INTRODUCTION
In 1982, Heald et al. first described the concept of total mesorectal excision (TME) and established this technique as the gold standard for the surgical treatment of middle and lower rectal cancer. Sharp en bloc resection of the rectum and mesorectum, including high ligation of the inferior mesenteric artery (IMA), was shown to significantly reduce rates of positive circumferential resection margins (CRMs), leading to lower risk of local recurrence and higher cancer-specific survival.
Minimally invasive surgery has been shown to achieve results similar to those of open surgery with respect to oncologic resection of rectal cancer. Multiple randomized controlled trials (RCTs) have shown that laparoscopic TME is associated with similar perioperative morbidity compared to open surgery, with less blood loss, rapid intestinal recovery, shorter hospital stay, and no compromise of oncologic outcomes. Despite the failure of the recent American College of Surgeons Oncology Group Z6051 and Australasian Laparoscopic Cancer of the Rectum RCTs to demonstrate non-inferiority of laparoscopic TME relative to open TME, long-term results from several RCTs continue to support the use of laparoscopic surgery for rectal cancer and show no difference regarding oncologic outcomes. Nevertheless, relatively high conversion rates to open surgery continue to be reported, even when performed in high-volume expert centers. Robotic TME has been touted as associated with a shorter length of hospital stay, and better recovery outcomes when compared to open surgery in patients with low and mid-rectal cancer.
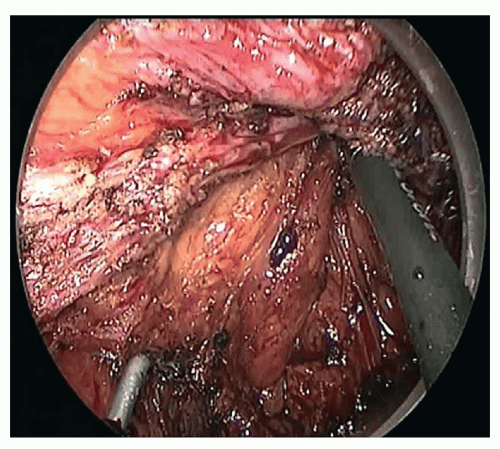
Laparoscopic and robotic surgeries have improved the approach to the pelvis when performing TME, and have been validated from an oncologic standpoint. However, achieving a complete TME with sphincter preservation and negative distal and radial margins for low rectal tumors, while preserving autonomic nerves and avoiding conversion, can be extremely challenging, even in the hands of experienced colorectal surgeons. The anatomic configuration of the distal rectum in tight apposition to the prostate, sacrum, pelvic plexus, and puborectalis, especially the narrow male pelvis, complicates the maneuvering required to complete sharp mesorectal dissection and transect the rectum well below the rectal tumor under direct visualization.
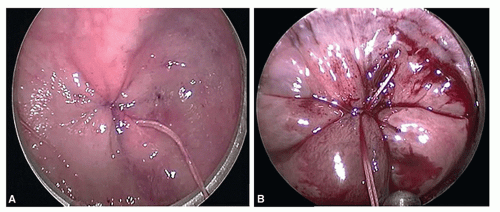
By providing direct and in-line intraluminal and transrectal access to the low rectum and mesorectum, a transanal natural orifice transluminal endoscopic surgery (NOTES) approach, first described in human cadavers in 2007, was proposed as a novel minimally invasive approach to overcome the anatomic limitation of a transabdominal approach to the low pelvis. Transanal proctectomy with total mesorectal excision (or transanal TME) with laparoscopic assistance, whereby TME is undertaken from a “bottoms-up” approach under direct visualization provided through transanal endoscopic multiport platforms, was first described in a clinical case in 2009 and has since become increasingly adopted worldwide as an attractive alternative to standard and minimally invasive TME. Benefits of using a transanal approach to complete the distal-most dissection of the mesorectum had been well described for rectal tumors located less than 5 cm from the anal verge, out of reach from a transabdominal approach, and when sphincter preservation was attempted.
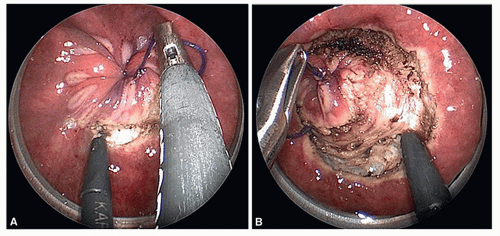
The transanal-transabdominal technique with intersphincteric resection (ISR) has evolved from the necessity of resecting part or all of the internal anal sphincter muscle in continuity with the distal rectum and mesorectum, to achieve negative distal margins for low rectal tumors. Likewise, transanal endoscopic access not only permits early identification and transection of the distal rectal margin with or without ISR but also allows taTME to be carried out entirely through a transanal endoscopic platform. With improved videoscopic visualization and exposure achieved with CO2 insufflation, nerve-sparing and complete dissection of the mesorectal fascia is greatly facilitated.
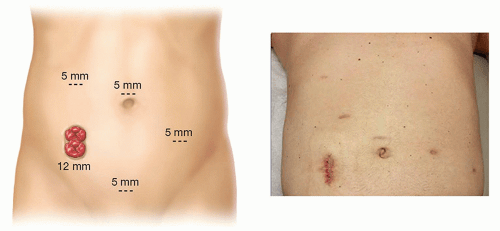
Other benefits provided by taTME include that distal rectal transection is performed transanally, under direct vision, and does not require laparoscopic staplers. Another advantage is that transanal specimen extraction, when feasible, avoids the need for specimen extraction sites and reduces wound-related complications. In addition, taTME procedures performed with a two-team approach, with both abdominal and transanal teams working simultaneously, may reduce operating time and intraoperative complications including conversion to open surgery.
Overall, despite the demonstrated benefits in postoperative recovery provided by the use of multiand single-port laparoscopy and robotics for rectal cancer resection, adoption and conversion rates have plateaued, which reflects the technical difficulties and the lengthy learning curve required for performing TME using these minimally invasive techniques. Since our first report of taTME performed for a mid-rectal cancer using a transanal endoscopic operation (TEO) rigid platform (Karl Storz, Tubingen, Germany) and an early case series reported the feasibility of this approach for rectal cancer, taTME adoption has been facilitated by increased access to disposable transanal minimally invasive surgery (TAMIS) platforms and supported by preliminary small and mid-sized series, confirming the procedural and preliminary oncologic safety of taTME. Thus far, the reported factors driving taTME adoption have been the high success with taTME completion for low rectal tumors, with sphincter preservation and exceedingly low conversion rates. In addition, oncologic results have demonstrated high rates of complete and near-complete TME grade achieved. We believe that in the hands of experienced operators, taTME is becoming the preferred approach for mid- and low rectal tumors, particularly in obese male patients because of the superior exposure provided, for procedures that would otherwise be technically difficult to approach from the abdomen.
The aim of this chapter is to provide a comprehensive review on taTME for rectal cancer, describe the procedure in detail, and summarize the preliminary outcomes of this procedure based on published results from the largest taTME series.
TRANSANAL TOTAL MESORECTAL EXCISION: TRAINING AND STANDARDIZATION OF PROCEDURES
There is clear consensus that taTME should be performed by experienced, skilled, and well-trained surgeons who can outgrow the learning curve in the most efficient way. A recent consensus of an expert group of surgeons from an international taTME conference states that training is necessary before surgeons undertake this procedure. Furthermore, it strongly recommends that surgeons undertake a taTME training course that includes didactic lectures, mentored cadaveric dissection, live surgery, and unedited video before clinical application. Ideally, this approach should be undertaken by high-volume rectal cancer surgeons with expertise not only in laparoscopic or robotic TME but also in transanal endoscopic microsurgery (TEM; Richard Wolf, Knittlingen, Germany), TEO, or TAMIS, and familiar with ISR techniques for very low rectal tumors. Institutions contemplating initiating the taTME program should demonstrate multidisciplinary expertise in the management of rectal cancer with tumor board review of all rectal cancers. Even for surgeons with all prerequisite skills for taTME, in-depth procedural training is mandatory before clinical practice. In addition, proctorship for the first few clinical cases is strongly recommended, given the lack of familiarity with anatomically correct perineal dissection planes from a perineal endoscopic approach. These recommendations stem from the fact that taTME procedures call upon mastery of several essential technical competencies, namely, laparoscopic suturing through a single-incision platform, transanal endoscopic dissection, and, most importantly, familiarity with the perineal anatomy and in-depth understanding of the relationship between the rectum, anal sphincters, prostate, and urethra.
The porcine model has been extensively investigated as a training model for transanal colorectal NOTES. However, because of the bony narrow porcine pelvis that does not allow dissection to the bottom of the pelvic floor, and given the lack of a true mesorectum, it was largely abandoned as a model for taTME training. Fresh human cadavers, on the other hand, are an optimal model for taTME training. In the largest cadaver series of transanal NOTES colorectal resections performed in 32 fresh male and female cadavers, our group demonstrated that although feasible in a few cadavers with favorable anatomy, pure transanal and combined transanal and transgastric NOTES colorectal resections were limited by the lack of specialized instrumentation, and that laparoscopic assistance was necessary to complete transanal NOTES procedures safely. With regard to the procedural learning curve anticipated for these procedures, in this large cadaver study of transanal NOTES colorectal resections, a significant decrease in the operative time and increase in the length of rectosigmoid colon mobilized was achieved after performance of the first five cases. Although no formalized learning curve analysis
has yet been performed for taTME, several mid- and large-sized institutional series have demonstrated a significant decrease in operative time with experience. In 2013, Lacy et al. reported their first 20 cases of taTME with a mean operating room (OR) time of 234 minutes. In 2015, the same group reported their experience with 140 taTME cases with a mean OR time of 166 minutes. Although this decrease in OR time may reflect the increased use of a synchronous two-team approach, it may also reflect the impact of the learning curve for surgical teams that have become experienced with taTME.
In 2014, Buscaglia et al. presented an alternative to cadaver and animal training. They introduced transanal NOTES sigmoidectomy training using an endoscopy simulation model. Four participants (two colorectal surgeons and two gastroenterologists) performed simulated NOTES sigmoidectomy with a baseline test, mentored training sessions, and a non-mentored simulated final test to the final testing. They showed a 42% reduction in operative time from the baseline performance. This preliminary data suggest that simulator use before performing the procedure in animal or cadaver models may improve the training process.
In a recent video manuscript, Mclemore et al. proposed a rigorous training pathway for taTME. This included team training in a fresh cadaver the day before the first clinical case with the same operative team consisting of surgeons, nurses, and operative staff. In addition, the case was proctored by an experienced taTME surgeon. The authors reiterated the key elements for successful development of a taTME program, including expertise in minimally invasive and sphincter-preserving TME, TES, and ISR for very low rectal invasive neoplasms. Experience with this first case reaffirmed the importance of procedural team training in cadavers.
One of the challenges of taTME has been the lack of standardization of the technique. Published reports and video presentations continuously demonstrate variations in operative setup and sequence, dissection and anastomotic techniques, and instrumentation that may or may not impact outcomes. Ongoing efforts are under way to define standard steps of taTME dissection using video-based assessments, to standardize procedures in preparation for randomized controlled comparison of taTME to other TME approaches.
Overall, prerequisite expertise in rectal cancer resections and appropriate procedural training in taTME will profoundly impact intraoperative and postoperative outcomes, especially the quality of the mesorectal dissection achieved and hence short- and long-term oncologic outcomes. Formal taTME cadaver training courses incorporate video-based didactics and hands-on training by experienced proctors. In the United States, the first American Society of Colon and Rectal Surgery (ASCRS)-sponsored taTME hands-on cadaver course and symposium was organized in May 2016.
The international (Low Rectal Cancer National Development Program) LOREC taTME registry contains 720 taTME cases performed for benign and malignant indications. The (American Society of Colon and Rectal Surgeons Optimizing the Surgical Treatment of Rectal Cancer) ASCRS OSTRiCh taTME registry used by US surgeons is identical to the LOREC registry. While awaiting the results of large prospective phase II taTME studies or RCT comparing taTME to open and or minimally invasive TME, it is hoped that these registries will accurately reflect current trends with adoption and outcomes of taTME, including operative techniques, indications, and procedural, postoperative, oncologic, and functional results. Large-scale data collected for these registries may also help standardize the technique.


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access