Fig. 15.1
Left cervical exposure with retraction of the sternocleidomastoid muscle, carotid artery, and internal jugular vein laterally and the trachea and thyroid medially
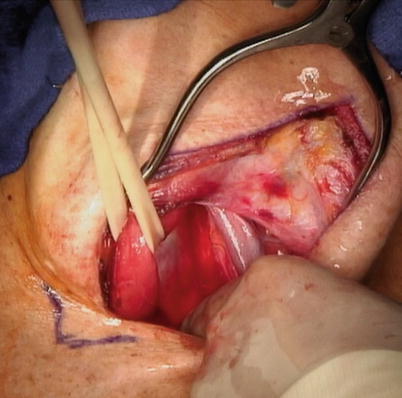
Fig. 15.2
Vessel loop encircling the cervical esophagus to aid in retraction during blunt dissection
15.1.4 Mid and Upper Mediastinal Phase
With downward retraction on the umbilical tape around the gastroesophageal junction, the posterior attachments of esophagus are dissected bluntly with a hand through the diaphragmatic hiatus to the level of the cervical dissection. Next, the anterior attachments are dissected manually, while staying directly on the anterior surface of the esophagus. Care must be taken to avoid injury to the membranous portion of the trachea and to avoid excessive pressure on the heart during dissection, which can cause hypotension. (This hypotension can be readily corrected with volume resuscitation.) Using a sweetheart retractor, the inferior lateral attachments are ligated and divided between large hemoclips. The cervical and upper mediastinal esophagus is brought out through the cervical incision, and after withdrawal of the nasogastric tube, the esophagus is divided with a GIA™ stapler (Covidien, Minneapolis, MN), securing a long Penrose drain marked to maintain its orientation during passage through the mediastinum (Fig. 15.3). With the stomach and mid/distal esophagus brought out through the abdominal incision, the gastric tube is carefully fashioned to a diameter