Vascular Lesions
A number of vascular lesions affect the large intestine. In this chapter we will deal with nonneoplastic vascular abnormalities. Vascular tumors are covered in Chapter 19.
Portal Colopathy
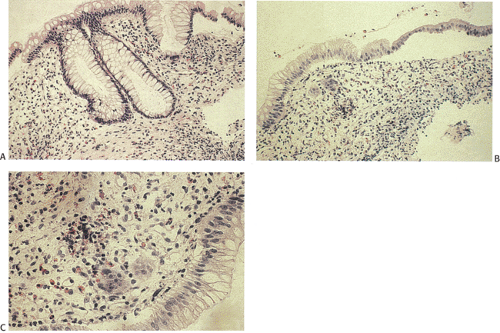
Patients with portal hypertension often develop hematochezia, Hemoccult-positive stools, and anemia. Some patients develop hemorrhoids (533); most patients have esophageal varices. Seventy percent of patients have a mosaic mucosal vascular pattern or multiple vascular ectasias. The ectasias cause both acute and chronic gastrointestinal bleeding (534). Other endoscopic mucosal abnormalities include edema, erythema, granularity, and friability, features often seen in colitis (535). Histologically, increased numbers of small vessels with prominent branching lie in the upper and midmucosa. The dilated, tortuous mucosal capillaries may show irregular thickening and arterialization of their walls. Vascular diameters can measure 20 ± 2 micra in the ascending colon and 30 ± micra in the rectum (536). These findings associate with edema of the lamina propria and mild chronic inflammatory changes (537). The typical signs of portal hypertension are present, including dilation and tortuosity of the mesenteric veins. Neither signs of chronic liver disease nor stigmata suggestive of severe portal hypertension correlate with the endoscopic findings. The colonic lesions resemble those found in portal gastropathy, an entity discussed in Chapter 4.
Varices
Esophageal varices are well known, but it is not generally appreciated that varices can involve the rest of the GI tract (538). Adhesions or enterostomies favor the formation of intestinal varices if portal hypertension is present. Patients with pancreatitis and splenic vein thrombosis also develop colonic varices (539). Colonic varices may also occur on a familial basis in the absence of portal hypertension (540). Mean patient age is 50 and there is a slight male predominance. Sites where
varices form reflect the embryonic juxtaposition of visceral and systemic vascular plexuses. Portal hypertension not only causes dilation of the pre-existing natural shunts with creation of collateral vessels, but also reopens embryonic vessels, particularly the periumbilical veins, producing the caput medusae.
varices form reflect the embryonic juxtaposition of visceral and systemic vascular plexuses. Portal hypertension not only causes dilation of the pre-existing natural shunts with creation of collateral vessels, but also reopens embryonic vessels, particularly the periumbilical veins, producing the caput medusae.
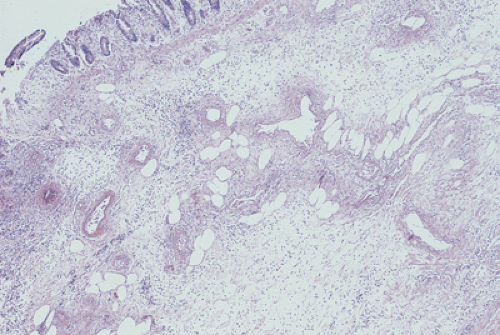
In patients with portal hypertension, the coronary azygous system is the primary portal–systemic channel in 50% of cases; in 25% the inferior mesenteric and internal iliac systems represent the primary portal–systemic channel. Portal–systemic communications also exist in the rectum. Prominent dilated vessels are present in the submucosa (Fig. 13.161). The histology of the varices resembles that of esophageal varices (see Chapter 2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree