House Flap Anoplasty for Bowen’s Disease
Jorge A. Lagares-Garcia
Paul R. Sturrock
Current terminology and definition of premalignant lesions of the anus and perineum are confusing. The same pathology can be defined with the terms squamous cell carcinoma in situ, anal intraepithelial neoplasia (AIN), anal dysplasia, squamous intraepithelial lesion, or Bowen’s disease. Unfortunately, there seems to be a significant discrepancy between the staging systems and intra- and interobserver variability. Moreover, increasing screening techniques have shown that detection of high-grade squamous intraepithelial lesions (HSILs) or AIN III has increased, but they have not decreased the incidence of invasive cancer in high prevalence areas of AIN. This fact is more significant in patients who practice anoreceptive intercourse, specifically those suffering from HIV.
Human papilloma virus is a DNA papovavirus that causes the most common viral sexually transmitted disease. Serotypes 16, 18, 31, 33, and 35 are significant for harboring a higher malignant potential.
For all purposes in this chapter, both Bowen’s disease and squamous cell carcinoma in situ will be described as HSIL to avoid any confusion. The potential of invasion is much less when the pathology report reveals low-grade squamous intraepithelial neoplasia, therefore the most common indication to perform a “house flap” anoplasty (HA) is currently HSIL.
Other pathologies such as anal stricture, extensive tracts of hidradenitis suppurativa, and mucosal ectropion from prior anorectal surgery may be indications for the use of advancement flaps such the “house flap.”
T1 tumors (2.5 cm or less in diameter) may undergo local excision if no lymphadenopathy is noted during the preoperative metastatic evaluation. Coverage of the resulting defect may also be undertaken with this kind of skin and subcutaneous tissue flap.
The current indications for the use of HA are indicated in Table 34.1.
The width of the area to be excised can be quite large depending on the extent of the disease. It is important to note that the disease is multicentric due to the viral nature
and the localization of HSIL areas may not be totally reduced to one aspect of the intra-anal, perianal areas (<5 cm radius from the anal opening) or skin (>5 cm from the anal opening). For isolated processes such as stricture or ectropion the decision of laterality is made simpler.
and the localization of HSIL areas may not be totally reduced to one aspect of the intra-anal, perianal areas (<5 cm radius from the anal opening) or skin (>5 cm from the anal opening). For isolated processes such as stricture or ectropion the decision of laterality is made simpler.
Table 34.1 Indications for “House Flap Anoplasty” | ||
|---|---|---|
|
To plan for the area of excision and reconstruction, two different modalities may be used for locating the HSIL.
The use of an operative microscope or surgical loupes and an anoscope after the use of Lugol’s solution and acetic acid will reveal the lesions that may be biopsied, marked, or fulgurated.
Another method is the anal mapping technique where multiple biopsies are performed at the level of the dentate line, anal verge, and anal margin in 12 different sites that are labeled and sent to pathology for analysis. These results provide the clinician with a diagram of the areas of HSIL in the anal canal and surrounding tissues.
Once the area has been located, the decision is made whether to perform a unilateral or bilateral HA.
Positioning and Preparation
Multiple different opinions exist regarding the use of preoperative cathartic bowel preparation and postoperative bowel lock. Our current practice is to avoid a full-bowel preparation and instead to advise the patient to have two enemas the morning of the surgery. Patients must also remain nothing by mouth (NPO) for at least 6 hours prior to the induction of anesthesia.
The day of the procedure, the patient’s medical history is reviewed for allergies to drugs that may be used during the operation as well as to assess the current health status. The patient is brought into the operating room where graded compression stockings and sequential compression devices are placed for deep venous thrombosis prophylaxis. Antibiotic prophylaxis is given within 1 hour of making the incision. Our routine consists of either ciprofloxacin 400 mg IV + metronidazole 500 mg IV or cefoxitin 1–2 g IV + metronidazole 500 mg IV depending on the patient’s drug allergies. This same regimen is continued postoperatively for 24 hours.
While still on the transport stretcher, general endotracheal anesthesia is induced with the patient in the supine position and a foley catheter is then inserted. After the airway is secured, we proceed to transfer the patient onto the OR table in the prone jack-knife position over a Kraske pillow at the level of the iliac crests to obtain elevation of the buttocks. Separation of the buttocks and exposure of the anal region is achieved with tapes placed widely enough on the skin of the buttocks to provide retraction yet to allow access to the tissue being used for the reconstruction. After the skin is prepared with chlorhexidine or iodine-based solution, a wide preparation of the surgical field is undertaken with sterile drapes. It is our practice for the primary surgeon to routinely use a headlamp for better illumination of the operative field. In addition, if very delicate dissection of the anal canal is needed, the use of microscopic loupes (×2–3 magnification) may aid in visualization of the tissue planes.
Technique
After the perianal area is examined, a digital rectal examination is performed to palpate any abnormalities in the anal canal. This is followed by visual inspection of the anal canal using a Hill-Ferguson retractor. A decision is then made regarding the surface area to be excised. It is our preference to remove all macroscopic lesions in toto; we do not routinely perform intraoperative frozen sections to assess for microscopic margins, as this is very time consuming and does not alter our surgical approach.
It is important to note that at times, coexisting conditions such as fungal or bacterial superinfections exist. These maladies must be treated with antifungals or topical antibiotics prior to any procedure to minimize the risk of postoperative wound complications. Surgery should be deferred until such infections have been completely resolved.
If additional lesions exist in the vicinity or more lateral to the area to be excised, primary resection and closure in layers is recommended unless the defect is so large that it has to be encompassed with the resected area itself.
Measurements and Calculations
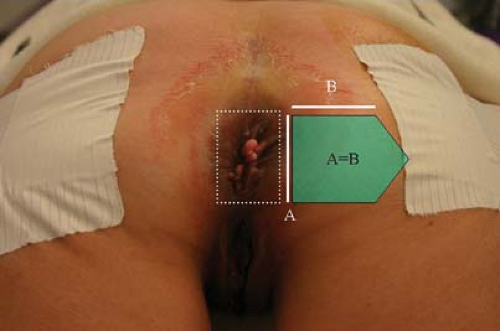
A quadrangular excision with clear margins from macroscopic lesions is drawn with indelible marker. The most lateral aspects will become the base of the HA. Our preference is to reconstruct the “side-wall” of the HA the same size as the base to avoid postoperative retraction making the advancements of the flap equidistant in all levels (Figs. 34.1




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree