Fig 47.1
TEMS rectoscope with the binocular eye-piece and the instruments in the appropriate ports
Procedure
The procedure is performed under general anesthetic with full muscle relaxation, as for abdominal surgery. Prior to the procedure, phosphate enemas may be employed to clear the rectum of feces. Full oral bowel preparation is also acceptable but it is essential that the rectum itself is meticulously cleansed so for many surgeons recommend two enemas. A single dose of broad-spectrum antibiotic (Ertapenam or Pipercilin/Tazobactam) is administered. Initially the patient is placed in Lloyd Davies position to assess the position of the tumor. It is essential that when performing TEMS the tumor is in the 6 o’clock position and therefore the patient has to be moved appropriately to achieve this orientation. So, for lateral tumors the patient will be in the decubitus position, reverse Lloyd-Davies for the anterior tumors and remain in the starting Lloyd-Davies position for tumors in a posterior location.
The TEMS rectoscope is inserted and firmly secured to the table using the Martin arm (Fig. 47.1). The tubes are connected for CO2 insufflation, suction and electro-cautery. The CO2 insufflation pressure is limited to 20–25 mm of H2O and uses a specific immediate feedback system for continuous pressure monitoring to maintaining adequate rectal insufflation without excessive proximal colonic distension.
Numerous energy device options have been used for TEMS including Ligasure™, Harmonic Scalpel™, and water dissection but the commonest option remains traditional electro-cautery using either monopolar or bipolar current via a needle-point instrument. This approach should be used initially to mark out the margins of excision ensuring an adequate cuff of normal tissue (Fig. 47.2a). This step is crucial for adequate excision especially in larger lesions as it helps maintain the correct orientation during resection when the lesion becomes increasingly mobile. In other words it prevents the surgeon wandering off the correct pathway and runs the risk of a positive excision margin. The stereoscopic vision and magnification help in this respect to identify the margins of the tumor. Full thickness excision of the tumor is carried out with coagulation of any bleeding vessels (Fig. 47.2b). Meticulous hemostasis is essential throughout as hemoglobin will absorb the light and make dissection less precise. Identification of areolar tissue and mesorectal fat deep to the muscle layer help confirm the thickness of excision and the aim should be to ensure a vertical dissection through the layers of rectal wall to the depth required—coning of the excision is best avoided (Fig. 47.2b). Routine suturing of the resulting defect was recommended for all lesions in the early days of TEMS. However it is widely recognized as not being necessary assuming there have been no breaches into the peritoneal cavity when careful sutured closure is obviously required (Fig. 47.2c, d). On the other hand routine sutured closure of defects does help to maintain suturing skills for when they are required. Overall, this decision remains a matter of surgeon preference.
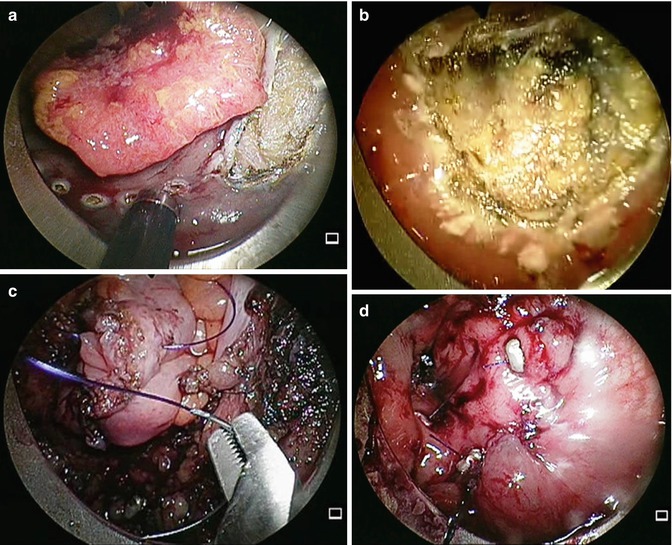
Fig 47.2
(a) TEMS Large polypoidal lesion being excised full thickness after marking excision margin with diathermy. (b) Mesorectal fat visible at the base after full thickness excision of polyp. (c) Suturing of the peritoneal defect after excision of polyp. (d) The final appearance of the area after suturing of the defects. The sutures are held in place with beads (seen)
For low rectal tumors close to the anal verge maintaining an air seal can present a particular challenge but these lesions can still be excised by wedging the rectoscope up against the anal sphincter thereby permitting adequate rectal insufflation. In addition, when excising these lowest lesions particular care must be taken to avoid excising any significant portion of anal sphincter muscle. This can be challenging at times but is essential if the risks of postoperative incontinence are to be minimized.
Complications
Early post-operative complications are unusual and generally involve mild pain and fever in the first 24 h. Pain is commoner when excision has approached the dentate line and unusual following excision of higher lesions. Post-operative urinary retention is not uncommon in male patients but is rarely a long-term issue. Probably the commonest significant complication is that of a secondary hemorrhage which may occur 5–7 days after surgery. This occurs in less than 3 % of patients but is frightening for the patient because it occurs without warning when the patient is at home. It is therefore useful to at least warn the patient of such a possibility while providing reassurance that the bleeding almost always stops spontaneously and requires no intervention in the overwhelming majority of patients. More unusual complications that have been reported include pelvic sepsis, fistula to the vagina and perineum and intra-peritoneal sepsis. A systematic review of published studies by Middleton et al. showed an overall complication rate 10.3 % for benign adenoma excision and 20 % for carcinoma excision [12] although the majority of these complications are minor in severity.
