CT scans can detect solid lesions greater than 1 cm in diameter due to primary or secondary malignant tumour. They usually have a lower attenuation value than normal liver which remains during enhancement. Calcification is present in some metastases such as from colon (especially mucinous primary ones and after chemotherapy). Hepatocellular carcinoma is hyperattenuating on arterial phase and hypoattenuating (washout) on portal venous phase when compared to the surrounding liver. However, detection of small hepatocellular carcinomas in a multinodular cirrhotic liver on CT is not as sensitive as MRI. Injection of iodized oil (lipiodol) into the hepatic artery followed by unenhanced CT 2 weeks later may be used to detect small lesions but has been abandoned due to improved CT and MRI imaging.
Abscesses usually show a lower attenuation than normal liver. Aspiration/ drainage under CT guidance is possible as with ultrasound. Hydatid cysts, particularly those that are old and inactive, may have a calcified rim. Daughter cysts can be seen in active disease [18].
Enhanced CT is a valuable aid in abdominal trauma The size of any laceration or contusion can be seen, and the severity and extent of a haemoperitoneum evaluated. False aneurysms of the hepatic artery should be searched for.
An important function of CT, more so than ultrasound, is to define the anatomy for the surgeon considering hepatic resection or transplantation [19]. The segmental position of the lesion and its relationship to vessels can be identified accurately.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) uses forcible alignment of hydrogen protons in a strong magnetic field, followed by short pulses of radiofrequency energy to deflect the protons. The subsequent release of energy as the protons realign is detected by receiver coils and used to create the image. The technique is safe with certain exceptions. Patients with cardiac pacemakers and internal magnetic material (clips, metallic foreign bodies) should not undergo MRI. Pregnancy is a relative contraindication and should be avoided, particularly in the first trimester. In addition, it is difficult to scan and monitor the ventilated patient.
Several types of measurement of tissue can be made, but those most commonly employed are the T1 and T2 relaxation times. The T1 relaxation time is the time taken for hydrogen protons to realign within the external magnetic field after a radiofrequency pulse. The T2 relaxation time describes the rate at which the axes of the protons move out of phase with each other because of the differing electromagnetic influence of adjacent protons. Tissues respond differently to the MRI process and scans can therefore characterize fluid, subacute and chronic haematoma, fat (Fig. 33.2), and vessels. Heavily T2-weighted scans can be used to visualize the bile and pancreatic ducts without the need for contrast material; this is magnetic resonance cholangiopancreatography (MRCP).
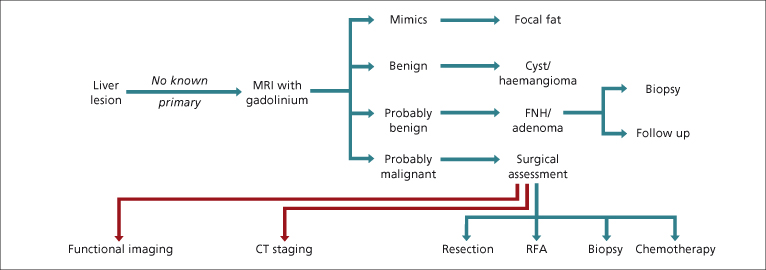
Fig. 33.2. Algorithm 2: the possible outcomes following an MRI scan of a focal liver lesion. FNH, focal nodular hyperplasia; RFA, radiofrequency ablation.
On T1-weighted scans the normal liver appears grey and homogeneous, with a signal greater than the spleen. On T2-weighted scans the hepatic signal is less than that from spleen. Normal blood vessels usually appear black with T1-weighted scans because the energy emanated during the radiofrequency pulse has passed out of the slice with blood flow by the time the return signal is recorded.
Although vessels and focal abnormalities can be identified on non-enhanced images, accurate assessment of the liver vasculature and characterization of defined lesions requires the use of contrast agents. There are three main categories used in liver imaging [20]:
- extracellular fluid agents
- hepatobiliary-specific agents
- reticuloendothelial agents.
The extracellular agents are the most commonly used and are composed of gadolinium chelated onto an organic compound. They predominantly act by shortening the T1 relaxation times, resulting in increased signal on T1-weighted images. They rely mainly on differential blood flow for lesion detection/ characterization and are considered safe at the low doses used for MRI scanning. At high doses they are nephrotoxic and there is a small risk of nephrogenic systemic fibrosis in patients with severe renal impairment [21].
The hepatobiliary-specific agents are also based on gadolinium (a previous manganese based compound is no longer available) and in the initial phase of imaging have similar properties to the extracellular agents. Subsequent uptake by hepatocytes allows for delayed imaging, which does not have to be precisely timed, offering potential advantages over the extracellular agents. Varying degrees of biliary excretion also allow delayed imaging of the bile ducts.
