Authors
Classification
Definition
Pilipshen et al. (1984) [15]
Anatomic pelvic side involved
Anastomotic
Perianastomotic
Pelvic disease without fixation
Pelvic disease with fixation
Pelvic disease (with or without fixation) presenting through the anastomosis
Suzuki et al. (1996) (Mayo Clinic) [9]
Degree and site of pelvic fixation
F0: fixed to any site
F1: fixed to 1 site
F2 : fixed at 2 sites
F3 : fixed at 3 or more sites
Guillem et al. (1998) [16]
Anatomic pelvic side involved
Axial
Anterior
Posterior
Lateral
Wanebo et al. (1999) [18]
Modified TNM classification
TR1
TR2
TR3
TR4
TR5
Yamada et al. (2001) [19]
Pattern of pelvic invasion
Localized
Sacral invasive
Lateral invasive
Boyle et al. (2005) [20]
Anatomic pelvic side involved
Central tumor
Sacral tumor
Sidewall tumor
Composite
2.3.1 Pilipshen et al. (1984)
In 1984, before the discovery of the importance of TME, Pilipshen and colleagues of the Memorial Sloan Kettering Cancer Center published a study presenting the first classification system for pelvic CRC recurrence as follows [15]:
Anastomotic: when recurrence is at the level of the anastomosis without clinically apparent contiguous extramural disease
Perianastomotic: when recurrence is presented in extramural position at the level of anastomosis but without fixation
Pelvic disease without sacral, sidewall, or anterior fixation using nonopera-tive criteria
Pelvic disease with sacral or sidewall and anterior fixation, precluding resection
Pelvic disease (with or without fixation) presenting through the anastomosis
Although this work was in the era before TME resection, the study considered for the first time the finding of recurrence fixation and a correlation between the type of first resection and the site of pelvic recurrence. Both factors are found in others classification systems.
In fact pelvic recurrences after APR were characterized by these authors as sacral, sidewall, or combined patterns of involvement in 90% of cases. After low anterior resection (LAR), the site of pelvic recurrence was described as being in proximity to the anastomosis in 67.6% of cases and had various degrees of perianastomotic (4.5%) or pelvic (48.5%) involvement.
2.3.2 Suzuki et al. (1995)
In 1995, Suzuki et al., at the Mayo Clinic, proposed a classification system that considered pain as a pattern of local recurrence (discussed above) as well as the degree of tumor fixation to both the surrounding tissue on the different sections of the pelvic wall (posterior, anterior, left and right pelvic sidewalls) and to the number of points of fixation in accordance with operative findings or histo -pathologic proof [9]:
F0: recurrences not fixed to any site, but also for recurrences confined to the small bowel (cephalad spread) or perineum (caudal spread)
F1: recurrences fixed to one site
F2: recurrences fixed to two sites
F3: recurrences fixed to three or more sites
In their work, the authors showed that patients who presented more points of fixation (F1–3) had more complications following surgery and had worse 3-year (35.7% vs. 61.3%) and 5-year (31.2% vs. 50%) survival rates compared with patients with an F0 stage (p = 0.384). This classification system was adopted by Hahnloser et al. in a study of 304 patients with LR: overall survival was significantly decreased in patients with symptomatic pain (S2) and more than one fixation sites (F2–F3) [8].
2.3.3 Guillem et al. (1998)
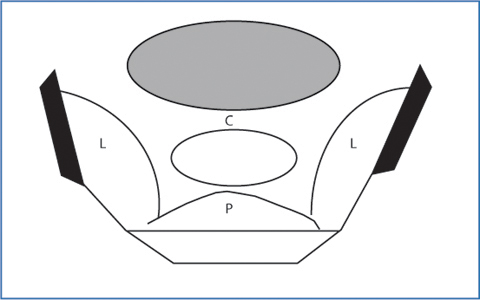
The Memorial Sloan Kettering Cancer Center group proposed a new classification system that divided the LR into four groups based on the anatomical region involved by the tumor in the pelvis (Fig. 2.1) [16]:
Axial: subdivided into anastomotic, mesorectal, and perirectal soft-tissue recurrence within the center of the pelvis (if previous SPS surgery) and perineum recurrence (if previous APR)
Anterior: when recurrence involves urinary bladder, seminal vesicles or prostate, or vagina or uterus
Posterior: when recurrence involves sacrum or presacral fascia, or sacral root sheaths or coccyx
Lateral: when recurrence involves muscles (piriformis and elevator), pelvic ureters, pelvic autonomic nerves, soft tissue of the pelvic sidewall, lymph nodes, iliac vessels, sacral nerve plexus, or lateral bony pelvis.
This type of classification, different from that proposed by Pilipshen et al., was adopted by Moore et al. in a study showing that when recurrence was axial only or axial/anterior only, the likelihood of achieving an R0 resection was high (90% vs. 43%, p = 0.001; 72% vs. 42%, p = 0.003, respectively). The same study reported that when recurrence was lateral, the likelihood of an R0 resection was significantly reduced (36% vs. 65%, p = 0.002). Moreover, the presence of hydroureteronephrosis was considered a radiologic finding that reduces the possibility of achieving an R0 resection [17].
2.3.4 Wanebo et al. (1999)
The classification system described by Wanebo et al. in 1999 was based on modified criteria of TNM staging system for primary rectal cancer [18]:
TR1: intraluminal recurrence that invades the submucosa and a minimal part of the muscular layer of the rectal wall either following local excision or at the anastomosis site
TR2: recurrence that invades the full thickness of the rectal muscular layer
TR3: recurrence is at or around the level of the anastomosis with limited extramural spread in the perirectal soft tissue and without pelvic fixation
TR4: recurrence is spread to the adjacent urogenital organs (vagina, uterus, prostate, bladder, seminal vesicles) or presacral tissues with tethering but no fixation (TR4 vagina, TR4 prostate)
TR5: corresponding invasion into the sacrum, pelvic side walls, and sacrotuberous/ ischiatic ligaments
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree