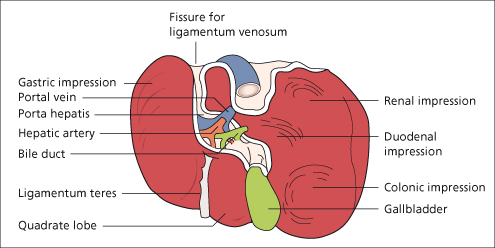
The liver has a double blood supply. The portal vein brings venous blood from the intestines and spleen and the hepatic artery, coming from the coeliac axis, supplies the liver with arterial blood. These vessels enter the liver through a fissure, the porta hepatis, which lies far back on the inferior surface of the right lobe. Inside the porta, the portal vein and hepatic artery divide into branches to the right and left lobes, and the right and left hepatic bile ducts join to form the common hepatic duct. The hepatic nerve plexus contains fibres from the sympathetic ganglia T7–T10, which synapse in the coeliac plexus, the right and left vagi and the right phrenic nerve. It accompanies the hepatic artery and bile ducts into their finest ramifications, even to the portal tracts and hepatic parenchyma [3].
The ligamentum venosum, a slender remnant of the ductus venosus of the fetus, arises from the left branch of the portal vein and fuses with the inferior vena cava at the entrance of the left hepatic vein. The ligamentum teres, a remnant of the umbilical vein of the fetus, runs in the free edge of the falciform ligament from the umbilicus to the inferior border of the liver and joins the left branch of the portal vein. Small veins accompanying it connect the portal vein with veins around the umbilicus. These become prominent when the portal venous system is obstructed inside the liver.
The venous drainage from the liver is into the right and left hepatic veins which emerge from the back of the liver and at once enter the inferior vena cava very near its point of entry into the right atrium.
Lymphatic vessels terminate in small groups of glands around the porta hepatis. Efferent vessels drain into glands around the coeliac axis. Some superficial hepatic lymphatics pass through the diaphragm in the falciform ligament and finally reach the mediastinal glands. Another group accompanies the inferior vena cava into the thorax and ends in a few small glands around the intrathoracic portion of the inferior vena cava.
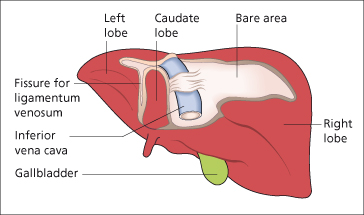
The inferior vena cava makes a deep groove to the right of the caudate lobe about 2 cm from the midline.
The gallbladder lies in a fossa extending from the inferior border of the liver to the right end of the porta hepatis.
The liver is completely covered with peritoneum, except in three places. It comes into direct contact with the diaphragm through the bare area which lies to the right of the fossa for the inferior vena cava. The other areas without peritoneal covering are the fossae for the inferior vena cava and gallbladder.
The liver is kept in position by peritoneal ligaments and by the intra-abdominal pressure transmitted by the tone of the muscles of the abdominal wall.
Functional Liver Anatomy: Sectors and Segments
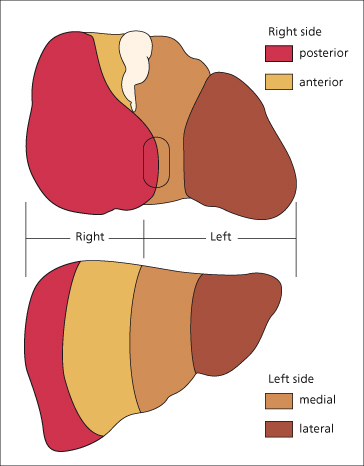
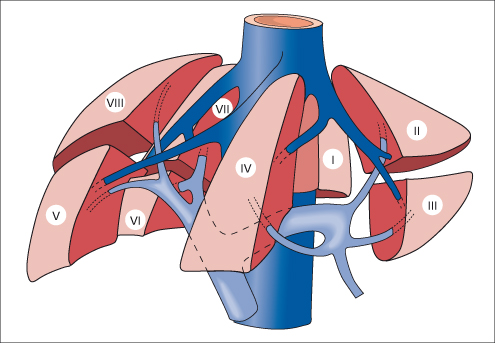
Based on the external appearances described above, the liver has a right and left lobe separated along the line of insertion of the falciform ligament. This separation, however, does not correlate with blood supply or biliary drainage. A functional anatomy is now recognized based upon vascular and biliary anatomy. The Couinaud classification [4] defines eight segments (segments I-IV in the left lobe, V-VIII in the right lobe), while the Bismuth classification [5] divides the liver into four sectors. These can be correlated with results seen with imaging techniques.
The main portal vein divides into right and left branches and each of these supplies two further subunits (variously called sectors). The sectors on the right side are anterior and posterior and, in the left lobe, medial and lateral—giving a total of four sectors (Fig. 1.4). Using this definition, the right and left side of the liver are divided not along the line of the falciform ligament, but along a slightly oblique line to the right of this, drawn from the inferior vena cava above to the gallbladder bed below. The right and left side are independent with regard to portal and arterial blood supply, and bile drainage. Three planes separate the four sectors and contain the three major hepatic vein branches.
Closer analysis of these four hepatic sectors produces a further subdivision into segments (Fig. 1.5). The right anterior sector contains segments V and VIII; right posterior sector, VI and VII; left medial sector, IV; left lateral sector, II and III. There is no vascular anastomosis between the macroscopic vessels of the segments but communications exist at the sinusoidal level. Segment I, the equivalent of the caudate lobe, is separate from the other segments and does not derive blood directly from the major portal branches or drain by any of the three major hepatic veins.
Fig. 1.5. Schematic representation of the functional anatomy of the liver. Three main hepatic veins (dark blue) divide the liver into four sectors, each of them receiving a portal pedicle; hepatic veins and portal veins are intertwined as the fingers of two hands [5].
This functional anatomical classification allows interpretation of radiological data and is of importance to the surgeon planning a liver resection. There are wide variations in portal and hepatic vessel anatomy which can be demonstrated by spiral computed tomography (CT) and magnetic resonance imaging (MRI) reconstruction [6].
Anatomical Abnormalities of the Liver
These are being increasingly diagnosed with more widespread use of CT and ultrasound scanning.
Accessory Lobes.
The livers of the pig, dog and camel are divided into distinct and separate lobes by strands of connective tissue. Occasionally, the human liver may show this reversion and up to 16 lobes have been reported. This abnormality is rare and without clinical significance. The lobes are small and usually on the undersurface of the liver so that they are not detected clinically but are noted incidentally at scanning, operation or necropsy. Rarely they are intrathoracic [7]. An accessory lobe may have its own mesentery containing hepatic artery, portal vein, bile duct and hepatic vein. This may twist and demand surgical intervention.
Ectopic Liver.
Small nodules of normal liver derived from the embryologic hepatic bud may be found in less than 1% of laparoscopies and autopsies near the gallbladder, hepatic ligaments, gastrorenal ligament, omentum, retroperitorneum and thorax. These may give rise to hepatocellular carcinoma [8,9].
Riedel’s Lobe.
This is fairly common and is a downward tongue-like projection of the right lobe of the liver [10]. It is a simple anatomical variation; it is not a true accessory lobe. The condition is more frequent in women. It is detected as a mobile tumour on the right side of the abdomen which descends with the diaphragm on inspiration. It may come down as low as the right iliac region. It is easily mistaken for other tumours in this area, especially a visceroptotic right kidney. It does not cause symptoms and treatment is not required. Rarely, it is a site for metastasis or primary hepatocellular carcinoma. Scanning may be used to identify Riedel’s lobe and other anatomical abnormalities.
Cough Furrows on the Liver.
These are vertical grooves on the convexity of the right lobe. They are one to six in number and run anteroposteriorly, being deeper posteriorly. These represent diaphragmatic sulci and fissures produced by pressure exerted by diaphragmatic muscle on peripheral structurally weak liver parenchymal zones associated with watershed vascular distribution [11]. Chronic cough produces such pressure.
Corset Liver.
This is a horizontal fibrotic furrow or pedicle on the anterior surface of one or both lobes of the liver just below the costal margin [12]. The mechanism is unknown, but it affects elderly women who have worn corsets for many years. It presents as an abdominal mass in front of and below the liver and is isodense with the liver. It may be confused with a hepatic tumour.
Lobar Atrophy.
Interference with the portal supply or biliary drainage of a lobe may cause atrophy. There is usually hypertrophy of the opposite lobe. Left lobe atrophy found at post-mortem or during scanning is not uncommon and is probably related to reduced blood supply via the left branch of the portal vein. The lobe is decreased in size with thickening of the capsule, fibrosis and prominent biliary and vascular markings. The vascular problem may date from the time of birth. Loss of left lobe parenchyma in this instance develops by the process of ischaemic extinction due to impaired flow from the affected large portal vein branch. Replacement fibrosis ensues. This large vessel extinction process should be distinguished from cirrhosis in which the entire liver is affected by numerous intrahepatic and discrete extinction lesions, which affect small hepatic veins and portal vein branches during the course of inflammation and fibrosis. Hence, in cirrhosis the entire liver surface is diffusely converted to regenerative parenchymal nodules surrounded by fibrosis.
Obstruction to the right or left hepatic bile duct by benign stricture or cholangiocarcinoma is now the most common cause of lobar atrophy [13]. The alkaline phosphatase is usually elevated. The bile duct may not be dilated within the atrophied lobe. Relief of obstruction may reverse the changes if cirrhosis has not developed. Distinction between a biliary and portal venous aetiology may be made using technetium-labelled iminodiacetic acid (IDA) and colloid scintiscans. A small lobe with normal uptake of IDA and colloid is compatible with a portal aetiology. Reduced or absent uptake of both isotopes favours biliary disease.
Agenesis of the Right Lobe [14].
This rare lesion may be an incidental finding associated, probably coincidentally, with biliary tract disease and also with other congenital abnormalities. It can cause presinusoidal portal hypertension. The other liver segments undergo compensatory hypertrophy. It must be distinguished from lobar atrophy due to cirrhosis or hilar cholangiocarcinoma.
Situs Inversus (SI).
In the exceedingly rare SI totalis or abdominalis the liver is located in the left hypochondrium and may be associated with other anomalies including biliary atresia, polysplenia syndrome, aberrant hepatic artery anatomy and absent portal vein. Hepatic surgery (partial hepatectomy, liver transplantation) is feasible, but complex. Other conditions associated with displacement of the liver from its location in the right upper quadrant include congenital diaphragmatic hernias, diaphragmatic eventration and omphalocoele.
Anatomical abnormalities of the gallbladder and biliary tract are discussed in Chapter 12.
Anatomy of the Biliary Tract (Fig. 1.6)
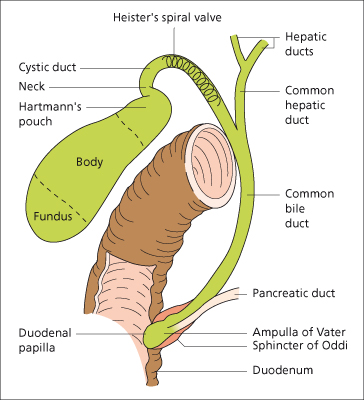
The right and left hepatic ducts emerge from the liver and unite in the porta hepatis to form the common hepatic duct. This is soon joined by the cystic duct from the gallbladder to form the common bile duct.
The common bile duct runs between the layers of the lesser omentum, lying anterior to the portal vein and to the right of the hepatic artery. Passing behind the first part of the duodenum in a groove on the back of the head of the pancreas, it enters the second part of the duodenum. The duct runs obliquely through the posteromedial wall, usually joining the main pancreatic duct to form the ampulla of Vater (c. 1720). The ampulla makes the mucous membrane bulge inwards to form an eminence, the duodenal papilla. In about 10–15% of subjects the bile and pancreatic ducts open separately into the duodenum.
The dimensions of the common bile duct depend on the technique used. At operation it is about 0.5–1.5 cm in diameter. Using ultrasound the values are less, the common bile duct being 2–7 mm, with values greater than 7 mm being regarded as abnormal. Using endoscopic cholangiography, the duct diameter is usually less than 11 mm, although after cholecystectomy it may be more in the absence of obstruction.
The duodenal portion of the common bile duct is surrounded by a thickening of both longitudinal and circular muscle fibres derived from the intestine. This is called the sphincter of Oddi (c. 1887).
The gallbladder is a pear-shaped bag 9 cm long with a capacity of about 50 mL. It always lies above the transverse colon, and is usually next to the duodenal cap overlying, but well anterior to, the right renal shadow. The fundus is the wider end and is directed anteriorly; this is the part palpated when the abdomen is examined. The body extends into a narrow neck which continues into the cystic duct. The valves of Heister are spiral folds of mucous membrane in the wall of the cystic duct and neck of the gallbladder. Hartmann’s pouch is a sacculation at the neck of the gallbladder; this is a common site for a gallstone to lodge.
The mucosa is in delicate, closely woven folds; instead of glands there are indentations of mucosa which usually lie superficial to the muscle layer. Increased intraluminal pressure in chronic cholecystitis results in formation of branched, diverticula-like invaginations of the mucosa which reach into the muscular layer, termed Rokitansky–Aschoff sinuses. There is no submucosa or muscularis mucosae. The gallbladder wall consists of a loose connective tissue lamina propria and muscular layer containing circular, longitudinal and oblique muscle bundles without definite layers, the muscle being particularly well developed in the neck and fundus. The outer layers are the subserosa and serosa. The distensible normal gallbladder fills with bile and bile acids secreted by the liver, concentrates the bile through absorption of water and electrolytes and with meals contracts under the influence of cholecystokinin (acting through preganglionic cholinergic nerves) to empty bile into the duodenum.
Blood Supply.
The gallbladder receives blood from the cystic artery. This branch of the hepatic artery is large, tortuous and variable in its anatomical relationships. Smaller blood vessels enter from the liver through the gallbladder fossa. The venous drainage is into the cystic vein and thence into the portal venous system. Attention to the vascular-biliary anatomy in the reference area known as Calot’s triangle (bordered by the cystic duct, common hepatic duct and lower edge of the liver) reduces the risk of vascular injuries and potential biliary strictures. Most bile duct injuries occur at cholecystectomy (incidence of <1.3% for either open or laparoscopic cholecystectomy). After liver transplantation 10–33% of patients may develop biliary complications, of which biliary stricture is the most important.
The arterial blood supply to the supraduodenal bile duct is generally by two main (axial) vessels which run beside the bile duct. These are supplied predominantly by the retroduodenal artery from below, and the right hepatic artery from above, although many other vessels contribute. This pattern of arterial supply would explain why vascular damage results in bile duct stricturing [15].
Lymphatics.
There are many lymphatic vessels in the submucous and subperitoneal layers. These drain through the cystic gland at the neck of the gallbladder to glands along the common bile duct, where they anastomose with lymphatics from the head of the pancreas.
Nerve Supply.
The gallbladder and bile ducts are liberally supplied with nerves, from both the parasympathetic and the sympathetic system.
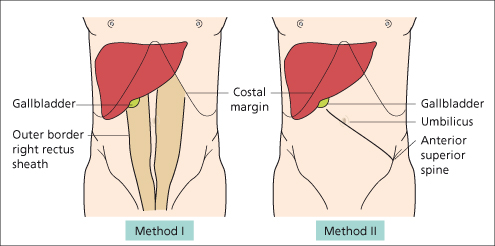
Surface Marking (Figs 1.7, 1.8)
Fig. 1.8. Surface markings of the gallbladder. Method I: the gallbladder is found where the outer border of the right rectus abdominis muscle intersects the 9th costal cartilage. Method II: a line drawn from the left anterior superior iliac spine through the umbilicus intersects the costal margin at the site of the gallbladder.
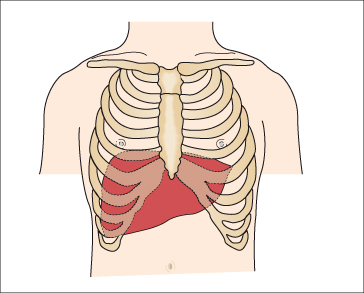
Liver.
The upper border of the right lobe is on a level with the 5th rib at a point 2 cm medial to the right midclavicular line (1 cm below the right nipple). The upper border of the left lobe corresponds to the upper border of the 6th rib at a point in the left midclavicular line (2 cm below the left nipple). Here only the diaphragm separates the liver from the apex of the heart.
The lower border passes obliquely upwards from the 9th right to the 8th left costal cartilage. In the right nipple line it lies between a point just under to 2 cm below the costal margin. It crosses the midline about midway between the base of the xiphoid and the umbilicus and the left lobe extends only 5 cm to the left of the sternum.
Gallbladder.
Usually the fundus lies at the outer border of the right rectus abdominis muscle at its junction with the right costal margin (9th costal cartilage) (Fig. 1.8). In an obese subject it may be difficult to identify the outer border of the rectus sheath and the gallbladder may then be located by the Grey–Turner method. A line is drawn from the left anterior superior iliac spine through the umbilicus; its intersection with the right costal margin indicates the position of the gallbladder. These guidelines depend upon the individual’s build. The fundus may occasionally be found below the iliac crest.
Methods of Examination
Liver.
The lower edge should be determined by palpation just lateral to the right rectus muscle. This avoids mistaking the upper intersection of the rectus sheath for the liver edge.
The liver edge moves 1–3 cm downwards with deep inspiration. It is usually palpable in normal subjects inspiring deeply. The edge may be tender, regular or irregular, firm or soft, thickened or sharp. The lower edge may be displaced downwards by a low diaphragm, for instance in emphysema. Movements may be particularly great in athletes or singers. Some patients with practice become very efficient at ‘pushing down’ the liver. The normal spleen can become palpable in similar fashion. Common causes of a liver palpable below the umbilicus are malignant deposits, polycystic or Hodgkin’s disease, amyloidosis, congestive cardiac failure and gross fatty change. Rapid change in liver size may occur when congestive cardiac failure is corrected, cholestatic jaundice relieved, or when severe diabetes is controlled. The surface can be palpated in the epigastrium and any irregularity or tenderness noted. An enlarged caudate lobe, as in the Budd–Chiari syndrome or with some cases of cirrhosis, may be palpated as an epigastric mass.
Pulsation of the liver, usually associated with tricuspid valvular incompetence, is felt by manual palpation with one hand behind the right lower ribs posteriorly and the other anteriorly on the abdominal wall.
The upper edge is determined by fairly heavy percussion passing downwards from the nipple line. The lower edge is recognized by very light percussion passing upwards from the umbilicus towards the costal margin. Percussion is a valuable method of determining liver size and is the only clinical method of determining a small liver.
The anterior liver span is obtained by measuring the vertical distance between the uppermost and lowermost points of hepatic dullness by percussion in the right midclavicular line. This is usually 12–15 cm. Direct percussion is as accurate as ultrasound in estimating liver span [16].
Friction may be palpable and audible, usually due to recent biopsy, tumour or perihepatitis. The venous hum of portal hypertension is audible between the umbilicus and the xiphisternum. An arterial murmur over the liver may indicate a primary liver cancer or acute alcoholic hepatitis.
Gallbladder.
The gallbladder is palpable only when it is distended. It is felt as a pear-shaped cystic mass usually about 7 cm long. In a thin person, the swelling can sometimes be seen through the anterior abdominal wall. It moves downwards on inspiration and is mobile laterally but not downwards. The swelling is dull to percussion and directly impinges on the parietal peritoneum, so that the colon is rarely in front of it. Gallbladder dullness is continuous with that of the liver.
Abdominal tenderness should be noted. Inflammation of the gallbladder causes a positive Murphy’s sign. This is the inability to take a deep breath when the examining fingers are hooked up below the liver edge. The inflamed gallbladder is then driven against the fingers and the pain causes the patient to catch their breath.
The enlarged gallbladder must be distinguished from a visceroptotic right kidney. This, however, is more mobile, can be displaced towards the pelvis and has the resonant colon anteriorly. A regenerative or malignant nodule feels much firmer.
Imaging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree