Fig. 10.1
Pelvic exenteration
Differently to the classic VRAM flap, its variants — the de la Plaza, and Taylor flaps, with a skin island designed differently and higher on the RAM to DIEA — allow a wide arc of rotation, providing better orientation of the skin paddle in the perineal area and a greater share of muscle tissue, which offers tension-free reconstruction. This reduces the need to divide muscle fibers from the pubis insertion to reduce tension of the transposition, thus having the advantages of maintaining a muscle-point anchor to the reconstruction, which is also useful in terms of rehabilitation.
Perineal surgery with curative intent requires extensive excision of tissues with neoplastic involvement (Figs. 10.2 and 10.3), subsequently necessitating complex reconstruction, which must be planned considering the deficit of residual pelvic organ tissue [7, 8].
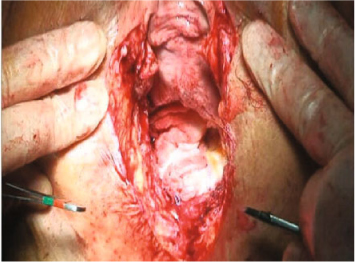
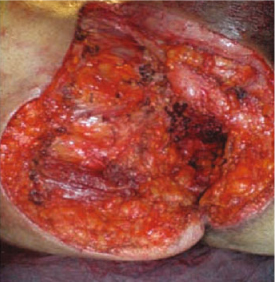
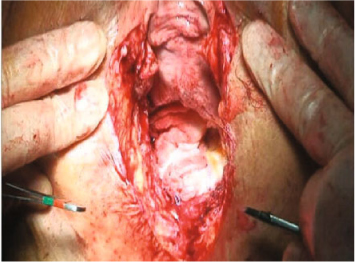
Fig. 10.2
Excision of neoplastic tissues extended to external genitalia and vagina
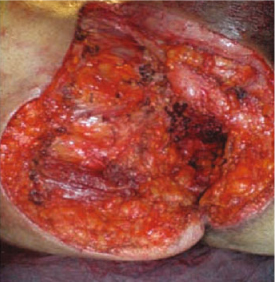
Fig. 10.3
Excision involving soft tissue at root of the thigh
The design of the cutaneous island on RAM to DIEA can vary in height, shape, and size, according to pelvic organs involved by the multiple possible locations of a centric pelvic recurrence and skin required to create flaps. It is extremely important to design an approach that provides cutaneous islands with extensions to cutaneous arteries.
It is also important to avoid prolonged and painful healing (Fig. 10.4), with failure of pelvic restraints and descent of the remaining pelvic organs—such as the bladder (Fig. 10.5) or intestinal loops in the perineal space. Such complications increase weight on the perineal skin, with subsequent pain and subocclusive crises for the numerous adhesions created in this area.



Fig. 10.4
Prolonged and painful healing

Fig. 10.5
Failure of pelvic restraint with descent of pelvic organs
The greatest risks to intra-abdominal perineal abscess—reduced vascularization and accumulation of secretions—is almost absent in reconstructions using a VRAM flap, as muscle tissue effectively performs the function of cleansing and lymphatic drainage of the perineal region [9–12]. The bilateral gluteus maximus musculocutaneous flap (Figs. 10.6–10.9) with plastic sliding V-Y is preferable in cases of neoplastic infiltration of the sacral bone, where it best fits the reconstructive needs following sacral resection with the patient in the prone position. Biological meshes are used in the donor site to strengthen large abdominal wall grafts or as integration and support when reconstructing the pelvic floor [13].


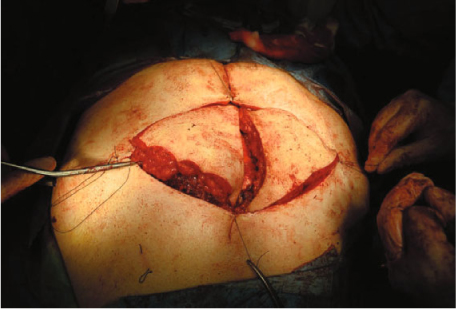


Fig. 10.6
Superior gluteal artery

Fig. 10.7
Bilateral gluteus maximus musculocutaneous flap
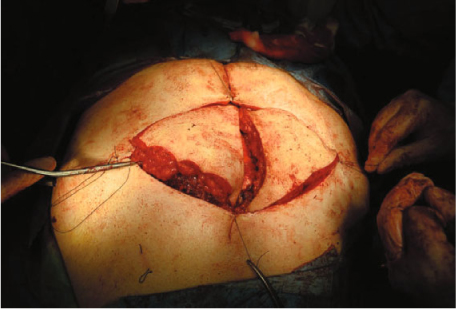
Fig. 10.8
Plastic sliding V-Y

Fig. 10.9
Final result
10.2 Regional Anatomy
The RAM flap is nourished by the DIEA. Constructing and applying the VRAM flap (Fig. 10.10), which is used in major reconstructive surgery, require extensive knowledge of the surface anatomy of the abdominal wall in order to avoid donor-site complications. Subcutaneous abdominal wall tissue consists of superficial and deep fat separated by surface fascia, composed of two layers: a superficial layer, barely visible, called Camper’s fascia; and a deep layer, much more evident, called Scarpa’s fascia. The RAM is long, thin, and flat, originating at the top front edge of the rib cartilage (5, 6, and 7) and xiphoid process and inserting at the bottom of the symphysis pubis. This anatomical condition is ideal for rotation to the pelvis. It has three tendon insertions — called tapeworms — that do not reach deep into the muscle, thus providing greater tensile strength and making it polygastric. The muscle is wrapped both anteriorly and posteriorly by a sheath created by merging the aponeurosis of the large abdominal muscles with those of the other side, forming the linea alba. The RAM has double vascularization type III according to Mathes and Nahai classification. The upper portion is fed by the deep superior epigastric artery (DSEA) and the lower portion by the DIEA. Along their entire course, these vessels emit perforating branches that cross the muscle belly, pierce fascia and fat, and nourish the skin.


Fig. 10.10
VRAM flap
10.3 Flap Design and Dimensions
A preoperative Doppler vascular ultrasound study of the DIEA and upper DSEA accurately identifies vascular pedicles and perforators, facilitating appropriate flap size and design (Figs. 10.11 and 10.12). A careful analysis must be performed to define abdominal wall characteristics (Fig. 10.12), which may be affected by previous surgery, muscle fascia diastasis, chest shape, adipose tissue thickness, and skin laxity. The headquarters of the bowel or urinary derivation will be determined in this design.



Fig. 10.11
Preoperative skin marking

Fig. 10.12
Preoperative surgical plan
Abundant skin islands, perfused by the DIEA, are taken at the top of the RAM flap according to the de la Plaza flap design. Skin tension in the final structure can be controlled with Z-plasty, as seen in Figs. 10.13 and 10.14. Perineal skin size, shape, and quality — especially after radiotherapy (Fig. 10.15) — are valid parameters for planning and creating the RAM to DIEA flap. The perineal deficit will be of variable shape and size but will never be <6 cm in diameter (Figs. 10.15 and 10.16). The skin paddle must be designed to correspond with the predetermined perineal deficit following APR; its height will be variable, according to the arc of rotation necessary, because the skin island and other flap components cross the perineal canal and cover the perineal deficit without tension or twisting on the vascular pedicle.



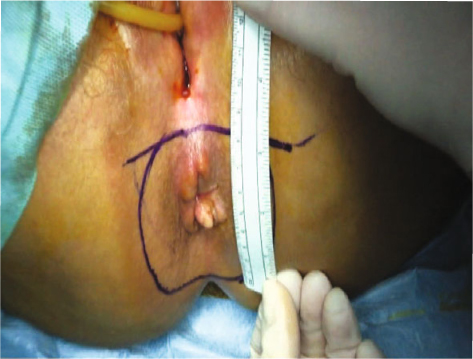

Fig. 10.13
Final tension-free suture of abdominal wall with Z-plasty (immediate postoperative view)

Fig. 10.14
Four weeks postoperative view

Fig. 10.15
Perineal deficit measurement
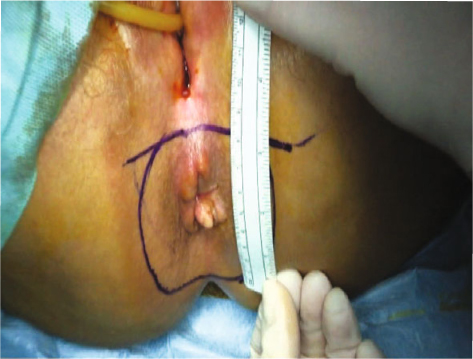
Fig. 10.16
Perineal deficit measurement
The VRAM flap requires a long and narrow dissection from the front fascia to incorporate the perforators, greatly facilitating the reconstruction phase of the abdominal wall without using biological mesh. The blood supply is guaranteed by numerous vessels perfusing the cutaneous island. The skin paddle, taken from above and below the navel, lies completely over the muscle. The VRAM is designed in classic manner and has the disadvantage of a limited arc of rotation for transposition to the perineal region and is therefore ill-suited to reconstructive initiatives following APR.
Removing a skin island vertically higher for a RAM than for a classic VRAM (Fig. 10.17) allows flap transposition without placing tension on its components due to the longer muscle pedicle (Figs. 10.18–10.21). The skin island can be planned in the upper portion of the RAM to DIEA thanks to the De La Plaza flap design, also called “flap to flag” due to its shape once created, which can be round or triangular. Arterial circulation in this flap is optimal due to its rich vascular communication via at least two groups of perforators originating in the DSEA. Also, donor skin quality is better than that of other programmable RAM to DIEA flaps.
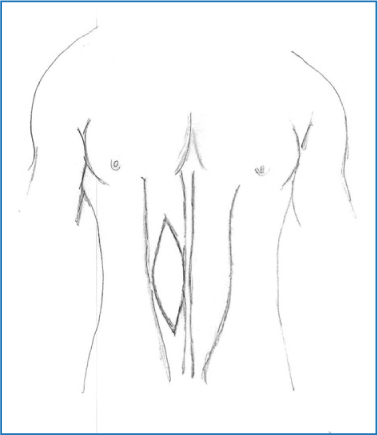
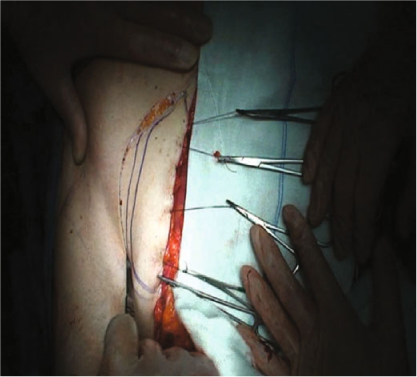
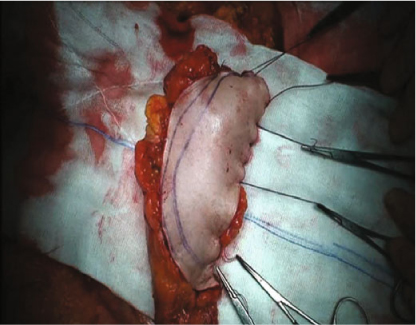


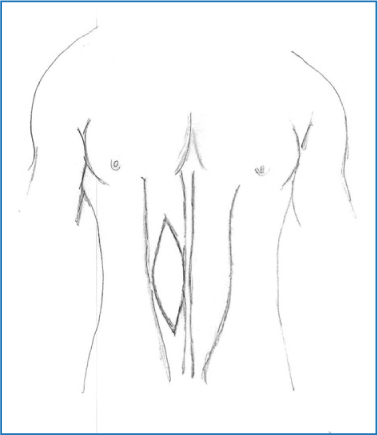
Fig. 10.17
VRAM flap with skin island classic technique
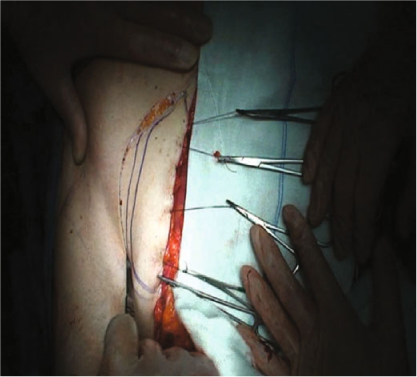
Fig. 10.18
VRAM flap harvesting
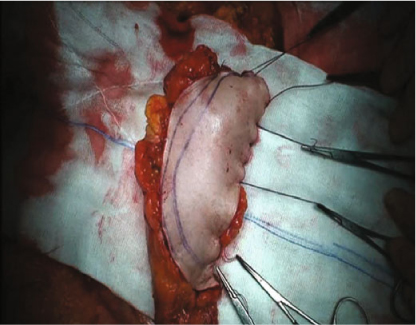
Fig. 10.19
VRAM flap with DSEA pedicle switched off

Fig. 10.20
VRAM flap inset in vaginal defect

Fig. 10.21
Postoperative view
The muscle pedicle is detached from the skin to provide a surface at least 4–5 cm larger than that of the classic VRAM flap. Compared with the VRAM flap, the De La Plaza flap easily adapts to the shape of the deficit in the perineal region after APR (Fig. 10.22). Creating a wide skin shell is necessary in the case of the large skin deficit at the root of the thigh (Fig. 10.23), with a muscular component free from skin that allows tension-free occupation of the perineal channel. The 180° rotational arc, facilitated by the flag shape, provides a large margin for orienting the skin island in the perineal zone, allowing a perfect fit into the deficit (Figs. 10.23–10.26).
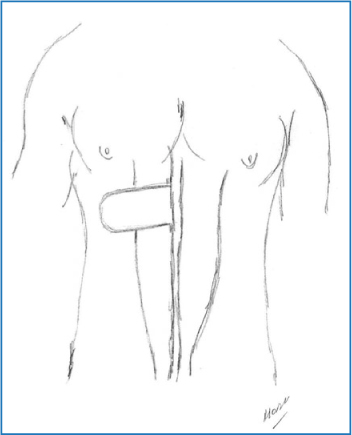

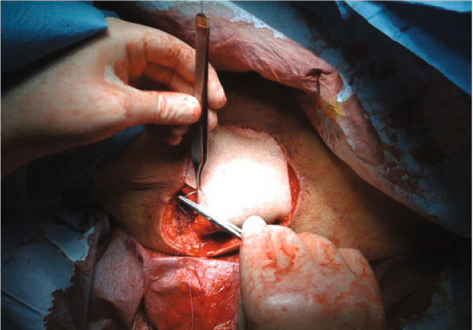
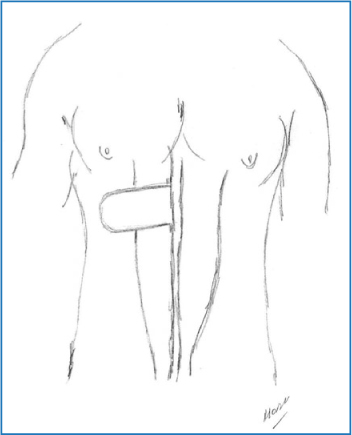
Fig. 10.22
De La Plaza skin island

Fig. 10.23
Perineal defect with extensive loss of tissue at root of thigh
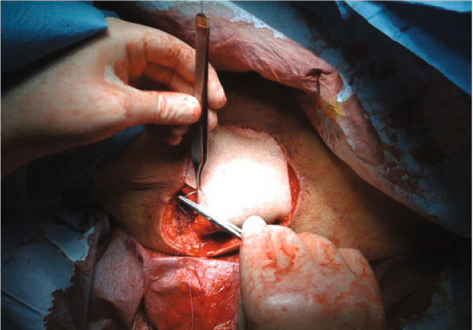
Fig. 10.24




Skin positioning into the defect
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




