Videourodynamics combines fluoroscopic voiding cystourethrography with multichannel urodynamics to better evaluate lower urinary tract symptoms. This article reviews current literature and guidelines outlining the indications for obtaining this specialized study as well as technique. Appropriate and judicious use of fluoro-urodynamics lends to improved diagnostic acumen in a well-selected patient population; however, clinicians must be mindful of the added cost, safety concerns, and limitations of its use.
Key points
- •
Videourodynamics (VUDS) combines a fluoroscopic voiding cystourethrogram with multichannel urodynamics, allowing anatomic and functional assessment of the bladder and outlet.
- •
There is a relative paucity of guidelines and literature surrounding the specific indications and techniques for VUDS.
- •
A thorough patient assessment is paramount in developing a differential diagnosis and identifying urodynamic questions to be answered.
- •
VUDS should be considered in patients with neurologic findings or diseases as well as those with obstructed voiding, congenital genitourinary anomalies, or a history of genitourinary reconstruction.
- •
Appropriate use of fluoroscopy is important in reducing any added cost and risk of ionizing radiation to patients and clinical staff.
Introduction
Diagnosing patients with multiple lower urinary tract symptoms and confounding comorbidities may require further assessment with advanced diagnostic testing, such as urodynamics. Standard multichannel urodynamics most often includes a filling cystometrogram and a pressure flow study during micturition. These 2 components are often the only obligatory tests required to determine a diagnosis; however, key pathognomonic findings may be overlooked in certain patient populations. Further delineation may be required, and the use of concomitant radiologic imaging during the study provides additional data to hone the differential diagnosis. Fluoroscopic imaging has been the modality of choice as an adjunct to traditional urodynamics.
Combining fluoroscopic voiding cystourethrogram with pressure flow urodynamics to evaluate lower urinary tract function dates back to the 1950s, was further developed through the 1970s, and was not widely used clinically until the 1980s. The original set-up used analog portable fluoroscopy (C-arm) and signal processing to combine the oscilloscope tracing from the pressure transducer with the live fluoroscopic images. This allowed simultaneous recording on a magnetic tape for cine image viewing, hence, the coined term, VUDS .
Improvements in portable computing and digital signal processing paved the way for modern-day VUDS (also referred to as fluoro-urodynamics). Imaging input (video) is channeled into a computer terminal with software chronologically integrating the digital image with the cystometrogram and pressure flow tracings. Advancements in imaging technology paralleled the changes in computing, and digital imaging detectors led to fully integrated digital fluoroscopy. This has allowed easier combination of the 2 technologies and facilitates review of imaging on specialized medical image viewing software with improved resolution and tools to optimize image analysis.
VUDS provides additional information compared with standard urodynamics; however, use of this specialized test should be limited to patients in whom this information adds value. There is increased cost and risk associated with radiologic imaging and clinicians should consider the usefulness of adding fluoroscopy as part of a patient’s evaluation.
Introduction
Diagnosing patients with multiple lower urinary tract symptoms and confounding comorbidities may require further assessment with advanced diagnostic testing, such as urodynamics. Standard multichannel urodynamics most often includes a filling cystometrogram and a pressure flow study during micturition. These 2 components are often the only obligatory tests required to determine a diagnosis; however, key pathognomonic findings may be overlooked in certain patient populations. Further delineation may be required, and the use of concomitant radiologic imaging during the study provides additional data to hone the differential diagnosis. Fluoroscopic imaging has been the modality of choice as an adjunct to traditional urodynamics.
Combining fluoroscopic voiding cystourethrogram with pressure flow urodynamics to evaluate lower urinary tract function dates back to the 1950s, was further developed through the 1970s, and was not widely used clinically until the 1980s. The original set-up used analog portable fluoroscopy (C-arm) and signal processing to combine the oscilloscope tracing from the pressure transducer with the live fluoroscopic images. This allowed simultaneous recording on a magnetic tape for cine image viewing, hence, the coined term, VUDS .
Improvements in portable computing and digital signal processing paved the way for modern-day VUDS (also referred to as fluoro-urodynamics). Imaging input (video) is channeled into a computer terminal with software chronologically integrating the digital image with the cystometrogram and pressure flow tracings. Advancements in imaging technology paralleled the changes in computing, and digital imaging detectors led to fully integrated digital fluoroscopy. This has allowed easier combination of the 2 technologies and facilitates review of imaging on specialized medical image viewing software with improved resolution and tools to optimize image analysis.
VUDS provides additional information compared with standard urodynamics; however, use of this specialized test should be limited to patients in whom this information adds value. There is increased cost and risk associated with radiologic imaging and clinicians should consider the usefulness of adding fluoroscopy as part of a patient’s evaluation.
Indications
Fluoroscopy as an adjunct to standard urodynamics should be considered in those patients whose diagnosis is aided by including this modality. Specialty societies have developed guidelines for standardizing terminology and technique as well as clinical guidelines for use of urodynamics. These guidelines are a consortium of expert panel opinion and literature review. A majority of recommendations apply to standard urodynamics and there is a paucity of guidelines and literature surrounding the specific indications and techniques for VUDS. Information in this article is derived from guidelines and available literature; however, much of the described principles and techniques follow expert opinion and the authors’ standard practice.
Determining the patient populations that may benefit from VUDS requires clinicians to develop a differential diagnosis of underlying conditions that may contribute to a patient’s urinary tract symptoms. This begins with a detailed history and physical examination. The history should include comorbid conditions and querying for any neurologic dysfunction as well as a family history of neurologic and congenital conditions. Knowledge of congenital anomalies and previous surgeries, in particular those involving the genitourinary or neurologic system, aids in patient selection. During examination, clinicians should evaluate for any signs of neurologic disease by assessing perineal sensation, pelvic muscle, and sphincter tone; testing the bulbocavernosus reflex; and identifying peripheral neuropathy or abnormalities of the vertebral column. In men, prostate size should be noted and the external urethral anatomy examined. In women, the examination includes evaluation of urethral mobility, incontinence, periurethral anatomy, and pelvic organ prolapse. Thorough assessment guides clinicians in formulating the diagnostic questions necessary to select the relevant urodynamic components.
Patients who may benefit from VUDS include those with neurologic findings or a history of neurologic disease, a history of congenital genitourinary anomalies, symptoms of obstructive voiding (often excluding straight forward benign prostate enlargement [BPE] symptoms), a history of pelvic irradiation, and a past history of surgical reconstruction. Current guidelines jointly published by the American Urological Association (AUA) and the Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction (SUFU) make only 2 recommendations regarding the use of VUDS. These include recommending that clinicians may use fluoroscopy at the time of urodynamics in patients with relevant neurologic disease or those with an elevated postvoid residual or urinary symptoms and a neurologic condition that may contribute (guideline statement 12). The other recommended condition is in patients with outlet obstruction to localize the level of obstruction, particularly in those thought to have primary bladder outlet obstruction (PBNO) (guideline statement 19).
The use of fluoroscopy during urodynamics can aid in further evaluation of
- •
Vesicoureteral reflux (VUR)
- •
Anatomic variations of the bladder, including trabeculations, saccules or diverticula, and filling defects
- •
Voiding dynamics in women with a cystocele or pelvic organ prolapse
- •
Bladder neck function and coordination during micturition
- •
Urethral pathology, such as strictures or diverticula
- •
Detrusor–external sphincter dyssynergia (DESD) (in conjunction with sphincter electromyography [EMG])
- •
Dysfunctional voiding/pelvic floor dysfunction
- •
Urinary fistulas
- •
Urinary incontinence
Neurogenic Bladder
VUDS is often useful in the evaluation of patients with suspected neurogenic lower urinary tract dysfunction (NLUTD). Clinical diagnoses include spinal cord injury; spina bifida or spinal dysraphism; Parkinson disease; Shy-Drager syndrome (multiple system atrophy [MSA]); demyelinating disorders, such as multiple sclerosis; Devic disease; and transverse myelitis and, in some cases, diabetic neuropathy and following a cerebrovascular incident. This list is not all inclusive and clinical acumen is needed to determine other signs, symptoms, and underlying pathology that may lead to neurologic dysfunction.
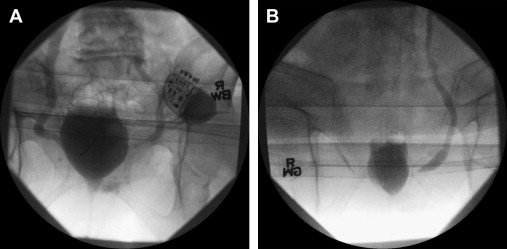
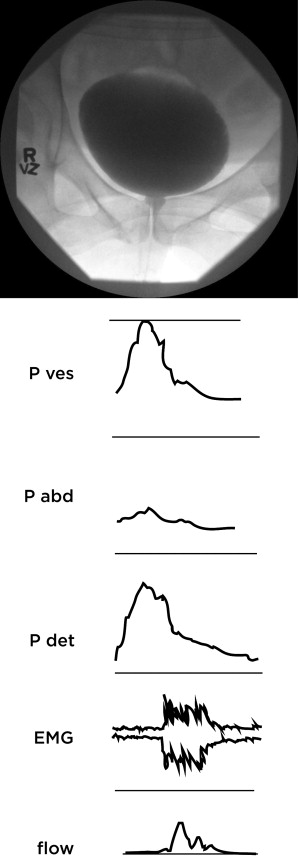
Key pathognomonic findings in NLUTD that are better evaluated with VUDS include VUR, which may indicate poor bladder compliance, and identifying improper coordination between detrusor contraction and sphincter relaxation. Either of these findings typically represents neurogenic bladder, and, if a neurologic disease is not known, these findings should prompt exclusion of a potential neurologic disease. Fig. 1 demonstrates 2 cases of bilateral VUR that occurs with bladder filling. In both cases, detrusor pressure remained normal and the only indication of bladder compliance changes was the identification of reflux. DESD occurs with lesions above the reflex pathways within the sacral spinal cord. With patch electrodes, the EMG tracing is not always diagnostic due to noise, and fluoroscopic findings may be the only evidence to suggest this condition ( Fig. 2 ). Assessment of bladder contour may provide additional insight toward the underlying pathology. For example, trabeculations, multiple diverticula, or a Christmas tree appearance indicates obstruction, possibly related to neurogenic dysfunction, in those with a known neurologic condition.