A review of UK wide TEMS database by Bach et al. showed an overall complication rate of 14.9 % and mortality of 1.4 %. Bleeding was the most common complication (9 %), followed by post op medical complication in 1.9 %, pelvic abscess in 1.7 % and perforation in 0.2 % cases [13]. Perforation in to the peritoneal cavity can be treated either by primary suture (at time of surgery) or conservatively. Morino et al. studied short and long term outcomes of peritoneal perforation after TEMS (n = 28) [14]. This study showed that conversion to an abdominal procedure was needed in 10 % (3/28) of patients with a significant peritoneal breach. Long term follow up (48 months) did not show increased peritoneal or liver metastases.
Outcomes for T1 Rectal Cancer
Early rectal cancers with favorable histological features such as SM1 invasion, well to moderate differentiation (G1–2) and no lymphovascular invasion are most suitable for TEM excision. An early study by Blair et al. showed 0 % local recurrence and mortality after local excision in T1 tumors with favorable histological characteristics [15]. However, recurrence rates varying between 0 and 21 % have been reported in the published literature and confirm the importance of appropriate patient selection [13, 16–18]. Bach et al. reviewed 424 rectal cancers of which the majority (253) were T1, and were treated with TEMS [13]. The T1 tumors were further divided in to SM1–3 based on the extent of sub-mucosal invasion. In this the local recurrence rates were 3–4 % and lowest in the Sm1 group [19].
De Graaf et al. compared outcomes in 80 patients undergoing TEMS and 75 patients undergoing TME [20]. TEM was shown to be safer with less blood loss, fewer complications, shorter hospital stay and no mortality. Follow up of more than 5 years showed that overall and cancer specific survival was similar in the two groups although the local recurrence rate after TEMS was shown to be 24 %. The only randomized trial performed to date comparing TEMS alone to radical resection (TME) showed no difference in local recurrence (4 % vs 0 %) or 5 year survival [8]. Heintz et al. studied 103 patients who underwent TEM or TME for T1 rectal cancer [9]. These patients were further stratified into low risk (G1 and 2 with no lympho-vascular invasion) or high risk (G3 and lympho-vascular invasion). The local recurrence and 5 year disease free survival were comparable between TEMS and TME. However, local recurrence rates were higher after TEMS in the high-risk group (33 % vs 18 %). Stipa et al. reviewed 144 patients of whom 86 had T1 cancer. The overall 5 year survival was 83 and 92 % for T1 tumors [21]. Interestingly in this study, of the patients who developed local recurrence the survival was better in those who had radical surgery rather than TEMS excision.
T2–3 Rectal Cancer
Local excision alone for T2–3 rectal cancer leads to an unacceptably high local recurrence rates and the majority of these patients are best served by a radical resection. A review by Tjandra et al. of 22 studies has shown a recurrence of 25 % for T2 and 38 % for T3 rectal cancer [6]. Previous individual case series have shown improved outcomes when local excision/TEMS has been combined with adjuvant chemo-radiotherapy. A phase 2 multi institutional trial performed by CALGB showed 83 % estimated overall survival and 71 % disease free survival in T2 tumors treated with LE and adjuvant therapy [22]. Long term follow up data of the patients in this study group showed overall survival of 42 % and disease free survival of 58 % at 10 years [23]. Guerriri et al. studied 84 T2 and 61 T3 rectal cancers treated with TEMS. These patients were treated with high dose radiotherapy before tumor excision. The rectal cancer specific survival at 97 months in T2 was 90 and 73 % for T3 tumors [17]. In a prospective randomized study Lezoche et al. compared outcomes in patients undergoing TEMS and laparoscopic TME for T2 rectal cancer 6 cm from anal verge [24]. All patients had received neo-adjuvant chemo-radiotherapy. At a median follow up of 84 months the local recurrence was 5.7 % for TEM and 2.8 % for laparoscopic TME group. The survival probability for both the groups was 94 %.
In the last decade another potential role for TEMS has developed for patients thought to have a complete clinical response (CCR) after neo-adjuvant chemo-radiotherapy. The pioneering work by Habr-Gama exploring the possibilities of a watch and wait program following CR have resulted in increasing use of TEMS in selected patients to confirm the diagnosis of CR by way of an excisional biopsy. The future will determine the exact role for this approach and longer term follow-up is clearly required before this approach is refined [25, 26].
47.3 Functional Outcomes After TEMS
One of the advantages of TEMS over radical resection of rectum is the maintenance of functionality and preservation of the anal sphincter. However, there have been no direct comparison studies in this regard. TEMS involves dilating the anal canal with a large diameter rectoscope for extended periods of time intuitively raising the possibility of damage to continence and a number of individual studies have addressed these issues [27–31]. Not surprisingly these have shown reduced squeeze pressures and resting tones particularly in relation to the duration of surgery. In addition, the absence of recto anal inhibitory reflex (RAIR) has been reported after TEMS. Despite these findings the majority of case series continue to document no long term problems and have shown adequate function without a change in continence after the initial 6–8 weeks following TEMS.
47.4 Recent Advances in Transanal Surgery
Two recent advances in transanal surgery that look promising are the transanal minimally invasive surgery (TAMIS) and robotic assisted transanal surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