of 4–5 cm with multiple firings of the GIA™ stapler, preserving the greater curvature and its blood supply (Fig. 15.4). The lesser curvature and a portion of the fundus and cardia are removed with the esophagus, nodal basins, and tumor (Fig. 15.5). The Penrose drain that traverses the mediastinum from the cervical to the abdominal incision is now sutured to the posterior aspect of the gastric conduit to maintain orientation during transposition to the neck.
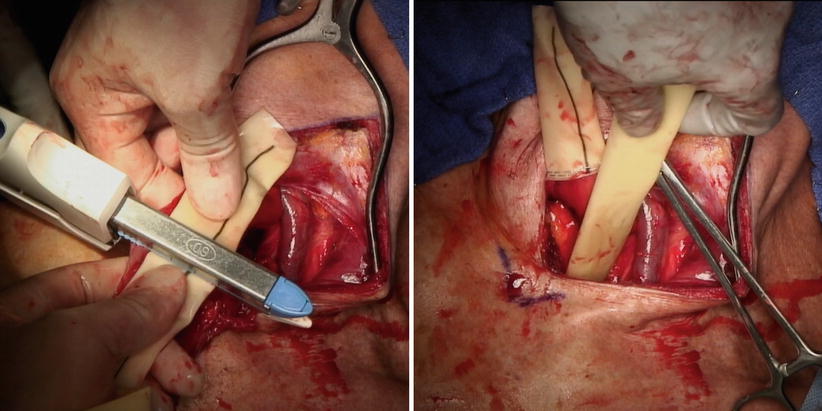
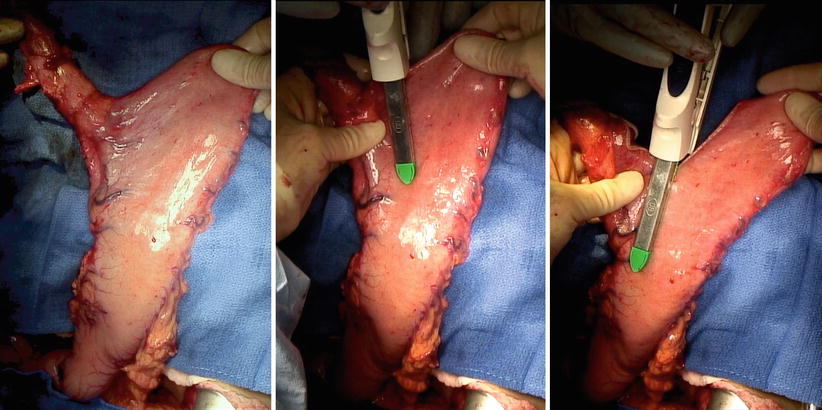
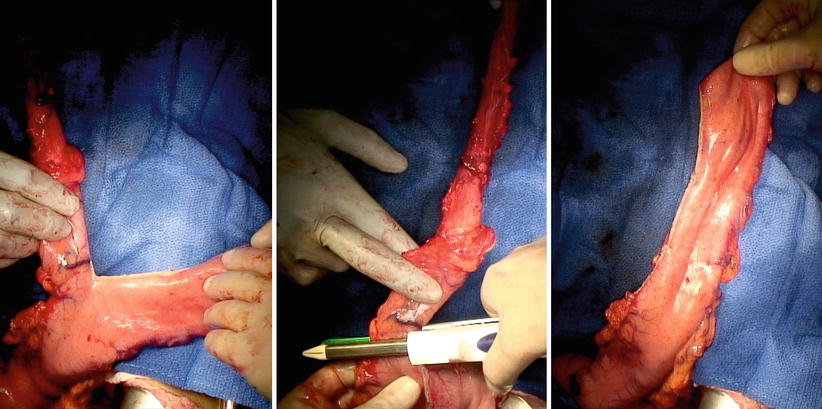
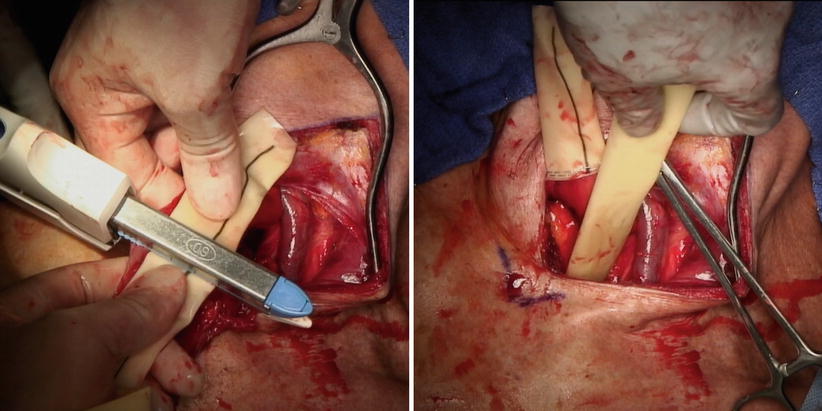
Fig. 15.3
The cervical esophagus is divided with a GIA™ stapler (Covidien, Minneapolis, MN), incorporating a marked Penrose drain to maintain orientation
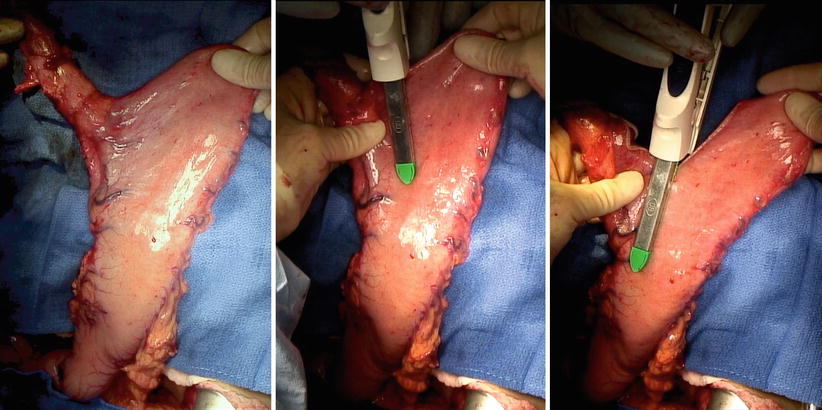
Fig. 15.4
The gastric tube is fashioned to a diameter of 4–5 cm with multiple firings of the GIA™ stapler, preserving the greater curvature and its blood supply
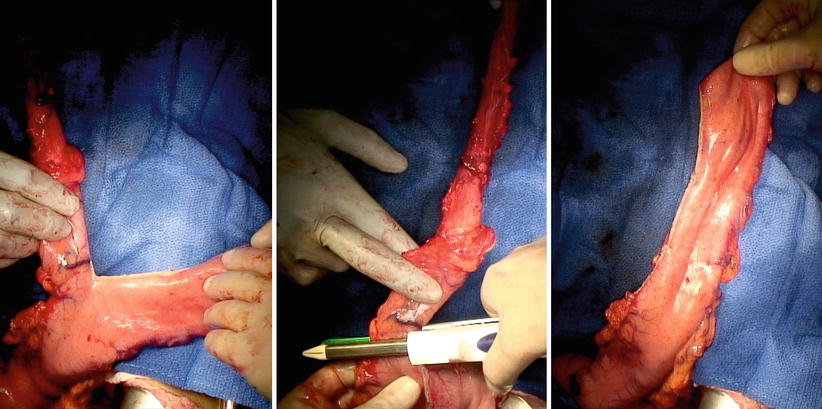
Fig. 15.5
The lesser curvature and a portion of the fundus and cardia are removed with the esophagus, nodal basins, and tumor
15.1.5 Gastric Transposition and Anastomosis
An automatic purse-string applier is used to place a nylon purse-string suture around the proximal cut end of the cervical esophagus. The anvil of a 25-mm EEA™ circular stapling device (Covidien, Minneapolis, MN) is passed into the cervical esophagus and the purse-string suture is secured (Fig. 15.6). The gastric conduit is gently pushed through the diaphragmatic hiatus while simultaneously gently pulling on the Penrose drain from the cervical incision until 6–8 cm of the stomach is mobilized into the cervical field (Fig. 15.7). Avoid excessive pulling of the gastric conduit during transposition, as the result may be trauma and ischemia that could compromise the anastomosis. Through an anterior gastrotomy, a 25-mm EEA™ circular stapling device is used to anastomose the cervical esophagus to the proximal posterior gastric wall (Figs. 15.8 and 15.9). After the nasogastric tube is replaced to the level of the gastric antrum, excess gastric tissue proximal to the anastomosis (including the anterior gastrotomy site) is excised with a TA™ 60-mm stapler (Covidien) (Fig. 15.10). The anastomosis is interrogated for an air leak and reinforced with silk sutures if necessary. The gastric tube is secured to surrounding tissue with care to avoid placing sutures in the prevertebral fascia, which could predispose to abscess formation. The platysma is reapproximated and the skin is closed with staples. Through the abdominal incision, the antrum of the stomach is secured to the hiatus and a needle catheter feeding jejunostomy tube is placed. Drains are unnecessary.
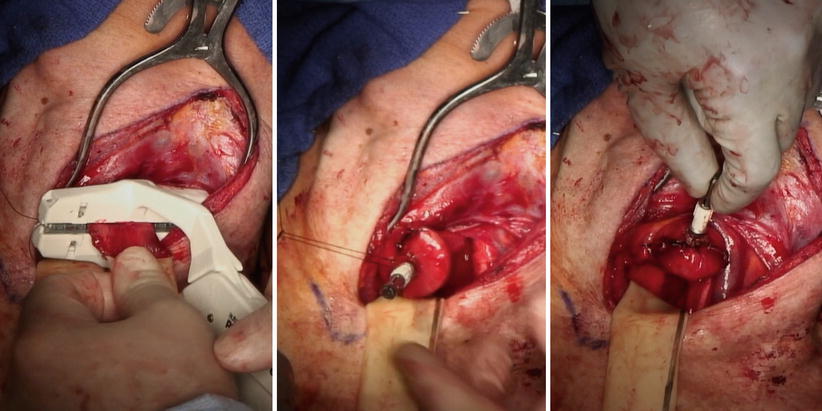
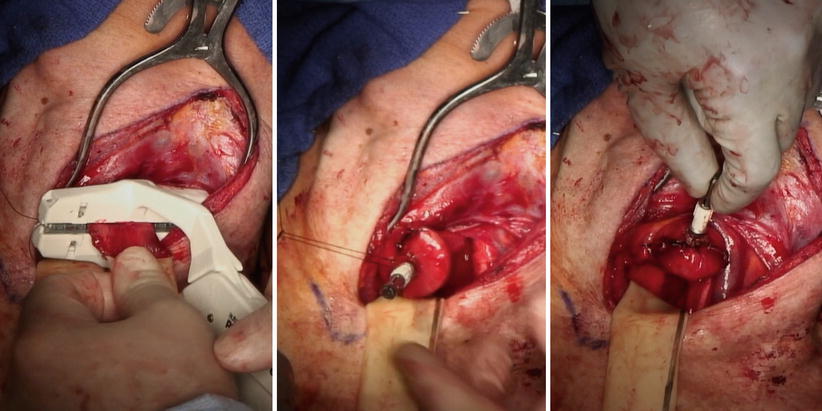
Fig. 15.6




Placement of a purse-string to anchor the anvil of the EEA™ stapling device (Covidien) to the proximal cervical esophagus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








