and Andrea Bischoff1
(1)
Pediatric Surgery, Colorectal Center for Children Cincinnati Children’s Hospital, Cincinnati, OH, USA
Electronic supplementary material
Supplementary material is available in the online version of this chapter at 10.1007/978-3-319-14989-9_11.
11.1 Definition and Frequency
Imperforate anus with a recto-bladder neck fistula is the highest of all anorectal malformations seen in male patients. The rectum connects to the bladder neck (Fig. 11.1). It is relatively common to see that these patients have a rather narrow pelvic space. We interpret this like a manifestation of a significant degree of caudal regression (Animation 11.1). The sacrum may be normal, but frequently, it is very abnormal or even absent. The frequency of associated defects is much higher than in all the other malformations. Fortunately, in our experience, this defect only occurs in approximately 10 % of all anorectal malformation patients in males [1]. Unfortunately, this defect runs with the worst functional prognosis for bowel control and occasionally for urinary control. In our experience, this particular defect is the only one that requires a laparotomy or laparoscopy in order to be repaired. In other words, the rectum is located so high in the pelvis and connected to the bladder neck (very high in the urinary tract) that it is not possible to be reached posterior sagittally.
Fig. 11.1
Diagram showing a bladder neck fistula
In fact, some of the worst unfortunate catastrophes that we have seen occurred in babies that were born with this defect and a surgeon tried to reach the rectum posterior sagittally; he obviously could not find it, but in the process, he damaged the vas deferens, seminal vesicles, and/or prostate. In some cases, the surgeons divided the entire urethra or the bladder neck and pulled down a megaureter or even the entire bladder thinking that they were dealing with the rectum. These catastrophic events occurred only in patients that were operated on without a preoperative high-pressure distal colostogram (Animation 11.2).
11.2 Associated Defects
11.2.1 Sacral Defects
The average sacral ratio in patients with recto-bladder neck fistula is AP 0.51 and lateral 0.6 (normal AP is 0.74 and lateral 0.76). It is not uncommon to find these patients to have, in addition, sacral hemivertebrae in approximately 35 % of the cases.
11.2.2 Spinal-Associated Defects
Fifteen percent of these patients have suffered from hemivertebra, which produces scoliosis of different degrees in magnitude. The most frequent location of the hemivertebra is the lumbar spine, followed in frequency by the thoracic spine.
11.2.3 Urologic-Associated Defects
As expected, the incidence of associated urologic defects is the highest in these particular types of patients. In a recent evaluation of 110 patients operated on by us with recto-bladder neck fistula, 99 (89 %) of them suffered from some sort of urologic malformation or vesicoureteral reflux. The frequency of absent kidney in these patients is 37/111 (33 %). Vesicoureteral reflux was present in 40 patients (36 %). Eighteen percent of them suffer from hypospadias. Thirty patients (26 %) suffered from an undescended testicle. Eighteen percent of them have a bifid scrotum. Two patients have penile-scrotal transposition. Thirty-three patients (29 %) were born with hydronephrosis. In addition, there is a specific group of patients born with recto-bladder neck fistula that have a single kidney with hydronephrosis, megaureter, and massive reflux. This is a very bad situation because usually they have poor sacrum and therefore poor prognosis for bowel and urinary control. In addition, the fact that the patients are born with a single kidney with hydronephrosis indicates that they already have a significant degree of kidney damage and there is a high chance that these patients will end up with a kidney transplant when they grow up.
Table 11.1 shows the list of urologic abnormalities.
Table 11.1
List of urologic abnormalities in patients with bladder neck fistula
Anomaly | No. (%) |
|---|---|
VUR | 36 |
Absent kidney | 33 |
Hydronephrosis | 29 |
Undescended testis | 26 |
Bifid scrotum | 18 |
Hypospadias | 18 |
Intravesical verumontanum | 45 |
Urethral stenosis | 13 |
Neurogenic bladder (congenital) | 11 |
Megaureter | 9 |
Other | 24 |
Ectopic ureters were present in ten cases (9 %). The ectopia occurs most commonly toward the bladder neck and occasionally in the posterior urethra. This last group of ureters connected to the posterior urethra usually originates from completely damaged kidneys (Fig. 11.2).
Fig. 11.2
Diagram showing a case of bladder neck fistulas with an ectopic ureter
A serious, not previously known anomaly found in 45 % (15 cases) of those patients in whom we performed a cystoscopy was an ectopic verumontanum. Six of them were located in the trigone (Fig. 11.3), five in the bladder neck, and four immediately below the bladder neck. Based on this experience, we now consider it mandatory to do a cystoscopy on these patients to avoid unpleasant future surprises for the patient and the family. When these patients reach adolescence, they have erections and orgasms but they ejaculate into the bladder. Theoretically for these patients to have children, it will require special maneuvers to retrieve the sperm from the urine followed by artificial insemination.
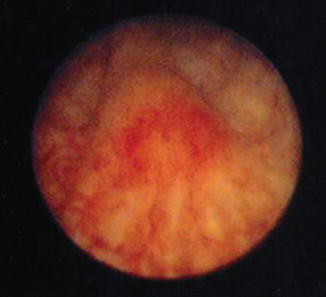
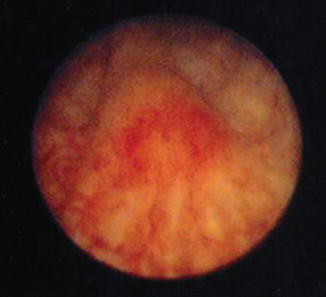
Fig. 11.3
Cystoscopic aspect of a verumontanum located at the trigone
When the clinician makes the diagnosis of the recto-bladder neck fistula type of malformation, he/she should be aware of the fact that he/she is dealing with a patient with a potential serious urologic condition.
11.2.4 Gastrointestinal-Associated Defects
The incidence of esophageal atresia is 15 %, Meckel’s diverticulum 2 %, and abdominal wall defects 4 %.
11.2.5 Neurosurgical-Associated Defects
The incidence of tethered cord in these patients is 32 %. In addition, 5 % of the patients suffer from other neurosurgical conditions, including a lipoma and blunted conus.
11.2.6 Cardiovascular-Associated Defects
Fifteen percent of these patients are born with an atrial septal defect and 10 % with a patent ductus arteriosus, 5 % with tetralogy of Fallot, 2 % with tricuspid atresia, and 2 % with pentalogy of Fallot.
11.2.7 Other Associated Defects
Five percent of these patients suffer from hand abnormalities and 5 % from lower extremity abnormalities (equinovarus).
11.3 Diagnosis
We must suspect the presence of these very complex malformations when we see a newborn baby with imperforate anus and flat bottom. The midline groove in between the buttocks that we see in normal children is not present. In addition, we frequently see in these patients a sphincter mechanism located right at the base of the scrotum (Fig. 11.4). The presence of a bifid scrotum (Fig. 11.5) also suggests that the malformation that the baby has is rather complex, most likely very high (recto-bladder neck fistula). The diagnosis is confirmed with a distal colostogram and subsequently by cystoscopy that is performed at the time of the main repair. The distal colostogram can be performed after the colostomy is opened (Fig. 11.6).
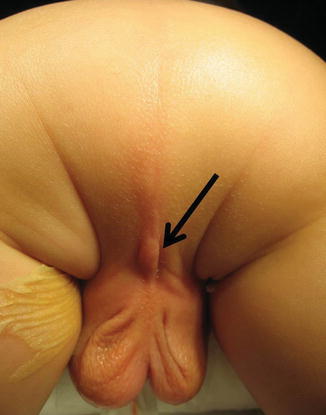


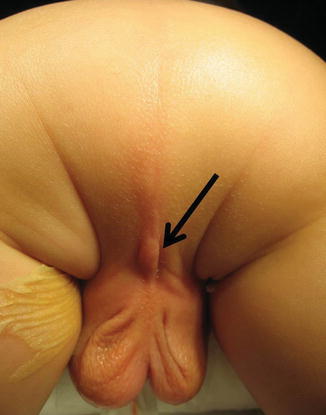
Fig. 11.4
Sphincter located next to the scrotum, frequently seen in cases of bladder neck fistula. Arrow showing the center of the sphincter

Fig. 11.5
Bifid scrotum, frequently seen in bladder neck fistula

Fig. 11.6
Distal colostogram showing a bladder neck fistula
11.4 Treatment
11.4.1 Colostomy
The type of colostomy that we recommend for patients with recto-bladder neck fistula is the same one recommended for the other types of anorectal malformations. However, emphasis must be placed on being sure that enough length of distal colon is left beyond the mucous fistula (distal stoma) (Fig. 11.7), in order to have enough length of bowel for the pull-through without interference by the colostomy (Fig. 11.8). The fact that these patients have the highest of all defects means that the surgeon will need more length of bowel for the pull-through. Unfortunately, in this particular type of defect is where we have seen more often the most common type of error in making a colostomy (making the stoma too distal in the bowel), leaving a very short piece of bowel for the pull-through (Fig. 11.8).


Fig. 11.7
Distal colostogram showing a good length of bowel left distal to the colostomy
Fig. 11.8
Distal colostogram showing a very short piece of bowel distal to the colostomy (insufficient length for a pull-through). (a) Diagram. (b) Image
11.4.2 Main Repair
We perform these operations as soon as we see that the baby is growing and developing normally. If the baby happened to be full term, had a good colostomy, and did not have important associated defects that interfered with his growth and development, then the patient can be operated, at our institution, within a month after the baby is born. However, as we previously mentioned, many of these patients come to our institution when they are much older, and that is why we have experience with the main repair at different ages. These patients should never be approached surgically without a good-quality, high-pressure distal colostogram that shows how much bowel is available distal to the stoma as well as the exact location of the fistula.
If we are dealing with a patient that has a very short piece of bowel distal to the stoma, there is a reason to believe that we will not have enough bowel for the pull-through and that we may have to mobilize the proximal stoma. This is extremely important because knowing this in advance will allow us to plan an adequate procedure. More specifically, we have to prepare the entire gastrointestinal tract (administration of GoLYTELY; see Chap. 7). On the other hand, if the distal colostogram shows that we have enough distal bowel from the mucous fistula, then we are certain that we will not be disturbing the proximal stoma, and all that the patient needs is irrigation of the distal stoma in preparation for the main repair.
The fact that the patient has a recto-bladder neck fistula means that we have to go into the abdomen either by laparotomy, laparoscopy, or both, in addition to the posterior sagittal approach. We start the operation by putting the patient in the lithotomy position and performing a cystoscopy. The cystoscopy is extremely valuable. We have been learning a great deal about the anatomy of the male urethra, bladder neck, and trigone in these patients. As previously mentioned, it is not uncommon to find that these patients have no verumontanum located in the posterior urethra. Rather than that, we find the verumontanum located in the trigone. In retrospect, now we have an explanation for the adult patients that were born with these kinds of defects and have no ejaculation. Further studies demonstrate that they actually ejaculate in the bladder. This must be differentiated from the concept of retrograde ejaculation. We are referring to a patient that has the verumontanum located in the trigone and ejaculates directly into the bladder. This is demonstrated later in life, by finding sperm in the urine after an ejaculation, as well as the cystoscopy (Fig. 11.3). It is not unusual in this type of patients to find, also, ectopic ureters. We have learned that the higher the malformation, the more chances of the patient to have ectopic ureters. The ectopia in this type of defect usually means that the ureters are located closer to the bladder neck or even below the bladder neck into the posterior urethra. Sometimes, the ureters open in the bladder neck and provoke either vesicoureteral reflux, ureterovesical obstruction, or urinary incontinence. When the ureter is ectopic and located into the posterior urethra, usually it is associated with a severe stricture, megaureter, and severe renal damage (Fig. 11.2). It is common for these patients to end up with a nephrectomy. The location of the fistula is frequently visualized at the bladder neck with the cystoscope. A Foley catheter is placed in the bladder.
11.4.3 Laparotomy
A total body preparation is performed on these patients (Fig. 11.9). This means to wash, prep, and drape both lower extremities, the perineum, buttocks, perianal area, lower abdomen, and lumbar portion; in other words, the entire lower body is included in the sterile field. The cautery plate is placed in the back of the patient and is protected with a plastic drape. The arms of the patient are placed in the upward position because they belong to the nonsterile part of the field. Both legs of the patient are covered with stockinettes or with an elastic bandage to avoid loss of temperature. The proximal stoma of the colostomy is packed with packing gauze impregnated with an antiseptic solution to avoid contamination. The skin of the abdominal wall is covered with a plastic drape.
Fig. 11.9
Total body preparation – diagram. (a) Supine. (b) Legs up. (c) Sequence of photographs of bowel preparation. (a) Holding legs up. (b) Cautery plate up in the back. (c) Packing gauze in proximal stoma. (d) Wash and prep the entire body below the chest. (e) Wash and prep the back. (f–h) Sterile sheets on table. (i, j) Covering stomas (k) Foley catheter inserted
We can start the operation either from below or through the abdomen. We more often now approach the abdomen first which can be done by laparotomy or laparoscopy. We consider this particular defect to be a good indication for a laparoscopic approach. More information related with the indications for laparoscopy in anorectal malformations can be found in Chap. 13. The abdomen is entered through a midline incision running from the umbilicus down to the pubis. A needle-tip cautery is used changing from cutting to coagulation to provide meticulous hemostasis. The peritoneal cavity is entered. The urachal remnant and obliterated umbilical arteries are identified and divided. A clamp is placed on the urachal remnant of the bladder to apply caudal traction. The lateral avascular attachments of the bladder to the abdominal wall are divided with cautery to have easy access to the lower pelvis. By pulling on the bladder out of the abdomen and toward the pubis, caudally, we can see the posterior wall of the bladder as well as the peritoneal floor, sigmoid, both vas deferens, and ureters (Fig. 11.10). Both vas deferens seen behind the bladder run distally toward the bladder neck; the ureters are seen retroperitoneally, and they also seem to be running toward the bladder neck. Our specific recommendation is to place a 4-0 silk stitch on the anterior wall of the sigmoid to apply traction. About 1 or 2 cm from the peritoneal floor, the serosa of the anterior wall of the sigmoid is divided in order to create a plane of dissection as close as possible to the bowel wall, but without damaging it. This plane of dissection is followed all around the bowel, separating the mesenteric fat from the sigmoid. Once we have created a plane all around the bowel, a Silastic vessel loop is passed around the rectum in order to have a more effective handle for traction (Fig. 11.11a). Applying traction on the vessel loop, it is very easy to continue a circumferential dissection of the bowel distally. Very soon, within a centimeter or two from our initial dissection, one can appreciate that the bowel decreases in size and becomes very narrow, indicating that it is reaching the bladder neck. One does not have to be very precise in trying to determine exactly the location of the end of the fistula and the beginning of the urinary tract. Once the rectum starts being narrow, it reaches a point where the diameter is about 3–4 mm, obviously not useful for the reconstruction of an anus, and, therefore, that means that we can divide the rectum right there. We must keep in mind that because we are applying traction on the bowel, there is a possibility that we are kinking the bladder neck or the upper posterior urethra, and therefore, when we divide the fistula, actually, we will be dividing the bladder neck or the posterior urethra. Therefore, the traction must be gentle. Two 5-0 Vicryl stitches are placed in both sides of the fistula site in order to avoid retraction, and the fistula is divided. The distal end of the rectum is also sutured with a running 5-0 Vicryl to avoid contamination from mucus or meconium previously left in the bowel. The fistula is closed with three to five 5-0 Vicryl sutures (Animation 11.3) (Fig. 11.11b).