One of the specific benefits of these agents is the ability to distinguish between the two benign hepatocellular lesions; focal nodular hyperplasia and adenoma (Figs 33.3, 33.4). Focal nodular hyperplasia maintains its enhancement on the delayed images, whilst adenomas lose signal on the delayed scan [22,23]. This distinction can be much more difficult with standard enhanced MRI. It is important to realize that it may not be possible to distinguish benign from well-differentiated malignant hepatocellular lesions, even with these agents, as opposed to the pattern of poorly differentiated hepatocellular carcinoma (Fig. 33.5).
Fig. 33.3. Focal fatty sparing. T1-weighted MRI in-phase image (a) and out-of-phase image (b) showing significant signal dropout of the liver on the out-of-phase image, indicating steatosis with relative sparing of segment IV.
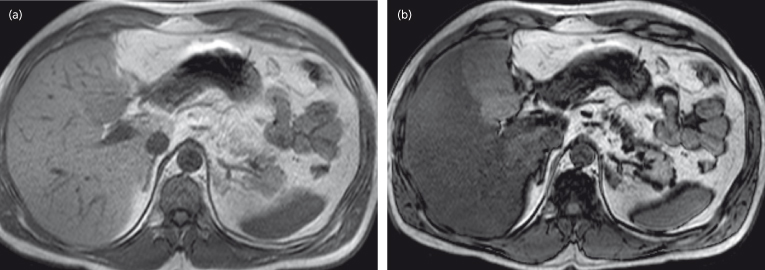
Fig. 33.4. Haemangioma. Portal venous phase CT (a) showing two focal lesions with peripheral enhancement, which on the delayed phase CT (b) demonstrated complete in-filling of the segment VII lesion but incomplete in-filling of the segment VIII, consistent with a haemangioma. MRI images showing a haemangioma which has a lobulated contour and exhibits high signal on T2-weighted imaging (c), intermediate signal on T1-weighted imaging (d), peripheral enhancement on arterial phase (e) and centripedal in-filling on portal venous phase imaging (f).
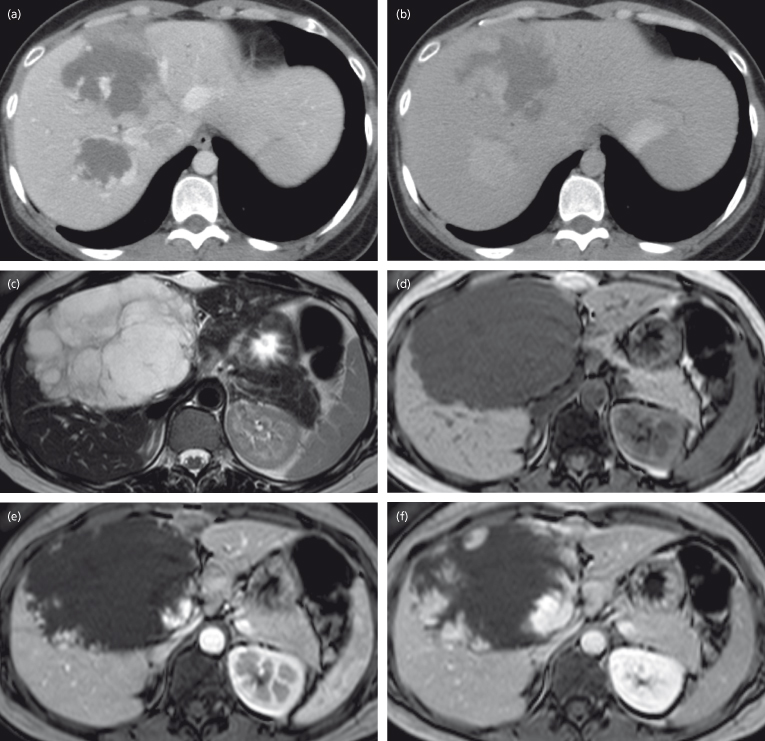
Fig. 33.5. Focal nodular hyperplasia (FNH). MRI images demonstrating a typical FNH in segment VIII of the liver. T2-weighted imaging (a) shows a focal lesion in segment VIII which is of slightly higher signal (hyperintense) compared to surrounding liver with a small higher-signal central scar, but on T1-weighted imaging (b) the lesion is slightly hypointense with a small lower-signal central scar. The lesion exhibits vivid enhancement on the arterial phase (c) with a non-enhancing central scar, becoming isointense on the portal venous phase (d) with enhancement of the central scar on the delayed phase (e).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








