Fig. 34.1
A External iliac artery region: lymph nodes that are attached to the external iliac artery and vein from the bifurcation till groin; B Obturator region: lymph nodes around internal iliac artery and vein, medial border by obliterated umbilical chord, lateral border pelvic side wall, caudally femoral canal; C Common iliac artery and vein region: lymph nodes that are attached to the vessels, between aortal bifurcation and iliac bifurcation; D Presacral region lymph nodes between common iliac arteries and veins, not in the attachment with the vessels; E Paracervical region: lymph nodes between cervix, umbilical chord, and internal iliac vessels; F Low paraaortal region: lymph nodes along aorta and vena cava inferior, between aortal bifurcation and a. mesenterica inferior
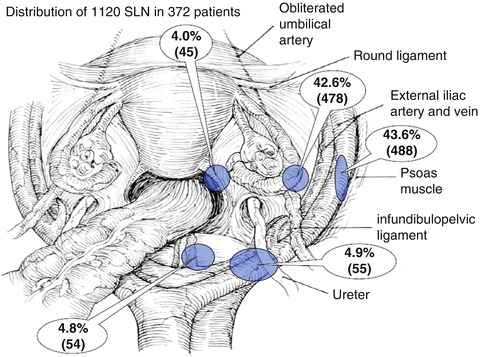
Fig. 34.2
Distribution of 1,120 SLN in 372 patients (From Rob et al. [17]. Used with permission from Elsevier)
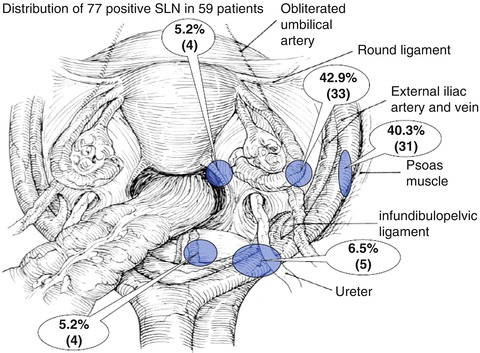
Fig. 34.3
Distribution of 77 positive SLN in 59 patients (From Rob et al. [17]. Used with permission from Elsevier)
34.5 Histopathological Procedure in SLN
We divided tumor deposits of SLNs in patients with cervical cancer into three categories: macrometastasis (diameter >2 mm), micrometastasis (diameter >0.2 mm but not >2 mm) and isolated tumor cells (ITCs, diameter ≤0.2 mm). The presence of macrometastatic or micrometastastatic disease in SLNs is described as positive nodes in the N category of the tumor, node, metastasis (TNM) staging system for cervical cancer. Although the extent of involvement of lymph nodes is an important prognostic factor, it still has not been validated in the literature. In cervical cancer surgery we have less extensive data though a recent multicenter study confirmed the prognostic significance of micrometastatic lymph node involvement [36]. However, the clinical significance of ITCs is still unknown. The identification of most micrometastases requires serial sectioning. We have no consensus about optimal leveling; however, in routine clinical practice 150–250 μm leveling seems acceptable.
A major controversy concerns FS biopsy of SLNs, including its benefits and limitations. The intraoperative assessment of SLNs potentially modifies the surgical procedure and subsequent treatment management. Despite the obvious benefits of FS examination for the patient, this technique has serious limitations in the microscopic evaluation of selected portions of tissue. Intraoperative serial cutting of the entire SLN is not applicable because of the prolongation of the operating time, technical limitations of the processing of frozen material and loss of tissue for postoperative evaluation. Presently, no standardization for the number of levels taken from each tissue block is available. Our algorithm of tissue sectioning in FS enables the disclosure of macrometastatic tumor deposits. However, it leads to reduced sensitivity in detecting micrometastases and may result in false negatives [17]. Using a good diagnostic tool such as FS allows reliable detection of clinically important metastases in lymph nodes (metastases >2 mm), but will miss a significant proportion of patients with micrometastatic disease (<2 mm) and ITCs [11, 23, 24, 27, 37–39]. Importantly, if there were negative SLNs in the hemipelvis in early cervical cancer, it is extremely rare to have metastasis in non-SLNs [16–19, 22, 23, 27–31, 40]. Further, if there were micrometastases in final ultrastaging of SLNs that were missed by FS, it is extremely rare to have metastasis in non-SLNs [39, 41–43]. Selection of patients with macrometastatic positive SLNs allows preoperative modifications of the treatment. In contrast, negative FS of SLN biopsy for early cervical cancer is an important adjunct of individually tailored less radical treatment options [43–47].
34.6 Identification of SLNs: Detection Rate
The cervix is a midline structure where the DR per patient is less accurate than the DR per hemipelvis (SSDR). General agreement has been emerging that optimal mapping implies identification of at least one SLN on each side. It is evident that Tc 99m or Tc 99m with blue dye is superior to blue dye alone. During the past decade, studies on SLNM have used different patient selection criteria, application methods, radiocolloid particles and timing of SLNM. In the literature the DR in tumors with small tumor volume (<2 cm) was 93.8–100 % and 58–87.8 % in tumors with large tumor volume (>2 cm). The SSDR, a more important measure, was 69.4–95.6 % in tumors with small tumor volume and 41.9–69.5 % in tumors with large tumor volume. Concerning clinical practice, the sensitivity and negative predictive value (NPV) for endpoints are also of importance. Sensitivity in the group of patients with small tumor volume was 99–100 % versus 84–100 % in the group with large tumor volume. Table 34.1 summarizes the results of our FN Motol ultra-short protocol.
Table 34.1
Results of the “prague fn motol protocol”
Stage | Number of patients | DR (%) | SSDR (%) |
|---|---|---|---|
IB1 <20 mm | 182 | 98.4 | 95.6 |
IB1 >20 mm | 92 | 94.6 | 91.3 |
IB2 (NAC) | 98 | 90.8 | 86.7 |
34.7 Summary
In the past two decades considerable attention has been directed toward optimal surgical management of early cervical cancer. Although enormous efforts have been made in developing exact preoperative methods to identify nodal involvement, diagnostic accuracy is still limited in terms of low sensitivity and specificity in detecting lymph node metastasis, especially in early cervical cancer. Several studies have confirmed that SLNM is a feasible and accurate technique in predicting the status of pelvic nodes in early cervical cancer patients. Using SLNM, we found that 15 % of the SLNs from “unusual’ locations could be identified. SLN biopsy and serial sectioning allowed precise histopathological evaluation of the “high-risk” nodes because serial sectioning and ultrastaging of whole lymph nodes were not possible. There are sufficient data to suggest that SLNM with 99mTc plus blue dye in the hands of an experienced surgeon should prove important in fertility-sparing and individually tailored surgery for cervical cancer.
Key Points
Sufficient data are available to suggest that SLNM mapping with a combination of 99mTc and blue dye should prove to be an important component in fertility-sparing and individually tailored surgery.
A number of studies confirm that SLNM is feasible and highly accurate in predicting the status of regional lymph nodes in small volume cervical cancer (<2 cm and less than one-half stromal invasion).
Uncommon lymphatic drainage has been reported in 15 % of cervical cancer patients.
Recent data establish that intraoperative detection is more sensitive than preoperative lymphoscintigraphy. A question for thought is whether the added benefit of preoperative lymphoscintigraphy for SLNM detection in cervical cancer is justified.
The cervix is a midline structure whose lymphatic drainage is bilateral and therefore DR must be interpreted per side (SSDR).
Bilateral SLN detection with histopathology ultrastaging is more sensitive than systematic pelvic lymphadenectomy.
References
1.
2.
3.
4.
5.
6.
Vrzackova P, Weiss P, Cibula D. Sexual morbidity following radical hysterectomy for cervical cancer. Expert Rev Anticancer Ther. 2010;10(7):1037–42.CrossRefPubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








