Stage
Characteristic
Stage 0
Cervical intraepithelial neoplasia (CIN 3)
Stage I
Confined to cervix
IA
Invasive carcinoma only diagnosed by microscopy
IA1
Stromal invasion <3 mm in depth and <7 mm in extension
IA2
Stromal invasion >3 mm depth and not >5 mm and extension <7 mm
IB
Visible lesions limited to the cervix or preclinical cancers >stage 1A
IB1
Clinically visible tumor ⩽4 cm in greatest dimension
IB2
Clinically visible tumor >4 cm in greatest dimension
Stage II
Beyond cervix though not to pelvic sidewall or lower third of vagina
IIA
With upper vaginal but without parametrial invasion
IIA1
Clinically visible tumor ⩽4 cm in greatest dimension
IIA2
Clinically visible tumor >4 cm in greatest dimension
IIB
With parametrial invasion
Stage III
Lower vaginal or pelvic sidewall spread
IIIA
Tumor involves lower third of the vagina with no extension to pelvic sidewall
IIIB
Extension to pelvic sidewall or causing obstructive uropathy
Stage IV
Extension beyond pelvis or biopsy proven to involve the mucosa of the bladder or the rectum
IVA
Extension beyond pelvis or rectal/bladder invasion
IVB
Distant organ spread
Staging
All cancers are staged in the same way if they are believed to be primary cervical cancer. The International Federation of Gynecology and Obstetrics (FIGO) system for staging is most widely used but does not include lymph node status [1]. It is primarily a clinical and pathologic system. The 2009 revision of FIGO staging (Table 1) made the concession that information from crosssectional imaging should be recorded [1].
The American Joint Committee on Cancer (AJCC) TNM staging scheme works as for most other cancers. Stages T1-T4 are similar to FIGO stages I-IVa, but it includes additional nodal (N) and distant spread (M) staging categories [2].
MRI Technique and Pearls for Cervical Cancer Staging
The imaging mainstay is T2-weighted imaging (T2-WI), comprising a sagittal sequence of the pelvis and a small field of view (SFOV) inclined axial sequence perpendicular to the endocervical canal (Fig. 1). In some cases, imaging along the plane of the endocervical canal better depicts lateral extension of the tumor. In the normal cervix, a low signal intensity (SI) stromal ring surrounds high SI mucosa. Tumors in premenopausal women are more commonly exophytic, filling the vagina. In postmenopausal (PM) women, they are more commonly endophytic within the barrel of the cervix.
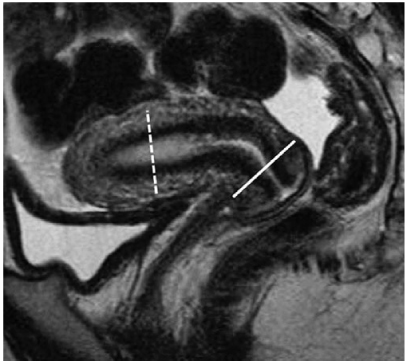
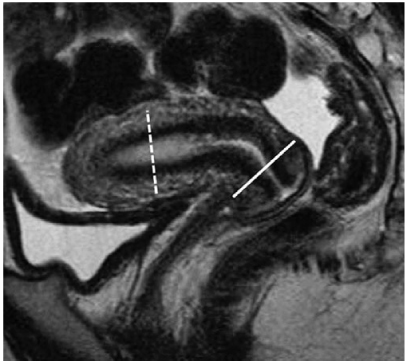
Fig. 1
Sagittal T2-weighted image of the normal uterus showing zonal anatomy and planes used for small field-of-view imaging of cervical cancer (solid white line) and endometrial cancer (dashed white line)
Stage I
Stage IA tumors are usually completely excised in the diagnostic biopsy. MRI shows only features of this artefact. Stage IB tumors have brighter T2-W SI than the dark, fibromuscular, cervical stroma. The key imaging sign of stage IB disease is preservation of a continuous intact low T2-W SI stromal ring of the cervix around the tumor [3].
Stage II
Stage IIB tumors interrupt or breach this “black ring” and may extend into the surrounding parametrial fat (Fig. 2). Stage IIA tumors invade the low T2-W SI wall of the upper vagina but do not breach this black ring.
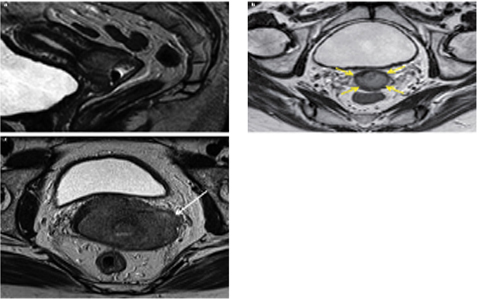
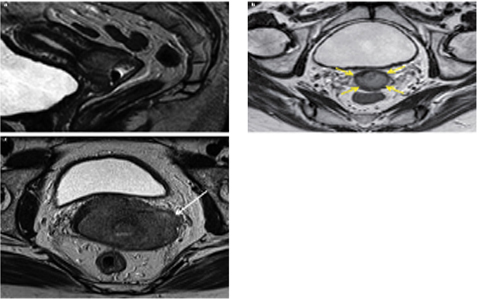
Fig. 2 a–c
a Sagittal T2-weighted image of stage IB cervical cancer with b corresponding inclined small field-of-view image showing an intact and complete T2 dark stromal ring (yellow arrows) and c a different and large stage IIB cancer with breach of the left side of the stromal ring and parametrial invasion (white arrow)
Stage III
Stage IIIA tumors invade the lower vagina, and this involvement may be better appreciated clinically. Stage IIIB tumors extend within 3 mm of or show abutment with the low-SI internal obturator, levator ani, and pyriform muscles and the iliac vessels, or show ureteric involvement with a hydroureter above this level.
Stage IV
Stage IVA tumors show loss or interruption of the low-SI bladder or rectal wall, and tumor invading through the mucosa is diagnostic. Bladder bullous edema alone does not qualify stage IVA disease (Fig. 3a).
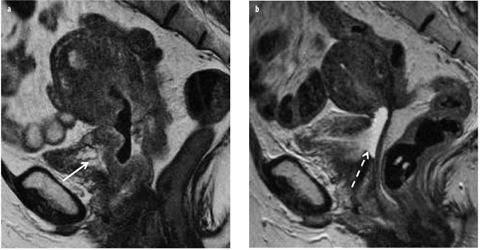
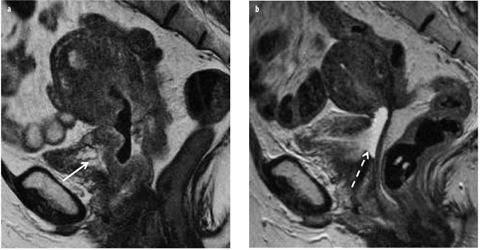
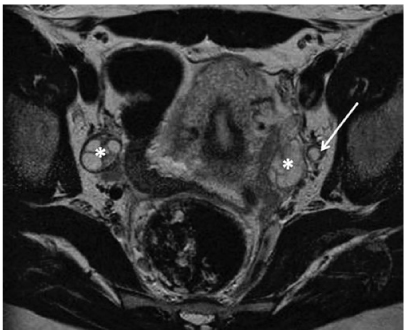
Fig. 3 a, b
a Sagittal T2-weighted image of a large stage II cervical cancer invading the upper vagina and outer wall of the bladder. Note the presence of bullous edema of the bladder (solid arrow) but no frank invasion of the lumen; b development of a vesicovaginal fistula postchemoradiation therapy (dashed arrow)
Alternative Imaging Sequences
Alternative sequences that may be used include diffusionweighted imaging (DWI) and dynamic contrast-enhanced (DCE) MRI. There is no consensus as to which other sequences should be used for staging pelvic lymph node metastasis and other abdominal spread, suffice to say that they should cover the pelvis and abdomen up to the renal hila and employ at least two orthogonal planes and both T1-W and T2-W images. A pelvic lymph node >9 mm in maximum small-axis dimension (MSAD) is concerning due to pelvic nodal metastasis [4], as is any lymph node showing necrosis (Fig. 4). Smaller nodes seen in the parametrium or the rectal envelope are concerning for metastasis. Examinations performed to assess treatment response should aim for reproducibility with earlier MRI studies. Examinations performed for suspected treatment complications should be tailored to the specific concern.