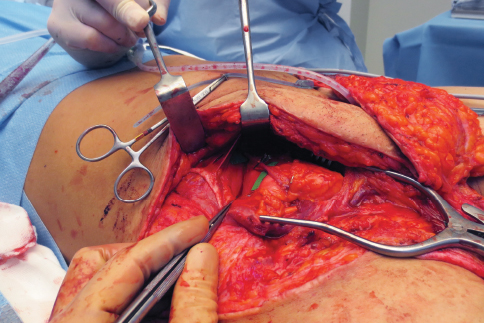
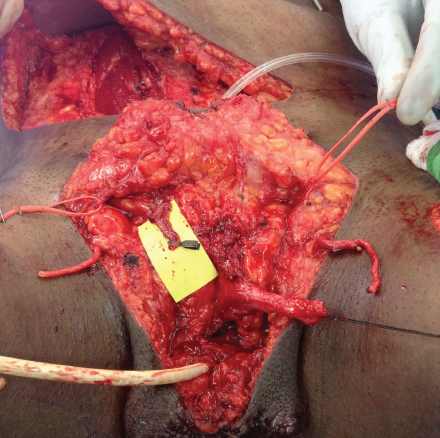
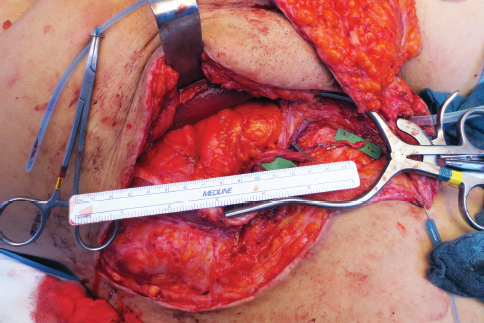
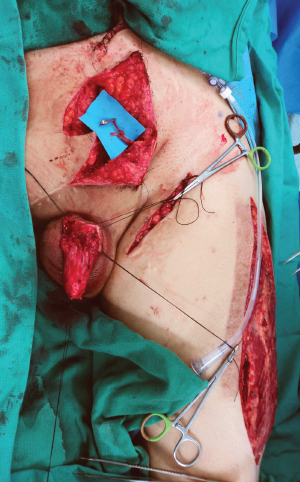
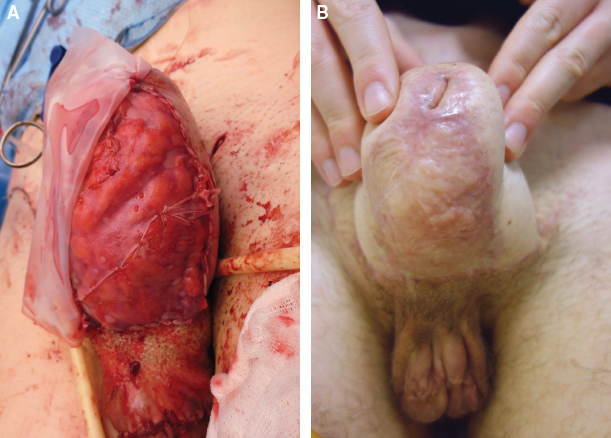
CHAPTER 13 Potential unfavorable results will be classified according to a chronologic order of immediate, early, delayed, and late “complications.” Solutions and preventive measures will be described case by case. We will define what “an unfavorable result” is. A phalloplasty is a complex surgical procedure that requires different reconstructive steps and the use of one or more sensate-free and/or pedicled flaps to obtain an aesthetic and functional penile construction. An unfavorable phalloplasty result includes all flap-related complications and all cases that have failed to achieve the ideal goals of a phalloplasty as described by Hage and de Graaf1 and Monstrey et al.2 Even with the substantial progress in phalloplasty, a single technique that produces an ideal neophallus without complications has not yet been found, and given its complexity, it is unlikely that there will be a procedure in which revision surgery is never needed. Thus part of this chapter will discuss the actual handling of untoward events, but part will also detail the functional and aesthetic improvement of previously performed phalloplasties that have failed to achieve these goals. An example of this category is an “uncomplicated” phalloplasty that was performed without urethral reconstruction. Thus, although no complications occurred in the initially performed procedure, the goal of voiding while standing has not been achieved. Because the population of these often rightfully demanding patients seeking revision or improvement is constantly increasing, we will also describe possible ways of improving previous incomplete or unfavorable phalloplasties. This latter category will be named redo-phalloplasties. In a transgender individual the ideal penile construction should achieve the following goals3: Based on the experience in our centers, we will consider only phalloplasty surgery with the radial forearm flap (RFF) and the anterolateral thigh (ALT) flap. There can be a problem with the vascularity of both a free and pedicled flap phalloplasty with a short pedicle. Very short pedicles do not pose any decisional dilemma, because obviously such pedicles will not reach far enough for adequate tissue transfer. Sometimes the pedicle is just long enough to reach the femoral vessels (or one of its side branches) for a free flap reconstruction or the recipient site in the pubic area for a pedicled flap. In those cases a little tension may cause vascular occlusion and subsequent revision for vascular insufficiency. If there is any doubt, we advocate taking one of the measures that will be described instead of waiting for the problem to occur and needing to do a revision. If a pedicled (ALT) flap phalloplasty has a short pedicle, the surgeon should convert it to a free flap without hesitation. Postoperative swelling can only worsen a borderline scenario. If the pedicle is still too short, adequate measures should be taken as will be described for free flaps. To prevent this unlucky scenario in an ALT flap phalloplasty, we always perform an angiographic CT scan preoperatively4 to identify the best thigh and pedicle both in diameter and distance from the groin area. Thus the need to use a short or small-sized pedicle can be avoided. Perforators located less than 20 cm below the anterior superior iliac spine are at risk of being too short. In an RFF phalloplasty, pedicle shortness is a problem that normally only affects the arterial side. In the dissection of an RFF, the cephalic vein is harvested until after the confluence between the superficial and deep venous systems, resulting in a draining vein that is always longer than the artery. Furthermore, on the venous recipient side, many long veins can always be found. If this is not the case, the great saphenous vein can always be harvested to a sufficient distal length and then divided and transposed cranially to allow a safe, large-caliber, and tension-free venous anastomosis. The drawback is that a longer vein is more prone to kinking if not appropriately positioned. The surgeon should always double check vein position before closing. If the saphenous vein is used, positioning of a coupler may be difficult. The saphenous vein tends to be thick walled and not easy to bend over the circular ring of the coupler. A short arterial pedicle will not reach the femoral artery (common or superficial) and its branches below the inguinal ligament, which are sometimes too small to allow a safe anastomosis. If this is the case, two options are available: arterial transposition or arterial interposition graft. If the gap to be filled is less than 4 cm (pedicle to femoral vessels), the deep inferior epigastric artery (DIEA) can be identified and used for vascular anastomosis. In this situation DIEA vessels can be harvested either through an extension of the existing groin incision (Fig. 13-1) or an extended Pfannenstiel incision (Fig. 13-2). The superior adipocutaneous flap is raised as needed with cephalad traction, and an incision is made just medial to the lateral border of the rectus abdominis muscle. The anterior rectus sheath fascia is incised, and the deep inferior epigastric vessels are isolated from the posterior rectus sheath posteriorly and the rectus muscle anteriorly. The artery and venae comitantes are harvested cranially until the desired length is reached; the surgeon must be careful to preserve the motor intercostal nerve branches. The vessels are then divided distally and transposed to the recipient site through the opening in the fascia (Fig. 13-3) that will be sutured completely except for a hole for the vessels. Although the artery maintains an adequate caliber, the veins may be so small that the discrepancy with the flap’s vein is too big. In this latter case the transposed saphenous vein or one of its branches can be used for outflow (see Fig. 13-2). After the desired length of the pedicle is obtained, the artery is ligated, divided, and transposed caudally. Letting the artery come out of the abdominal wall from the lowest point of the fascial incision usually allows sufficient length to almost reach the pubis. Tunneling the pedicle underneath the inguinal ligament to bring it below provides additional length but at the expense of a longer, deeper, and more complicated dissection. This is almost never necessary, because extending the dissection cranially is usually easier and as effective; this is because the inferior epigastric vessels do not reduce much in their caliber in their course underneath the rectus abdominis muscle. Furthermore, the proximal part of the artery lying underneath the ligament is rather tortuous, whereas the distal part underneath the rectus muscle is straight and easier to position. When closing the abdomen, the surgeon should carefully reapproximate the two layers of fascia that are encountered without arterial compression. Some surgeons reinforce the anterior rectus sheath with a mesh graft to avoid a postoperative bulge. However, preservation of the intercostal motor branches and careful reapproximation of the fascial layers prevent any bulging. Fig. 13-1 The DIEA and venae comitantes (green backgrounds) are isolated through the prolonged groin incision. A microvascular clamp is placed on the vessels before division. Fig. 13-2 The deep inferior epigastric artery and vein are tunneled into the defect after an extended Pfannenstiel incision is used to harvest the vessels. Two saphenous veins as outflow vessels, the left ilioinguinal nerve, and the denuded clitoris are also shown. Fig. 13-3 The transposed DIEA and venae comitantes