral rectal ligaments are transected with an energy device (FIG 11).

■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








