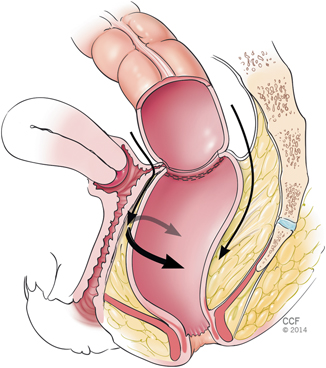
Fig. 36.1
Demonstration of the digital rectal examination. The tip of the finger corresponds to the anorectal ring where the linear stapler is placed for double-stapled anastomosis or purse-string sutured applied for single-stapled anastomosis. (Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2014. All rights reserved)
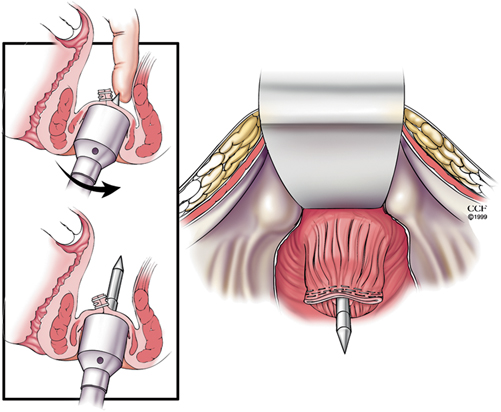
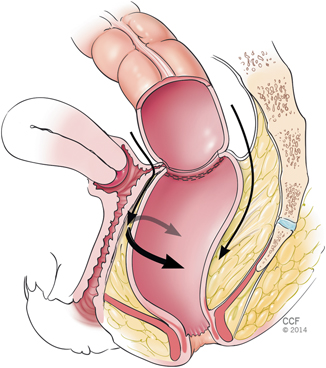
Fig. 36.2
In the double-stapled anastomosis, the trocar of the stapler should traverse just posterior to the staple line. This can be facilitated by putting the index finger from the abdominal side and guiding the trocar posterior to the staple line. (Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2014. All rights reserved)
Another maneuver to avoid vaginal injury is the retraction of the vagina anteriorly with lighted deep pelvic retractors. This helps prevent the redundant posterior vaginal wall from being accidentally incorporated within the staple line (Fig. 36.3). In addition to these, vaginal bougies and/or obturators inserted via the perineal approach can delineate the anatomy, facilitate pelvic dissection and to avoid this complication in reoperative pelvic surgery.
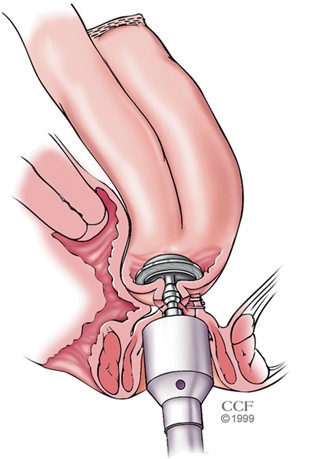
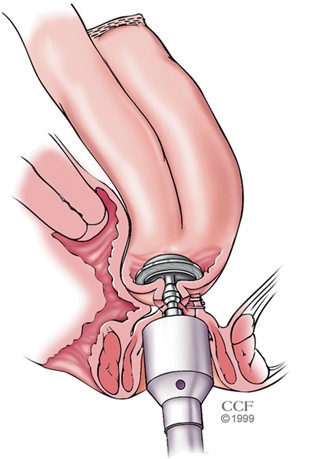
Fig. 36.3
Incorporation of the redundant posterior vaginal wall within the staple line during double-stapled anastomosis (this complication can be prevented by anterior retraction of the vagina with deep pelvic retractors). (Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2014. All rights reserved)
How to Fix Vaginal Injury
Most of the time, a high-level vaginal injury is related to the inadequate anterior mobilization of the rectum. Normally, rectal mobilization requires a minimum of 2 cm anterior dissection below the level of planned anastomosis. Once this complication happens, the surgeon should take a pause and get a proper assistance. To fix the problem, complete exposure of the operative area should first be obtained even if this requires a conversion of a laparoscopic case to a full laparotomy. It would not be wise to tackle the area of injury first even though it seems tempting for the surgeon. The surgeon needs to strategize the operative plan. In this case, the vaginal injury has occurred due to inadequate rectal mobilization. Therefore, it is critical to fully mobilize the rectum and further separate the rectovaginal septum lower than the level of injury. In order to accomplish this, the rectum should first be further mobilized posteriorly and laterally and then the dissection should be continued to the anterior side below the level of injury (Fig. 36.4). Only then it is proper to disconnect the anastomosis, where the vaginal injury has occurred. Attempting to disconnect the anastomosis prematurely without full posterolateral and anterior rectal mobilization lower than the area of injury can further complicate the situation. This technique minimizes the risk of further injury and/or enlarging vaginal defect by identifying the proper tissue planes. Furthermore, it may also enable the surgeon to do a second attempt of a double-stapled anastomosis. If a second attempt of double-stapled anastomosis is not a possibility, then a single-stapled anastomosis remains a very good option as seen in Fig. 36.5. For this, after identifying the vagina and separating it off the anastomosis, a small proctotomy is made at the anterior wall and stay sutures are placed. Starting from the anterior wall, a purse-string suture is applied circumstantially around the anorectal stump by hand and tied down over the trocar, and then the gastrointestinal continuity is established by creating a single-stapled anastomosis. If the omentum is present, omental pedicle flap can be used to patch the vaginal site following its primary repair.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