almost reach the recipient site. It is not always necessary to take such a long stump. The shorter the stump, the bigger the caliber. Fig. 13-4 The left descending branch of the lateral circumflex femoral artery is dissected and tunneled in the defect for recipient vessels when inferior epigastric arteries were not useful and femoral arteries had extensive scarring. An alternative to arterial transposition can be an arterial interposition graft. An arterial (and venous) interposition graft can be harvested from the deep inferior epigastric vessels as previously described or from the DIEA/descending branch of the lateral circumflex femoral artery, which is the ALT flap pedicle, accessed through an incision at the septum between the vastus lateralis and rectus femoris muscles and deepened until the pedicle is encountered lying on the medial edge of the vastus lateralis (Fig. 13-4). As long as the motor nerve to the vastus lateralis is spared, this donor site provides easy access to a very long graft with no functional loss and through a linear scar in a thigh that is usually already scarred to harvest either an ALT flap and/or a split-thickness skin graft used to cover the ALT or RFF donor site. In ALT phalloplasties the graft can be harvested from the vessels distal to the perforator or from the contralateral thigh. We prefer to avoid a vein-to-artery graft. An artery-to-artery graft preserves a more physiological situation, better tolerates high-pressure regimens, and maintains the pulsatile flow. Immediate arterial thrombosis is a very rare event, but it can sometimes complicate a phalloplasty procedure intraoperatively or (very) shortly after surgery. These early arterial thrombi are normally white and easy to remove. The problem with this complication is not only that the anastomosis (either end-to-end on a side branch or end-to-side on the femoral artery) must be redone, but there is not too much room for vessel shortening in the first case or for a change in anastomotic site in the second case. When a thrombosis occurs at an end-to-side anastomosis, the surgeon should preferably not remove the anastomosis and close the femoral artery, because leakages or breakdowns may occur. The flap’s artery is normally divided while leaving the stump (ligated or clipped) attached to the femoral vessels. A new recipient vessel must be found, eventually requiring an arterial interposition as previously described for short pedicled flaps. In this case the inferior epigastric artery is an excellent choice for a recipient artery. If the thrombosis is not explained by a technical mistake, thromboprophylaxis is started with a bolus of an antiplatelet drug (dipyridamole, lysine salicylate, and piracetam) at the completion of the arterial anastomosis before clamp release. Antiaggregation is continued postoperatively as a continuous infusion for 24 hours and then orally for 7 days. This regimen is only used in patients with an otherwise unexplained arterial thrombosis. Alternatively, low-molecular-weight heparin and aspirin—discontinuing heparin on discharge and aspirin after 1 month—can be used. Although rare, an arteriovenous fistula that causes a steal phenomenon to the flap may exist between the radial artery and venae comitantes. In these cases the anastomoses are patent, there is venous return in the vein, and the flap is pale; there is neither bleeding nor capillary refill. The clue to diagnosis is a pedicle that is well pulsatile until a certain point with venous return through the flap’s vein (this latter case rules out a pedicle thrombosis). On suspicion the pedicle is examined starting from the anastomosis and carefully isolating the artery from the vein until the communication is found and ligated or clipped. Sometimes there can be multiple shunts. In these latter cases the flow will progress a little further and then stop again. After all the fistulas are closed, the flap will again be well perfused. If the subcutaneous fatty layer in the forearm or thigh is too thick (or the dimensions of the flap are not designed large enough), closure under tension, which is often combined with postoperative swelling, can cause a compartment syndrome within the flap, jeopardizing vascularization of the urethra, the outer flap, or both. Every time tension is observed, the flap should not be sutured to itself but left open in its ventral part and the residual defect grafted. This is often required only in the proximal two thirds of the flap, but if any doubt exists, it is safer to place a small skin graft over the complete ventral side of the flap (which will not be visible long-term) rather than risking partial flap necrosis. The same applies to revisions for venous congestion, hematomas, or intraflap arteriovenous loops (Fig. 13-5), which result in additional flap congestion and increased swelling. In these cases the cylinder of the penis should not be closed but left open and grafted.
Unfavorable Results and Complications in Phalloplasty Surgery
Key Points
 Prevention and treatment of complications and failures of a phalloplasty are discussed.
Prevention and treatment of complications and failures of a phalloplasty are discussed.
 Failure to achieve the goals of correct penile reconstruction despite a “successful operation” is also discussed. Sometimes these cases require a redo.
Failure to achieve the goals of correct penile reconstruction despite a “successful operation” is also discussed. Sometimes these cases require a redo.
 Immediate or perioperative complications are a short pedicle, arterial thrombosis, arteriovenous shunts (radial forearm flap), and tight closure.
Immediate or perioperative complications are a short pedicle, arterial thrombosis, arteriovenous shunts (radial forearm flap), and tight closure.
 Early complications include insufficient venous outflow in patients with a free radial forearm flap, vascular insufficiency, partial necrosis, and a fistula.
Early complications include insufficient venous outflow in patients with a free radial forearm flap, vascular insufficiency, partial necrosis, and a fistula.
 Delayed complications include strictures.
Delayed complications include strictures.
 Late complications are atrophy, dyspareunia, erectile implant exposure, an unaesthetic donor-site scar, and compression neuropathy.
Late complications are atrophy, dyspareunia, erectile implant exposure, an unaesthetic donor-site scar, and compression neuropathy.
 In cases of shriveled or incomplete phalloplasty, redos must be considered.
In cases of shriveled or incomplete phalloplasty, redos must be considered.
 Decrease the individual’s gender dysphoria
Decrease the individual’s gender dysphoria
 Avoid the need for a prosthesis for penetrative vaginal or anal penetration, thus allowing sexual intercourse with the construction
Avoid the need for a prosthesis for penetrative vaginal or anal penetration, thus allowing sexual intercourse with the construction
 Have the ability to achieve orgasm during the sexual experience
Have the ability to achieve orgasm during the sexual experience
 Allow voiding while standing
Allow voiding while standing
 Have tactile and erogenous sensation
Have tactile and erogenous sensation
 Have a normal-looking scrotum and be aesthetically pleasing
Have a normal-looking scrotum and be aesthetically pleasing
 Cause little morbidity and scars at the donor site
Cause little morbidity and scars at the donor site
Immediate or Perioperative Complications
Short Pedicle
Arterial Transposition (Deep Inferior Epigastric Artery)
Arterial Interposition Graft (Deep Inferior Epigastric Artery/Descending Branch of the Lateral Circumflex Femoral Artery)
Arterial Thrombosis
Arteriovenous Shunts (Radial Forearm Flap)
Tight Closure
Abdominal Key
Fastest Abdominal Insight Engine