Transperineal
Guillermo Rosato
Pablo E. Piccinini
Criteria of patient selection for surgery:
Rectocele ≤4 cm in diameter as measured during defecography (DFG) or ≤2.5 cm as measured during pelvic floor dynamic magnetic resonance (DMRPP) imaging.
Non- or partial emptying of rectocele during the push phase in other DFG or DMRPP.
Rectal and/or vaginal symptoms for longer than 12 months.
3 + for at least 4 weeks despite dietary fiber of 30 g/day.
Rectal and/or vaginal digitation required to facilitate rectal evacuation.
Patient election for surgery has followed the previously mentioned selection criteria of anorectal physiology including transit time, anal manometry, DFG, DMRPP, and neurophysiology of the pelvic floor.
All patients underwent bowel preparation with 3,000 cc polyethylene glycol or a phospho-soda solution. Antibiotic prophylaxis consisted of a combination of Metronidazole and Gentamycin or Ceftriaxone.
Positioning
The patients were placed in the prone jackknife position.
Technique
Anesthesia was at the patient’s choice either spinal or general.
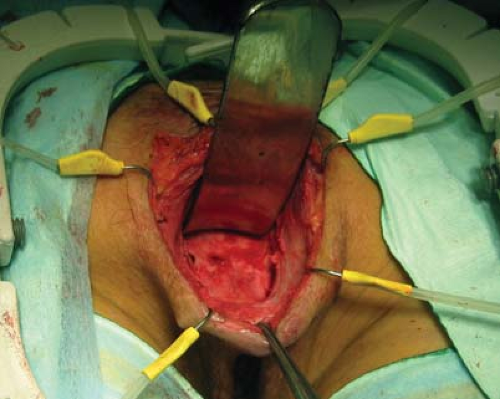
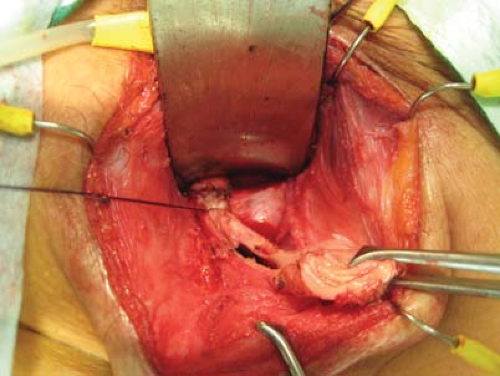
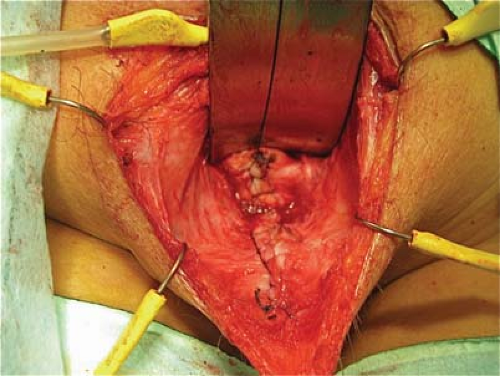
The surgical technique was a perineal approach, through a U-shaped incision (Figs. 24.1 and 24.2). Dissection was undertaken in a cephalad direction to reach the vaginal cupola (Fig. 24.3) after which trapezoid strip of posterior redundant vaginal wall was resected (Fig. 24.4). The posterior vaginal wall was closed by a running suture of 3-0 Polyglactin 910 (Fig. 24.5) including closure of the dead spaces between the rectal and the vaginal walls (Fig. 24.6). A levator plication was undertaken by placing two single stitches of 2-0 Prolene. A perineoplasty was performed on an individual basis to prevent bulging of the perineal body during push (Fig. 24.6). Ultimately the skin was fully closed, without drainage (Fig. 24.7).
Combined procedures for hemorrhoidectomy and/or fissure were undertaken at the same time of surgery.
Patients were usually discharged on day 2 although oral antibiotics were continued for 5 postoperative days. Initially intravenous analgesia was delivered (50 mg of Diclofenac each 8 hours) after which oral analgesia was used and was maintained on demand after hospital discharge.
Clear fluids were started on the first postoperative day. On day 2, a normal diet plus psyllium supplement was begun. Imaging control at 4 months postoperation was undertaken to verify surgical results.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree