CHAPTER 6 Gastric wedge resection
Step 1. Clinical anatomy
♦ Gastric wedge resections may be performed for gastric tumors such as early gastric adenocarcinoma (lesions <25 mm in size), gastrointestinal stromal tumors, or other gastric tumors.
♦ Wedge resections to establish a diagnosis may be indicated if other less invasive diagnostic modalities have been unsuccessful.
♦ Wedge resections may also be performed for palliation of symptoms such as tumor hemorrhage for otherwise advanced, unresectable gastric neoplasms (for instance, in patients with distant metastatic disease).
♦ Tumors located at the GE junction or along the pyloric channel may not be appropriate for wedge resection because of the risk of luminal narrowing and may be more appropriately treated with conventional open or laparoscopic anatomic resections.
♦ Tumors along the lesser curvature may involve one or both vagus nerves. If both nerves are divided as part of the resection to achieve oncologically appropriate margins, pyloromyotomy or pyloroplasty may be required.
Step 2. Preoperative considerations
♦ The indications and contraindications for laparoscopic gastric wedge resections are similar to those for any open gastric resection.
♦ Patients who have had significant upper abdominal surgery with resulting dense adhesions may not be candidates for a laparoscopic approach, although a diagnostic laparoscopy may be performed at the beginning of the procedure to determine the feasibility of such an approach.
Patient preparation
♦ Gastric tumors appropriate for wedge resection are generally identified either endoscopically or radiographically during workup of nonspecific upper abdominal symptoms, gastroesophageal reflux, obstruction/early satiety, pain, or gastrointestinal hemorrhage.
♦ On upper endoscopy, tumors generally amenable to a laparoscopic wedge resection are submucosal lesions with an intact mucosal layer. Those that appear mucosal-based or ulcerated may not be appropriate for a wedge resection based on histologic diagnosis, and the planned approach should be reevaluated.
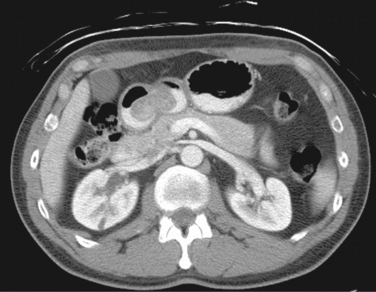
♦ On radiographic imaging, such as computed tomography (CT), tumors may appear as well-encapsulated or infiltrative lesions within the gastric wall or as exophytic lesions protruding intra- or extraluminally (Figure 6-1). Presence of extensive lymphadenopathy may suggest either lymphoma or gastric adenocarcinoma, necessitating a change in treatment.
♦ Additional imaging and laboratory studies for cancer staging may be ordered based on confirmed or suspected diagnosis.
♦ Endoscopic or image-guided fine-needle aspiration or core needle biopsy is indicated if the differential diagnosis would significantly change management. For instance, lymphoma would be treated with nonoperative, medical management, whereas gastric adenocarcinoma would require a more extensive gastric resection plus lymphadenectomy. Although resection for a gastric adenocarcinoma may also be performed laparoscopically, the resection involves removing more gastric tissue, and the procedure should be planned appropriately preoperatively.
♦ Some surgeons tattoo the lesion preoperatively, to assist in localization.
Equipment and instrumentation
♦ Standard laparoscopic instruments may be used for gastric wedge resections:
 Harmonic scalpel (Ethicon, Somerville, New Jersey) or LigaSure (ValleyLab) for omental dissection, division of short gastric vessels, and adhesiolysis
Harmonic scalpel (Ethicon, Somerville, New Jersey) or LigaSure (ValleyLab) for omental dissection, division of short gastric vessels, and adhesiolysis♦ Intraoperative esophagogastroduodenoscopy may be helpful to localize the lesion, particularly for submucosal lesions, which may not be readily visible laparoscopically.
Anesthesia
♦ Procedures are performed under general anesthesia with muscle relaxant.
♦ Epidural anesthesia is not usually required.
♦ Topical anesthetic agents, such as 0.25% bupivacaine hydrochloride, may be infiltrated at each trocar site.
♦ At induction, intravenous antibiotics (generally a cephalosporin) are administered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree