CHAPTER 1 Zenker’s diverticulum
Step 1. Surgical anatomy
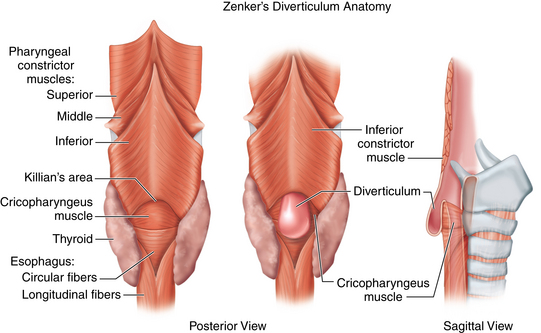
♦ Zenker’s diverticulum is a pulsion diverticulum that occurs between the lowermost fibers of the inferior pharyngeal constrictor and the cricopharyngeal (CP) segment. This segment is the upper esophageal sphincter (UES) and is composed of the cricopharyngeus muscle and a portion of the upper esophagus musculature (Figure 1-1).
♦ The etiology of Zenker’s diverticulum is a failure of timely opening of the CP segment. The diverticular sac forms in a relative weak spot in the posterior pharyngeal wall as contraction of the tongue and pharyngeal musculature builds pressure above a closed CP segment. Therefore, surgical correction of the condition must address not only the diverticulum but also the hypertonic or stenotic CP segment by performing a thorough myotomy.
♦ The transoral approach provides easy access to the diverticular sac and the CP segment (which lies within the common wall between the diverticulum and the cervical esophagus). However, the access to the segment is limited by the size of the diverticulum. Therefore, it is paradoxically easier to perform an adequate operation on patients with large diverticula as these may be stapled. Diverticula smaller than 2.5 cm may be inadequately divided by stapling because of limitations of the device and inadequate access to the CP segment. However, these smaller diverticula may be treated endoscopically with a CO2 laser in similar fashion.
♦ The availability of endostapling devices has decreased the concern of postoperative salivary leakage to a minimum. Improvements in laser technology allow this laser division to be performed safely without hemorrhage or stenosis.
Step 2. Preoperative considerations
Patient preparation
♦ Patients with Zenker’s diverticulum need a complete head and neck examination to identify other anatomic or neurologic causes for dysphagia. The input of a speech-language pathologist trained in dysphagia is extremely helpful. Many of these patients are elderly and may have more than one reason for their dysphagia. The symptom of dysphagia may not improve after repair of the Zenker’s diverticulum if other contributing causes are not identified preoperatively; in rare cases (listed later), symptoms may actually worsen.
Imaging
Modified barium swallow may identify pharyngeal dysphagia not seen in simple esophagram. Whichever study is performed, evaluation of bolus transit through the esophagus and lower esophageal sphincter (LES) is critical to rule out other disease processes that will not improve with surgery. When a straightforward diverticulum is seen, then the endoscopic diverticulectomy may be considered (Figure 1-2).
♦ The imaging study may identify other causes of dysphagia such as the following:
♦ Other findings on imaging studies must be ruled out to prevent intractable reflux following division of the UES:
Anesthesia
♦ General anesthetic is used with the patient orally intubated. If performing laser division, a reflective, laser-safe endotracheal tube should be used. Oxygen concentration should be maintained below 30% and diluted with helium.
♦ Prophylactic antibiotics that cover oral flora are given in the event that perforation of the sac occurs or there is a need to convert to open repair. We use ampicillin/sulbactam (3 gms intravenously) or clindamycin (600 mg intravenously) for the patient who is allergic to penicillins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree