CHAPTER 115 Ulcers of the Small and Large Intestine
ISOLATED ULCERS
NONSPECIFIC OR IDIOPATHIC SMALL INTESTINAL ULCERATION
Solitary ulcers of the small intestine result from a wide variety of causes (Table 115-1). Radiation injury is a known cause of small intestinal ulceration and is discussed in Chapter 39. Solitary ulcers beyond the duodenum that cannot be explained on the basis of any known etiology are referred to as nonspecific or idiopathic intestinal ulcers. Such solitary nonspecific ulcers are rare, with an incidence of 4 per 100,000.1
Table 115-1 Causes of Small Intestinal Ulceration
Clinical Features
In a review of the Mayo Clinic’s experience with 59 cases of small intestinal ulcers over a 22-year period ending in 1979, Boydstun and associates1 showed that 53 (89.8%) patients had no identifiable cause of ulceration. Patients ranged in age from 17 to 77 years, with most presenting in the fifth and sixth decades of life; no gender predominance was found. The most common presenting symptom was intermittent small bowel obstruction (63%). Physical findings ranged from nonspecific abdominal tenderness and distention to an acute abdomen resulting from intestinal perforation. Laboratory evaluation was notable only for anemia in one half of the patients. Radiologic studies localized the ulcer in a minority of patients.
Pathology
In the Mayo Clinic series,1 the ileum was the most common location of nonspecific ulceration (78%), and perforation (13 cases, 22%) occurred most commonly in the jejunum (78%). At surgery, 41 patients were found to have solitary ulcers, five patients had two ulcers, and six patients had more than three ulcers. Ulcer size varied between 0.3 and 5 cm. On pathologic examination, the ulcers were predominantly on the antimesenteric border of the small intestine and, in some cases, were associated with a fibrous scar that narrowed the lumen. Microscopy revealed nonspecific chronic inflammation that ended abruptly at the ulcer edge. The intervening bowel and vasculature were normal.1
SOLITARY RECTAL ULCER SYNDROME
Solitary rectal ulcer syndrome (SRUS) is an uncommon or under-reported disorder of defecation that affects patients of all ages. The term is a misnomer: Patients can present with hyperemic mucosa only, a solitary ulcer, multiple ulcers, or even a polypoid lesion resembling carcinoma.2 Regardless, the histology of SRUS is typical, showing fibromuscular obliteration of the lamina propria and smooth muscle fibers extending from a hypertrophied muscularis mucosa to the lumen.2 The diagnosis of SRUS often is delayed because of its varied endoscopic appearance and a lack of awareness of the disorder.
Pathogenesis
SRUS is a disorder of defecation, but its pathogenesis is uncertain, and it has a spectrum of disease presentations. A large subgroup of patients with SRUS strain excessively during defecation, and some have a behavioral disorder. Occult or overt rectal prolapse with paradoxical contraction of the pelvic floor during defecation appears to be involved in most patients3; evidence of inappropriate pelvic floor contraction has been shown in electromyographic and video-proctographic studies.3 It has been suggested that the rectal mucosa can be traumatized from the pressure of being prolapsed against a closed anal canal4 and that straining during defecation results in prolapse and high fecal voiding pressures that reduce local blood flow, causing ischemia and ulceration.4 The mucosa of the anterior rectal wall, 7 to 10 cm above the anal verge, is the most common area of such prolapse into the anal canal, and this corresponds to the usual location of ulceration in SRUS.
SRUS also has been associated with the use of ergotamine suppositories and is well known after radiotherapy, further supporting a pathogenic role for ischemia.5,6 Successful treatment of SRUS using biofeedback has been associated with an increase in local blood flow, additionally suggesting that SRUS may be associated with reduced rectal blood flow from impaired extrinsic autonomic cholinergic nerve activity.7
The association of SRUS and rectal prolapse, however, is neither pathogenically clear nor universal; the incidence of associated rectal prolapse varies from 13% to 94%.2 It is assumed that the ulcer develops as a result of local trauma to the apex of the prolapse, either because of manual attempts to reduce the prolapse digitally or because of contractions of the external anal sphincter when the mucosa prolapses through the anal canal.4
Du Boulay and colleagues have shown that the histology of the rectal mucosa in patients with SRUS is similar to that seen at other sites of mucosal prolapse, suggesting that prolapse of the mucosa alone rather than the entire rectal wall is important in SRUS pathogenesis.8 Ischemia results in fibromuscular obliteration of the lamina propria and the formation of an ulcer. Once the ulcer is formed, it can further intensify the urge to defecate; this urge combined with straining and changes in local blood flow causes persistent symptoms and chronic ulceration.
Clinical Features
Patients with SRUS present with varied symptoms, but most patients typically complain of passage of mucus and blood per rectum on defecation.9,10 Some patients also complain of tenesmus, straining, altered bowel habits, and the sensation of incomplete evacuation. Men and women are affected equally, and they usually present in the third and fourth decades, respectively.11 The mean duration of symptoms is long, ranging from 3.5 to 5 years, possibly reflecting a delay in diagnosis.
Diagnosis and Pathology
Diagnosis of SRUS is based on clinical symptoms, physical examination, endoscopic findings, and typical histology. Physical examination can demonstrate tenderness in the left lower quadrant. On digital rectal examination, there may be reduced anal sphincter tone and an indurated area, or thickened folds may be palpated.12 Overt rectal prolapse may be demonstrated by having the patient assume a squatting position and straining as if to have a bowel movement. Sigmoidoscopy may demonstrate single or multiple ulcers or a patch of erythematous mucosa on the anterior rectal wall within 10 cm of the anal verge. The lesion has a polypoid appearance (Fig. 115-1) in 25% to 44% of patients.2,12 Differential diagnosis includes inflammatory bowel disease, malignancy, ischemic colitis, stercoral ulcer, medication-induced ulceration, trauma, and infections, including amebiasis and secondary syphilis.11
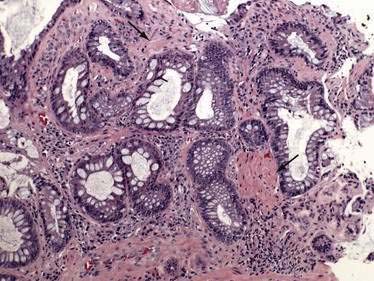
Biopsy specimens always should be taken from the ulcer margin and from any abnormal-appearing mucosa. In 1969, Madigan and Morson9 first described the histologic features of SRUS. There is fibromuscular obliteration of the lamina propria by collagen from fibroblasts and smooth muscle fibers derived from the muscularis mucosae. The muscularis mucosae is often hypertrophied, and its fibers are in continuity with those in the lamina propria. There is no significant increase in the number of inflammatory cells. The polypoid variant is similar to the ulcerative variant except for regenerative hyperplastic changes, such as cystic dilatation and mucus cell production.11 Epithelial elements and lamina propria can be displaced into the submucosa (Fig. 115-2). This displaced tissue can then undergo cystic dilatation because of mucus retention. The misplaced and dysplastic-appearing glands may be misdiagnosed as adenocarcinoma, especially when the histologic and macroscopic features of SRUS are not recognized; at times SRUS is present in association with an carcinoma, further confusing the issue.
