- Type I: self-limiting, resolution expected within 4 weeks
- Type II: medium term, resolves within weeks to months but before the need for home parenteral nutrition (HPN)
- Type III: irreversible/long term, usually requires HPN
Important features in the history
- Family history
- Duration of symptoms
- Degree of weight loss
- Evidence of dehydration
- Recurrent infections/evidence of immune system defects
Baseline investigations
- Nutritional bloods, including:
- U&E, calcium, magnesium and phosphate
- LFTs
- FBC and coagulation: fat soluble vitamin
- B vitamins, folate and ferritin, triglycerides
- U&E, calcium, magnesium and phosphate
- Strict fluid balance: record stools, vomiting and other losses, e.g. chest drain
- May need brief urinary catheterisation to assess urine output accurately if very watery diarrhoea
- Anthropometry, including head circumference <1-year old
- Urinary electrolytes: to determine adequate sodium input
General management and adaptation
PN should be started when there the gut is unable to provide nutrition for a period of at least a week, or even shorter where there is already significant malnutrition. It should not be used where sufficient nutrition can be given enterally or where the period of non-feeding is likely to be only a few days.
Consider refeeding syndrome if significant weight loss (see Chapter 42).
Trophic feeding
Enterocytes require enteral nutrition for optimal growth and health, so even small amounts of feed given continuously will be beneficial. In young infants this can be as little as 1 mL/hour and around 5 mL/hour in an older child.
- Slow introduction of continuous enteral feeding, progressing to introduction of small oral boluses
- Proton pump inhibitors decrease volume of gastric secretions
- Consider jejunal feeding if foregut dysmotility
- Antimotility agents such as loperamide for diarrhoea (if colon present)
- Cycled enteral antibiotics for bacterial overgrowth
When to refer to nutrition support team (NST)
All children with type II intestinal failure require multidisciplinary input from the NST for ongoing support and planning for home PN if necessary. Once it is recognised that a child is likely to have a long-term PN requirement for permanent intestinal failure or severe short bowel syndrome, referral should not be delayed.
The NST also provides support in the nutritional management of any child with complex nutritional needs, especially where there are complicating factors such as fluid balance and difficulty establishing enteral or oral feeding.
Short bowel syndrome (SBS)
Normal bowel length varies with age and increases maximally over the first year of life (Table 44.1). SBS in children is most common in infancy and is defined as a bowel length of <80 cm, with very short bowel defined as <40 cm and extreme as <15 cm.
Table 44.1 Normal bowel lengths at different ages
| Age | Bowel length (ligament of Treitz to ileo-caecal valve) |
|---|---|
| Premature infant | Correlates to gestational age and doubles in length from 28 weeks to term |
| Term infant | 240 cm |
| 15 years old | 430 cm |
| Adult | 600–2000cm |
Important features from history
- Length of remaining bowel: <40 cm is likely to require HPN
- Calibre and motility of remaining bowel
- Part of bowel remaining: ileum more likely to adapt than jejunum; colon is important for water reabsorption and nutrient production from short chain fatty acids
- If the ileo-caecal valve has been removed, there is increased risk of bacterial overgrowth
Management and adaptation (Algorithm 44.1 and Table 44.2)
Adaptation is the process by which intestinal hypertrophy and hyperplasia allows increased nutrient and water absorption.
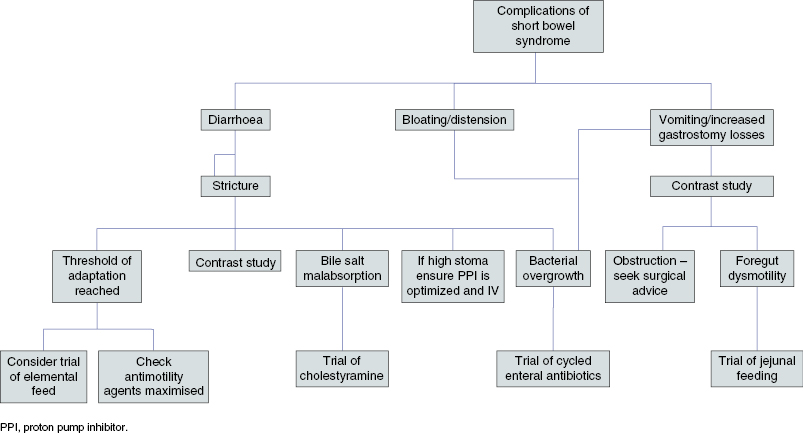
Table 44.2 Conditions giving rise to short bowel syndrome and management
| Diagnosis | Aetiology | Particular complications |
|---|---|---|
| Necrotising enterocolitis (NEC) | Premature babies (especially <1500 g) Gram-negative sepsis Hypoxia Altered intestinal blood flow | Total gut ischaemia |
| Cardiac NEC | Seen after bypass for cardiac surgery | Protein-losing enteropathy, e.g. after Fontan |
| Gastroschisis | ? Association with recreational drug use | Often poorer outcome, especially if other anomalies present Dilated and dysmotile bowel |
| Neonatal volvulus/atresias | Some genetic cases of malrotation, including FOXF1 transcription factor mutations There are also four syndromes featuring malrotation | Motility often disordered Perforation of bowel in utero with meconium peritonitis and/or hydrops fetalis |
| Congenital short bowel | Unknown; very rare Some cases familial May be associated with other anomalies | Usually associated with malrotation |
| Meconium ileus (MI)/Distal Intestinal Obstruction Syndrome (DIOS) | Often associated with cystic fibrosis Simple or complex, i.e. associated with atresia, perforation, etc. |






