Colonoscopy is the best imaging device currently available for the detection of lesions in the large bowel, but may be an imperfect tool against colon cancer. Because recent guidelines for colorectal cancer screening and surveillance depend on whether polyps are found on colonoscopy and on their size, the need to identify all the neoplasia in the colon has assumed greater importance. This article reviews and assesses the latest developments in colonoscopy including wide-angle optics, endoscope caps and hoods, retroflexion and the use of the third eye retroscope.
Colonoscopy has long been considered the gold standard for evaluation of the colon, as not only can it locate and find lesions throughout the large intestine, but therapy is also possible during the procedure. Unfortunately, time has shown that colonoscopy may be a flawed gold standard, as lesions may be missed and carcinomas may not be prevented. In an editorial, Dr David Lieberman stated that “the data on colonoscopy accuracy is a humble reminder of the limitations of colonoscopy.” Despite the known diagnostic accuracy of colonoscopy, this examination may miss some colonic lesions.
Colonoscopy became popular soon after it was introduced because it was a considerably better tool than barium for colonic evaluation. However, early in the infancy of this combined diagnostic and therapeutic procedure, investigators questioned the accuracy of this gold standard. It was decided that the best way to test the accuracy of colonoscopy was to have a procedure performed and immediately afterward have a repeat examination by the same or a different endoscopist. Thus the patient would serve as his or her own control and permit the discovery of any lesions missed by the first examiner.
The concept of “tandem colonoscopy” is best suited for evaluation of a discrete lesion such as a polyp because this is a quantifiable object with a defined size, shape, and location in the colon. If seen and removed, biopsied, or photographed, there is no mistake that it is present. During these investigations, the first examiner removes all polyps that are encountered so that all polyps seen by the second endoscopist will represent overlooked lesions. One drawback to tandem colonoscopy is that the interventionists are totally aware that this study is under way and will pay special attention to the intraluminal pathology so as not to miss lesions. Despite the heightened awareness by virtue of participating in a tandem colonoscopy experiment, the 3 trials that specifically evaluated the possible “miss” rate of polyps in the large bowel revealed strikingly large numbers of polyps overlooked by the first examiner using standard colonoscopic equipment.
The first report of back-to-back colonoscopies on the same day and immediately following each other was in 1991. The next report of tandem colonoscopy appeared 6 years later, and the most recent was in 2008. The overall miss rates for adenomas in the earlier studies were 15% to 24%. The large multicenter European study found that the miss rate for all polyps was 28%, for hyperplastic polyps 31%, and for adenomas 21%. However, the miss rate for all polyps equal to or larger than 5 mm was 12% and for adenomas 9%. Among the 14 polyps and 6 adenomas larger than 5 mm missed during the first examination, 5 polyps and 1 adenoma were sessile, and 9 polyps and 5 adenomas were flat. In all, 37 adenomas were overlooked in 286 patients with the median size being 3 mm; however, the range of missed lesions was from 1 to 18 mm. In this European study, 3 advanced adenomas were missed with a size from 15 to 18 mm. The investigators reported that there was a 27% rate of missed adenomas for lesions smaller than 5 mm in diameter, and the miss rate for lesions greater than 5 mm in diameter was 9%. In a previous study of 183 patients having tandem colonoscopy, Rex and colleagues reported a 27% miss rate for polyps smaller than 6 mm in diameter and only 6% for polyps larger than 9 mm. There was no significant difference between in the miss rate of polyps in the right colon (27%) and the left colon (21%). Although a substantial percentage (24%) of adenomas was missed, there was an inverse ratio between the miss rate and the size of the adenoma. In the summary of the report, Rex and colleagues recommended that technology be developed that may overcome the technical limitations of colonoscopy.
Another way of evaluating whether polyps were missed on an initial colonoscopic examination is to repeat the colonoscopy at an interval time, not on the same day as the original procedure. In a retrospective analysis of more than 15,000 colonoscopies, the polyp miss rate was evaluated by comparing findings on repeat colonoscopic examinations at 4 and 12 months after the initial colonoscopic examination. The calculated miss rate for all polyps was 17% and for neoplastic polyps 12%. Retrospective studies such as this are not as elegant as tandem examinations, but the findings are similar: polyps are missed during the initial colonoscopy.
The problem with missed colonoscopic neoplasms is primarily due to their location, being on the proximal aspect of folds; this means that the technique of the examination is critically important in the discovery of colon polyps. It has been shown that not all missed lesions are “hidden” because flat neoplasms can elude detection by the casual or untrained observer, even when they are in the field of view of the straightforward viewing standard colonoscope. Pickhardt and colleagues did a computed tomographic colonography (CTC) evaluation of more than 1200 persons who had same-day CTC and colonoscopy. With segmental unblinding during a colonoscopic examination that followed the CTC, 10% of polyps were found only after they were originally missed by colonoscopy but detected on the original CTC. Of the missed neoplasms found on the second-look colonoscopy after segmental unblinding, 17 were tubular adenomas, 3 were tubulovillous adenomas, and 1 was a small adenocarcinoma (size range 6–17 mm). The majority of these neoplasms were located on the edge or on the proximal aspect of a fold. A more recent article from London on CTC simulation reconstructions using a 90° imaging field of view corroborated a previous report which showed that 23.4% of the colonic surface is not visualized by direct straight end-on examinations. The report by East and colleagues repeated the type of scan by Pickhardt and colleagues but with simulated varying fields of view of 90°, 120°, 140°, and 170° to match the angle of view of some colonoscopes. In addition, a simulated retrograde view was obtained with a 135° field of view, equivalent to retrograde viewing by the third-eye retroscope (TER). In this study, the percentage of visualized colonic surface increased with each increasing angle of view increment. The total number of missed areas was approximately the same for fields of view of 90° to 140°, but decreased when the field of view was 170°. Approximately only 85% of the colonic surface would be visualized using a 140° angle of view, and this increased so that more of the surface would be seen when the examination was repeated using a 170° angle of view comparable to the Olympus 180 series colonoscopes (Olympus Medical Instruments, Tokyo, Japan). The simulated addition of a retrograde viewing auxiliary imaging device led to an almost complete surface visualization, with a tenfold decrease in the area that was missed compared with that obtained using a wide-angle colonoscope with a 170° angle of view. With the simulation of optical colonoscopy by CTC software, using the commonly available 140° angle of view of most colonoscopes, approximately 13% of the colonic surface is unseen. Simulation of a colonoscope with a 170° field of view resulted in an almost 6% reduction in percentage of surface missed. The marked additional mucosal visualization seen in the simulation models with a combination of 140° forward and a 135° reverse view (such as that provided by the TER) may actually be preferred to recently developed optics providing a 360° view (Aer-O-Scope), which has a substantial “fish eye effect.” In this simulation model, there does not seem to be any additional benefit to using a colonoscope with 170° angle of view instead of a 140° instrument when associated with the additional advantage of the TER.
Barthel, in an editorial in Gastrointestinal Endoscopy , mentions that to attempt an increase in the finding of adenomas, there have been several articles written on the use of a wide-angle lens on a colonoscope. At present, most colonoscopes have a 140° angle of view, but only one manufacturer has a standard production model colonoscope with a 170° angle of view (Olympus Medical Endoscope, Tokyo, Japan) ( Figs. 1 and 2 ). An evaluation of a 15-mm diameter colonoscope with a 210° angle of view, in which the lens projects from the endoscope tip permitting an ultrawide angle of view, has been performed. With this instrument, the viewing angle could be converted to 160° for close inspection of the mucosal surface. This study included 50 patients randomized to the ultrawide-angle colonoscope compared with a standard colonoscope with a 140° angle of view. There was no difference between the 2 types of colonoscopes in the detection of adenomas, but the miss rate for polyps was somewhat lower with the ultrawide-angle colonoscope. It is interesting that of two examiners, one found no difference in adenoma detection between the 2 types of colonoscopes, but the second examiner missed more polyps with the ultrawide-angle colonoscope than when using a colonoscope with a 140° angle of view. The investigators concluded that the principal deficit of the extremely wide-angle colonoscope was that the resolution was significantly reduced when compared with standard colonoscopes.
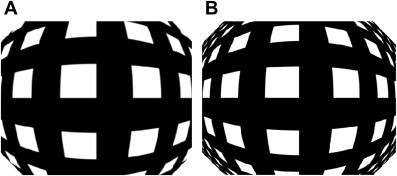
A randomized tandem colonoscopy study in 50 patients comparing a colonoscope with a 170° angle of view with a 140° instrument demonstrated that the miss rate for all polyps with the wide-angle colonoscope was similar to the miss rate with the standard colonoscope. In this study, 50 patients were randomized to have colonoscopy with the standard instrument first (140° angle of view) or to have colonoscopy with the wide-angle instrument as the first examination. The miss rate for all polyps with the wide-angle colonoscope was not statistically different from the miss rate for all polyps with the standard colonoscope. It should be noted that neither of the tested instruments were high-definition instruments, and the only parameter that was different between the 2 endoscopes was the angle of view of the lens. The conclusion of the investigators was that “in comparison with other innovations for reducing polyp miss rates during colonoscopy … wide angle colonoscopy may be the least effective strategy.” A similar conclusion was reached by a group from Spain who randomized, in a one-to-one ratio, 620 patients into those having colonoscopy with a wide-angle high-definition instrument versus procedures using a standard colonoscope. This study showed no significant difference in the number of adenomas detected by either instrument. A study with 8 colonoscopists at 2 institutions randomized 710 patients using a standard (140° angle of view) colonoscope and a 170° wide-angle instrument. Neither instrument had a high-definition component. The primary end point of this study was to see if there was a reduction in withdrawal time using the wide-angle instrument as compared with the standard colonoscope. The mean insertion time for the 2 instruments was similar, at approximately 5 minutes, but overall the mean withdrawal time was shorter with the wide-angle colonoscope than with the standard colonoscope (4.9 vs 5.4 minutes); however, the shorter withdrawal time was only statistically significant for 3 of the 8 endoscopists. In this study, the proportion of patients with at least one adenoma was significantly higher for the standard instrument than for the wide-angle colonoscope. However, there was no difference in the mean number of adenomas detected with either instrument. The conclusion was that although there was a 30-second reduction in mean withdrawal time using wide-angle instruments, the benefits of the wide-angle colonoscope “appeared minimal on close inspection.”
In contrast to the majority of reports, a nonrandomized study from Prague compared wide-angle high-definition colonoscopy with standard-angle (140°) instruments with and without high definition. A total of 507 patients were involved in the study, which showed that the wide-angle high-definition instrument detected more adenomas, flat adenomas, and adenomas with advanced histology as compared with both instruments with a 140° angle of view. The instruments were not randomly assigned in this study, but the mean rate of adenomas and flat adenomas found per patient was significantly higher in the wide-angle high-definition colonoscopic group compared with the other groups, and in the right colon was almost double that found with the standard-angle colonoscopes. The currently available 170° wide-angle instrument also has a high-definition component. The question arises as to whether the high-definition component increases the ability of the examiner to find more polyps and adenomas than can be found with the wide-angle component alone.
A retrospective report from the Cleveland Clinic compared endoscopic findings in more than 400 individuals who underwent examination with a wide-angle high-definition colonoscope and compared them with a group who had conventional colonoscopy (non–high definition) with a 140° angle of view that were matched for gender, age, and indication for colonoscopy. This study was not randomized, and polyps were detected in 39.9% of the subjects in the high-definition/wide-angle group and in 36.9% of those in the conventional colonoscopy group. The investigators concluded that wide-angle high-definition colonoscopy afforded no increase in the detection of polyps or adenomas over conventional colonoscopy with 140° angle of view, and that the improved resolution and wider angle of view does not increase the ability to see polyps and adenomas.
Another study reported a large randomized trial but did not show any objective advantage of the high-definition instrument using narrow-band imaging over the same wide-angle high-definition scope using white light imaging. Only hyperplastic polyps were found to be more frequent in the group for whom narrow band imaging was used. Other investigators using tandem colonoscopy and either narrow band imaging or white light (both with wide-angle high-definition instruments) found that the neoplasm detection rates were similar when the mucosa was viewed with narrow-band imaging or white light. The conclusion was that they did not find narrow-band imaging to significantly influence the likelihood of missing or detecting a colorectal neoplasm as compared with white light.
During evaluation of the wide-angle instruments, multiple comparisons have been made to study whether there is any significant difference in cecal intubation with the 170° colonoscope as compared with one with a 140° angle of view. The 2 instruments being compared in several reports were identical in every aspect except for the angle of view. In one study, the mean insertion time to the cecum was shorter with the wide-angle colonoscope than with the standard colonoscope (2.09 vs 2.53 minutes). Similarly, the mean withdrawal time was shorter with the wide-angle instrument (4.98 vs 5.74 minutes) than with the standard colonoscope. Colonoscopists in a dual-center study also looked at the insertion time of a standard colonoscope versus a wide-angle colonoscope. The mean insertion time was similar, and the mean withdrawal time of the wide-angle instrument was somewhat shorter than for the standard colonoscope, 4.9 minutes versus 5.4 minutes, respectively. Another study with the wide-angle instrument determined that its use resulted in a more rapid examination, with the mean time for examination with the wide-angle colonoscope being 6.75 minutes versus 7.64 minutes with the standard colonoscope. During this evaluation the aim was to withdraw the standard or the wide-angle colonoscope as rapidly as possible while yet being able to examine the entire lumen and the proximal side of any fold or structure. The mean extubation time with the wide-angle colonoscope was reduced by 25% to 30% as compared with the 140° instrument. Another report compared the standard colonoscope with the wide-angle colonoscope, and found no statistical difference in either intubation or withdrawal time between the 2 instruments when a minimal 6-minute extubation time was mandated. The reports in the medical literature confirm that the extubation time may be up to 1 minute shorter with a wide-angle colonoscope because of the ability to expose a greater surface area than can be visualized with an instrument having a 140° angle of view. However, this does not translate into a clinically meaningful advantage unless it results in a greater polyp-finding capability. The polyp miss rate has been investigated (vide supra) and there has been no significant difference shown in the probability of missing polyps as adenomas, whether the instrument used had a wide-angle as opposed to a narrower angle of view.
In the continuing quest to find changes in design, techniques, or accessories to make the colonoscopic examination more efficient, a cap or hood in the instrument has been investigated. The use of this device keeps the tip of the scope from contacting the mucosal surface to prevent obstruction of vision when the scope tip is deflected around a fold or a bend in the colon. The cap could be of use to flatten folds and thus see lesions that grow behind folds unseen by standard straightforward colonoscopy. It was the consideration that a clear plastic cap could be used as an extension of the colonoscope’s tip while permitting the portion of mucosa that is deflected to be seen through the transparent hood ( Fig. 3 ).

Use of a transparent cap to assist in viewing behind haustral folds was suggested in 1995 by Inoue and colleagues. In this article, the cap was reported to avoid contact of the lens with the mucosal surface, and the colon wall could be seen through the clear plastic hood attached to the colonoscope tip. The investigators described that the area behind folds could be observed by compressing the fold to flatten it using the edge of the cap. In 1998 Matsushita and colleagues described in 24 subjects a decreased miss rate for polyps when using a transparent cap as compared with a colonoscope without the cap. This tandem study randomized patients with known polyps to an examination with or without the cap. No polyps were missed when using the cap as opposed to a 15% miss rate with standard colonoscopy. All of the missed polyps were smaller than 5 mm except one of 8 mm diameter.
Using a colonoscope with a transparent hood, Kondo and colleagues found in a randomized control trial of 721 patients at least one polyp in significantly more subjects than in those with no hood, but prevalence rates (polyps/patient) were identical. The conclusion of the investigators was that a cap that extended 4 mm from the faceplate of the colonoscope did not interfere with intubation, but its ability to depress folds and reduce the blind areas hidden behind them led to a higher rate of polyp detection.
Horiuchi and Nakayama performed repeat colonoscopy with an experimental transparent retractable extension hood months after initial colonoscopy showed the presence of adenomas; more adenomas were found on the second examination using the hood. A similar finding was reported from this group in a more recent publication. This unique device has the capability to extend or retract a 7-mm clear plastic cap affixed to the tip of a colonoscope. The hood responds to air pressure delivered to bellows on the cap through a long slender catheter attached externally along the length of the colonoscope. Its usefulness is that fluid and debris that collects and pools in a fixed cap can interfere with vision, but retraction of the cap permits complete clearing.
Hewett and Rex performed a tandem study with 100 subjects, reporting a significantly lower miss rate for cap-fitted colonoscopy versus regular colonoscopy (21% vs 33%, P = .039). However, it should be noted that there was still a considerable miss rate even when the cap was applied. Improvement in detection was limited to diminutive adenomas (<5 mm), and there was no significant difference in per-patient miss rates in the comparison of the 2 groups.
Not all reports of the transparent cap on the scope show a benefit in polyp detection. In a report of 592 patients by Harada and colleagues, there was no difference in polyp detection rate between the randomized-cap and no-cap groups. Lee and colleagues, in a randomized prospective trial involving 11 endoscopists in 2 centers, found a significantly lower adenoma detection rate with the cap in place during the evaluation of 1000 patients.
In general, the literature on cap-assisted colonoscopy for diagnostic purposes is inconsistent, and this device does not seem to be of universal benefit for locating polyps hidden behind folds or in the deep valleys between haustral folds.
In addition to wide-angle optics, and a cap on the endoscope tip, other innovations and variations have been introduced in an attempt to enhance the ability of the colonoscopic examination to find more polyps (or miss less polyps) during the examination, including an adequate bowel preparation, slow withdrawal time, high-resolution imaging, dye spray, and narrow band imaging. Despite meticulous techniques and new imaging tools, lesions behind the colonic folds may be impossible to see by any addition to the straight end-on colonoscopic examination.
Retroversion of the colonoscope in the rectum has long been considered an integral part of colonoscopy. A similar capability is possible in the proximal colon, but not investigated until recently. The bending capability of flexible instruments has resulted in frequent episodes of inadvertent retroflexion of colonoscopes during attempts to perform intubation to the cecum. It is possible to purposefully perform retroflexion of the instrument throughout various parts of the colon, in a similar fashion to the procedure that is more routinely performed in the rectum during a colonoscopic examination. A comparison was made between 2 prototype scopes and a standard colonoscope to evaluate the effectiveness and utility of performing retroflexion in the colon. The standard commercially available Olympus pediatric colonoscope has a bending section length of 10 cm (Olympus Medical Instruments, Tokyo, Japan). A prototype instrument with a shorter bending length of 6.7 cm was specifically designed for its capability of easy retroflexion and was compared with a pediatric instrument that has a standard length-bending section, but has a tighter radius of tip deflection curvature than a standard colonoscope. With these instruments, cecal retroflexion was attempted, defined as the ability to see the ileocecal valve orifice en face and also to be able to visualize part of the ascending colon in the retroflexed position. The result was no difference in intubation time to the cecum between the standard pediatric colonoscope and the instrument that had the same length-bending section but a tighter radius of tip deflection. However, during the use of the instrument with a shorter bending section, cecal intubation times were longer and more maneuvers were necessary (abdominal pressure/variable stiffness device activation/position change) to intubate the cecum with the shorter tip deflection instrument. The 2 prototype instruments showed a significantly higher rate of being able to perform retroflexion than the standard pediatric colonoscope; there was no difference between them in the success rate of cecal retroflexion. The success of retroflexion in the cecum was 57% for the standard pediatric colonoscope, and 91% and 94% for the prototype instruments. There was a 98% success rate for all instruments for intubation of the terminal ileum. It was thought that the instrument with the shorter bending section, although easily retroflexed in the cecum, took longer to pass to the cecum and was more likely to require additional maneuvers to reach the cecal tip. The consideration was that the very tight turning radius of the bending section along with the shortened tip resulted in difficulty with advancement because the colonoscope was not able to bend sufficiently when pushed against the wall of the colon. From personal observations the author, too, noted that a short bending section made the colonoscopic examination much more difficult, presumably because the short bending section did not permit the instrument to be pulled back and straightened in a normal fashion, since the bending section was too short to bridge across the lumen of the colon and allow the instrument to be pulled back and straightened. Whenever a straightening maneuver was attempted, the short tip failed to anchor itself in the colon, so that pulling back with the tip deflected merely resulted in pulling the instrument out of the colon without straightening.
Another study was performed with similar instruments, but using adult colonoscopes. One of the prototype adult instruments had a bending section length of 13 cm and the other a length of 11.5 cm. These 2 specialty instruments were randomized, with the standard adult colonoscope not being one of the study instruments. In general, there was no difference in the mean time to the cecum or any of the ancillary measures required for passing the instrument. Regarding these adult colonoscopes, the instrument with a shorter bending section could be retroflexed in the cecum more often than the other, but there were no other significant differences noted with either instrument.
Two articles have discussed the removal of colon polyps during retroflexion with a colonoscope. In the first study, the same 2 prototypes of the pediatric type of colonoscope were used. One has a shorter bending section and the other has a tighter tip deflection radius in the right/left direction as compared with the standard pediatric colonoscope. The technique used for instrument deflection was to advance the instrument tip several haustral folds proximal to the polyp (except when cecal polyps were present). The dial controls were used to deflect the tip maximally in both the left and up directions, and the instrument was then torqued in a counterclockwise (left) direction occasionally with advancement of the shaft. Once a retroversion maneuver had been completed, the colonoscope was then withdrawn until the polyp was visualized. Standard polypectomy procedures were used to remove 59 consecutive large sessile polyps proximal to the rectum. Fourteen polyps were removed partially or completely in the retroflexion mode. There were no perforations and no complications related to retroflexion. The polyps removed in retroflexion could only barely be visualized in the forward view and all could not have been removed except by using the retroflexion technique. A similar report detailed 15 polypectomies with endoscopic retroflexion. All of the polyps were sessile and large (average size 38 mm, range 20–60 mm); of these polyps 3 were in the cecum, 3 in the ascending colon, 3 at the hepatic flexure, 3 in the transverse colon, 2 at the splenic flexure, 2 in the descending colon, and 2 in the sigmoid colon. The procedures were performed using a standard Pentax colonoscope (EC3831L; Pentax Precision Instrument Corporation, Orangeburg, NY, USA). The technique for retroflexion was: advance the scope beyond the index polyp, reduce all the loops in the instrument; bend the tip of the colonoscope fully upward; and advance the instrument until the polyp is seen. Scope rotation was sometimes necessary. Standard polypectomy techniques with endoscopic mucosal resection were performed in both forward and retrograde approaches. There were no endoscopic complications.
The investigators of both these reports state that retroflexion attempts should be stopped if the endoscopist feels resistance when bending the tip or when trying to advance the scope. Often, the use of an upper endoscope may be a good alternative especially when retroflexing in the left colon.
A disappointing view of the value of retroflexion in the right colon during screening colonoscopy was published by the Indiana Group. One hundred patients had all polyps removed between the cecum and splenic flexure and then a repeat examination was performed from the splenic flexure to the cecum and back, looking for polyps that had been missed during the original scan and polypectomy. Following the first examination, the cecum was then reintubated and the patients were randomized to a second examination either using a straightforward viewing technique or by using a retroflexed mode. Standard instruments were used along with prototype pediatric colonoscopes with a short bending section or a tight radius of bending curvature of the tip. Retroflexion was readily made in the ascending colon and transverse colon, but the standard adult colonoscope could only be retroflexed in the cecum approximately 40% of the time and a standard pediatric colonoscope could be retroflexed in the cecum approximately one-third of the time when attempted, whereas the prototype instruments could be retroflexed in the cecum more than 90% of the time. The calculated miss rate for polyps/adenomas found in the forward view during reintubation after the initial colonoscopist removed all polyps was 37%/33%, and when the retroflex examination was performed the incidence of missed polyps/adenomas was 38%/23%. In this report, the calculated miss rate on the second examination when performed in retroflexion was numerically lower than when the second examination was performed in the forward view. The explanation proffered in this report was that the retroflexion does not expose the entire colon to view because the instrument may be difficult to maneuver during retroflexion, or that polyps located in hidden positions on the proximal sides of folds are not the principal mechanism accounting for failure of detection during colonoscopy. Although no complications were seen during this randomized study, the investigators cautioned against routine retroflexion in the right colon because of the possibility of complications.
Rectal retroflexion, on the other hand, has long been taught as the “routine” concomitant to a total colonoscopy. There have been few studies on the yield of finding significant pathology during rectal retroversion. An article from the Indianapolis group performed rectal retroversion on 1502 consecutive patients enrolled in a study of several aspects concerning rectal retroversion. Retroflexion was successful in about 94% of patients, but was not performed in 6% because the rectum appeared narrow. During this study, 7 polyps were visualized only by retroflexion (following a careful planned extubation of the colonoscope with special attention to the rectal mucosa right down to the anal verge). Of these polyps, 6 were hyperplastic sessile polyps and 1 was a 4-mm sessile tubular adenoma. Despite this finding, several gastroenterologists are committed to the concept of performing a rectal retroversion before or after total colonoscopy to visualize the area surrounding the dentate line and the distal rectum. Although there have been reports of perforation related to rectal retroversion, and a few reports of closing those perforations with clips, it is the consideration of this author that rectal retroversion should be performed and need not be uncomfortable for the patient. The technique is to withdraw the colonoscope to the anal verge following a total colonoscopic examination. The instrument is then advanced up to the first or second valve of Houston with the apex of the valve placed at the 12-o’clock position in the visual field. The colonoscope tip is then deflected maximally up and the colonoscope gently advanced, usually resulting in a retroflexion maneuver. If this does not work another valve should be approached, which may be on the right or on the left. The tip of the endoscope is then placed on a distal aspect of the valve and with the tip maximally deflected the scope is then advanced gently. Once the U-turn has been made, the right/left control should be locked and moved maximally to the right, and the shaft of the instrument held near the perineum is rotated in a clockwise fashion, while withdrawing the instrument to move the lens closer to the anal verge. Should the patient complain of pain when the instrument is advanced into the rectum, that particular attempt should be abandoned and another fold approached. Patients should not be discomforted by the retroversion maneuver, and if they are, the tip should be moved to a different location for another attempt. Occasionally the rectal vault may be small, such as occurs after radiation therapy to the pelvis, in inflammatory bowel disease, or in slender women who may have an acute angulation just inside the anal verge. During these circumstances, rectal retroversion should not be performed, and if painful, any attempt should be stopped to avoid a perforation.
The main reason that retroflexion is performed by endoscopists is to visualize more of the mucosal surface, especially those areas that are not well seen by direct end-on examination with the standard colonoscope, whether the location of the instrument tip is in the cecum or the rectum.
As noted before, instrument manufacturers have been dealing with the problem of making an instrument that easily retroflects throughout the large bowel, but up to now the major instrument manufacturers have not come up with an instrument that can easily perform forward and backward (retroflexed) views of the colon. To this end, Avantis has developed a small-caliber endoscope that can fit through the instrument channel of a standard colonoscope. The third-eye retroscope (TER; Avantis Medical Systems Inc, Sunnyvale, CA) was developed specifically because of the inability of the standard forward-viewing colonoscope to find all of the polyps that are located behind folds and flexures in the colon during screening procedures.
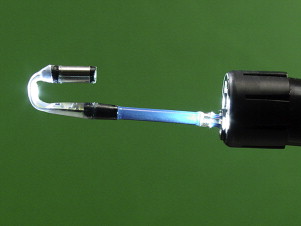
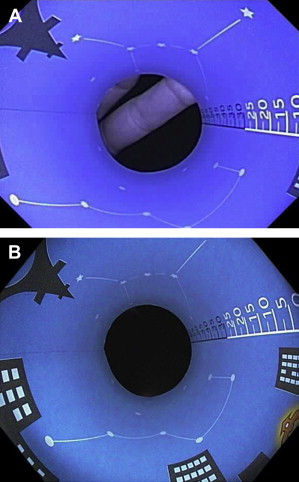
The TER is a miniature self-contained endoscope that is passed through the accessory channel of a standard colonoscope, and when positioned beyond the tip of the colonoscope permits a retrograde view of the colon ( Fig. 4 ). Whereas the standard colonoscope provides an image of the colon in a forward direction, the TER looks backward toward and beyond the faceplate of the colonoscope, visualizing the proximal aspect of folds as the colonoscope simultaneously views their distal surfaces. The disposable TER is a marvel of engineering, with its built-in 180° tip angulation, light source, and video chip being contained in a flexible sheath of 2.5 mm external diameter, with the tip housing the camera being 3.5 mm. To prevent triggering the automatic brightness reduction feature built into the colonoscope, the TER has a polarized light-emitting diode (LED) matched to a polarized filter affixed to the colonoscope tip before the procedure. This configuration results in the colonoscope light being as bright as usual and not diminished in intensity by the built-in light sensor, resulting in full illumination for both forward and retrograde viewing.