Histology typically provides a definitive diagnosis; however, defecography may be useful to shed light on the pathophysiology of SRUS, especially if surgery is being considered. Defecography may be used to demonstrate mucosal prolapse, intussusception, rectal prolapse, a nonrelaxing puborectalis muscle, and incomplete or delayed evacuation.11 Endorectal ultrasound can demonstrate the presence and components of rectal wall thickening, particularly the muscularis propria, and may be useful to distinguish SRUS from other conditions such as invasive cancer.11
Treatment
Asymptomatic patients might not require any treatment, and in some patients, SRUS resolves spontaneously. Treatment includes improving bowel habits; consuming a high-fiber diet; using bulk laxatives, local agents, and biofeedback; and undergoing surgery. The addition of fiber as a bulking agent along with bowel habit training to reduce straining can improve symptoms in patients with mild disease. Local agents such as topical glucocorticoids and aminosalicylates are not effective. Sucralfate enemas and human fibrin sealant have been effective in small studies.13 Argon plasma coagulation (APC) has been used to treat hemorrhage from SRUS; continued treatment with APC has been associated with symptomatic and endoscopic improvement.14
Behavioral therapy or biofeedback is the first line of therapy for those with more-severe disease, and it improves symptoms in more than 50% of patients; ulcer healing, however, is seen in a minority of patients. Behavioral therapy aims at bowel habit training with normalization of pelvic floor coordination. Jarrett and associates demonstrated that biofeedback resulted in improved rectal blood flow, which was associated with a successful clinical outcome.7
Surgery is indicated in symptomatic patients who have severe disease and who do not respond to medical or biofeedback therapy, but the best surgical option depends upon the underlying anatomic pathology, and every patient must be assessed individually.15 Surgical procedures include excision of the ulcer, low anterior resection, colostomy, or anterior resection with rectopexy.10 It is difficult to compare surgical treatments for SRUS because of the small number of patients in surgical series and the variety of anatomic pathology that underlies SRUS.10
STERCORAL ULCERS OF THE COLON
Stercoral ulcers result from pressure necrosis of the mucosa caused by the direct effect of a hard fecal mass (scybalum). Over time, the pressure of the scybalum results in local ischemic necrosis and ulceration and can eventuate in perforation. These ulcers are rare and usually asymptomatic until they manifest with lower gastrointestinal bleeding or colonic perforation. Fecal disimpaction occasionally precipitates rectal hemorrhage when the scybalum is removed, along with an adherent blood vessel in the subjacent ulcer crater. Maurer and coworkers observed that 3.2% of colonic perforations in their series were caused by stercoral ulcers.16
Chronic constipation is the major risk factor for stercoral ulceration and, although described in patients of all ages, it is more common among elderly patients with clinical features that may be associated with constipation.17 Although constipation and fecal impaction are observed commonly, complications of stercoral ulceration are relatively uncommon. Serpell and Nicholls reviewed 64 cases of stercoral perforation of the colon. The median age of these patients was 60 years, and 23% of them were nursing home residents. Factors that increase constipation and formation of a scybalum, such as antacids containing aluminum hydroxide, use of narcotic analgesics, constipating sedatives and psychiatric medications, and chronic renal failure, were observed in patients who developed stercoral ulceration.18 Why a stercoral ulcer develops is unclear, although implicated factors predisposing the left colon to ulceration include dehydrated and hard feces, a narrow-diameter colon with high pressure, and relatively poor blood supply.
Patients with perforated ulcers usually present with peritonitis and findings of an acute abdomen.18 The scybalum sometimes is palpable as an abdominal mass. Plain films of the abdomen might demonstrate pneumoperitoneum, fecal loading, or calcified scybala. Nonperforating ulcers can manifest with lower gastrointestinal bleeding. Caution must be used in performing disimpaction in patients with hard fecal masses in the rectum, because removing the mass can result in severe hemorrhage if the underlying blood vessel in the ulcer base is torn during removal.
The antimesenteric border of the colon is most commonly involved, usually in the sigmoid or proximal rectum. Ulcers usually are large, irregular, and sharply demarcated, and they may be single or multiple. Ulcers conform to the contour of the impacted scybala and result from ischemic pressure necrosis. A rounded or ovoid perforation may be seen in the center of the ulcer. Necrotic colonic mucosa with acute and chronic inflammation is noted on histology.17 Differential diagnosis includes spontaneous colonic perforation, malignancy, ischemia, and infection.
Perforated stercoral ulcers require emergency laparotomy with resection of the affected colonic segment. A Hartmann’s operation is the preferred procedure, and along with extensive peritoneal lavage, it is associated with a lower mortality than other surgical procedures.16,18 Nonperforating stercoral ulcers might respond to antibiotics and aggressive treatment of constipation, although surgical resection remains the only definitive treatment.
ULCERATION INDUCED BY NONSTEROIDAL ANTI-INFLAMMATORY DRUGS
NSAIDs are among the most frequently administered drugs in the world, and their adverse side effects involve not only the stomach and duodenum but also the distal portions of the small intestine and colon. Gastroduodenal risks of NSAIDs are well known, but lower gastrointestinal tract risks of NSAIDs occur with similar frequency.19,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree