3. THE STOMACH
BASIC FUNCTIONS
After studying this chapter you should be able to:
1. Understand the relationship between the structure of the stomach and its function in the process of digestion.
2. Understand the secretory processes of the stomach mucosa and how dysfunction may influence digestion, absorption and body homeostasis in terms of:
a. Acid–base balance
b. Red blood cell formation in the bone marrow.
3. Understand the protective functions of the stomach including those relating to:
a. Mucosal structure and secretion
b. Acid and pepsin secretion.
4. Understand the importance of stomach smooth muscle function in:
a. The storage of food
b. Mixing the food with the digestive secretions
c. The regulation of the entry of the stomach contents into the small intestine.
5. Understand the process of vomiting.
Introduction
The primary function of the stomach is to store the food ingested during a meal and to regulate its release into the duodenum. Its other functions are to churn and mix the food with the gastric secretions producing a thick mixture known as ‘chyme’. In addition it has a range of exocrine, paracrine and endocrine functions. The exocrine secretions, which are released into the stomach lumen are digestive juices, collectively known as gastric juice. The major paracrine secretion is histamine, a substance that stimulates gastric acid secretion. The major endocrine secretion is the hormone gastrin, which acts both locally on the stomach smooth muscle and mucosa to stimulate gastric motility and acid secretion, and distally on the intestines, pancreas and liver.
In this chapter, the secretory and emptying functions of the stomach will be considered in the light of a clinical problem concerning the consequences of partial gastrectomy, a condition in which these functions are compromised (Case 3.1: 1). Another clinical problem, the consequences of excessive vomiting, is also used to highlight the importance of the stomach for homeostasis. The control of stomach functions is the subject of Chapter 4.
Case 3.1
A 72-year-old man complained to his general practitioner that he had recently started to feel tired and listless. He also complained of longstanding symptoms of dizziness, sweating and palpitations after meals. Eight years previously, he had undergone a partial (proximal) gastrectomy that involved removal of most of the body and fundus of the stomach. At first, he had felt reasonably well but in the past 2 years he had become forgetful and had neglected to attend for his medication – vitamin B12 injections. The doctor told him that he should start the medication again, and should also try to regulate his food intake more carefully by eating smaller, but more frequent meals, as his symptoms were partly due to the rapid entry of large amounts of material into the small intestine. The doctor also sent him for a blood test. The patient was found to be suffering from megaloblastic anaemia, and mild metabolic acidosis. His blood vitamin B12 level was low and he was found to be mildly iron-deficient.
Note: The consequences of partial surgical resection of the stomach depend on the part being removed. Removal of the upper part of the stomach (body and fundus), as in this patient, will remove the majority of the oxyntic cells, whereas resection of the lower part, the antrum and pylorus, will remove most of the G cells.
It can be inferred from studying the details of this case that a good quality of life can be maintained after such a partial gastrectomy if:
• The development of pernicious anaemia is prevented
• The development of iron-deficiency anaemia is prevented
• Food intake is carefully regulated.
We can also infer that the digestive functions of the stomach are not essential for life.
Anatomy and morphology of the stomach
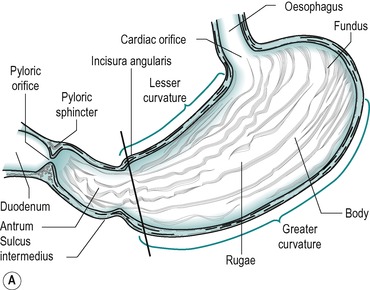
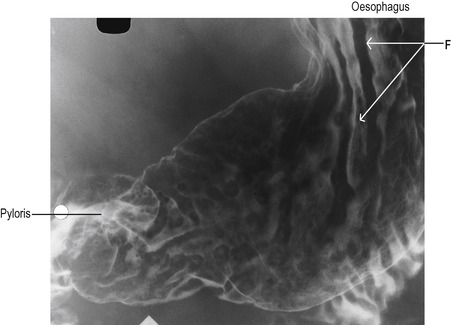
The stomach is a storage sac located between the oesophagus and the duodenum. Figure 3.1 indicates the major features of the stomach. It consists of three regions: the fundus, which is the upper region; the main body; and the antrum. Folds, known as rugae, are present on the inner surface of the empty stomach. The rugae can be clearly seen in Figure 3.2 which shows an X-ray of a stomach. The rugae flatten out as the stomach fills. A rare condition known as Ménétrièr’s disease is characterized by giant gastric folds due to hypertrophy of the gastric epithelium (Box 3.1).
Box 3.1
Ménétrièr’s disease is a condition characterized by hypertrophy of the gastric epithelium that results in the secretion of abnormally large amounts of mucus, and loss of plasma proteins. This dangerous loss of protein can lead to reduction in the extracellular fluid volume, shock and dehydration. It can be treated by antisecretory drugs or enteral protein replacement, but these measures are not usually very effective.
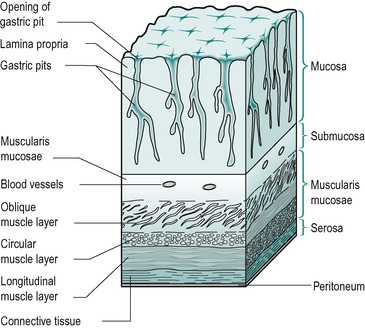
The wall of the stomach consists of various layers of tissue (Fig. 3.3). The inner lining is known as the mucosa. It comprises the lamina propria and the gastric glands (or pits). Beneath this lie the submucosa, the muscularis mucosae and the serosa which is covered by the peritoneum. The wall structure of the stomach is similar to that present throughout the rest of the gastrointestinal tract (see Ch. 1), except that the stomach has an oblique muscle layer in addition to the circular and longitudinal layers in the muscularis mucosae. This facilitates distension of the stomach and the storage of food. The muscle layers are not evenly distributed over the wall of the stomach. The external circular muscle layer is relatively thin in the fundus and body, and thick in the antrum, where strong muscular contractions aid the mixing of food. In addition, it is highly developed in the pylorus where it becomes a functional sphincter that regulates stomach emptying.
 |
| Fig. 3.3 |
The lining of the stomach is covered with a protective layer of columnar epithelial cells. These have well developed tight junctions to protect the underlying tissue from erosion by acid. In addition, the columnar cells secrete mucus and alkaline fluid to further protect the gastric mucosa from injury. The mechanisms of damage to the mucosal barrier are discussed in Chapter 4. Numerous gastric pits (approximately 3.5 million in the human) penetrate the surface. These are short ducts into which the more deeply lying gastric glands empty their secretions. The secretions enter the main compartment of the stomach via the necks of these ducts.
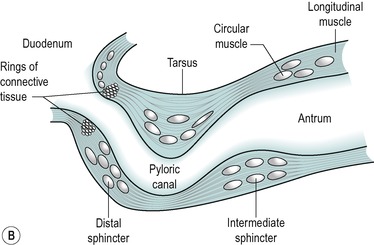
The stomach is separated from the duodenal bulb by the pyloric sphincter. Figure 3.1B shows the main structural features of the pylorus. It is not an anatomically discrete sphincter but a development of the circular smooth muscle layer. A ring of connective tissue separates the pylorus from the duodenum, enabling the contractions of the two regions to be independent. However, the myen-teric nerve plexi of the pylorus and duodenum are continuous (see Ch. 7).
Secretory mucosa of the stomach
The secretory mucosa of the stomach can be considered as two separate regions (Fig. 3.1): the upper region comprising the fundus and the body of the stomach, known as the oxyntic glandular area, and the lower antral and pyloric region which secretes the hormone gastrin.
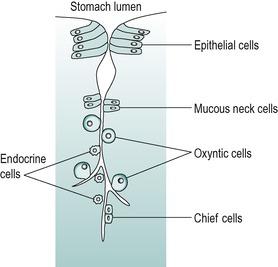
The secretory cells of the oxyntic glandular area produce most of the exocrine digestive juice known as gastric juice. The major secretory cells present in this area are oxyntic (or parietal) cells that secrete acid and intrinsic factor, and chief (or peptic) cells that secrete pepsinogen, the precursor of the proteolytic enzyme pepsin. The stomach also contains enterochromaffin (ECL)-like cells that secrete histamine, and D cells which secrete somatostatin. The gastrin-secreting cells, G cells, are restricted largely to the antral region. The secretions of these cells are involved in the control of many digestive functions including gastric secretion and motility (see Ch. 4).
Histology
The oxyntic cells and chief cells are located in deeper regions of the pits as are the endocrine cells. Mucus-secreting cells are located in the neck region providing a protective barrier to the deeper lying secretory cells. The location of endocrine cells in the deeper aspect of the gastric pits facilitates uptake of their secreted granules by the underlying capillaries (Fig. 3.4).
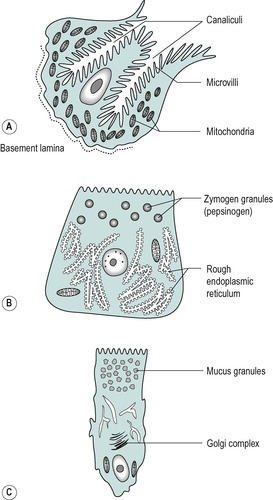
Figure 3.5 shows the three major exocrine cell types that produce secretions that enter the lumen of the stomach. These cells are all specialized in various ways to perform their secretory function. The oxyntic cell has a vast surface area enabling it to produce large amounts of secretion. Invaginations of the luminal cell membrane form canaliculi (tubular passages) that penetrate deep into the cell. The canaliculi open on to the cell’s free surface. They are lined with finger-like processes, known as microvilli, and these provide a large surface area for transport of secreted substances (see Ch. 1). When the cell is actively secreting, the canaliculi enlarge, as they fill with secreted juice. These cells are also rich in mitochondria that provide the energy in the form of ATP required for the secretory process.
The chief cell is specialized for the secretion of enzyme protein. It contains an extensive network of rough endoplasmic reticulum, the site of protein synthesis. Numerous dense zymogen granules, the loci of storage of the enzyme precursor protein, are located towards the luminal side of the cell.
Composition of gastric juice
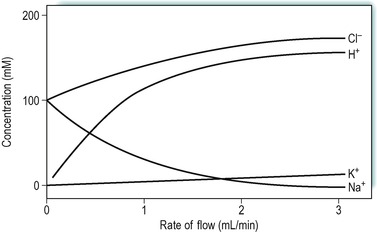
The adult human secretes approximately 2L of gastric juice per day. When a meal is being eaten, soluble substances in the food material stimulate the secretion of gastric juice. The stomach produces two different secretions: an acid secretion known as parietal juice which is released from the oxyntic (parietal) cells, and an alkaline juice released from the mucous cells. Gastric juice is isotonic with plasma but the concentrations of its various constituents vary with the rate of flow: the higher the rate the greater the acidity. During a meal therefore, the chyme becomes more acid; the acidity can reach pH 2.0. Maximum acid secretion can be induced by injection of histamine. Figure 3.6 shows the changes in concentration of some of the constituent ions in an individual in whom secretion was stimulated by injection of histamine. This procedure is used clinically to assess the secretory function of the stomach. It is known as the Gray and Hollander test after the physicians who first developed it in the early twentieth century. More recently, pentagastrin, a synthetic drug which contains the terminal tetrapeptide active site of gastrin, has been used instead of histamine, thereby avoiding the side-effects due to the action of histamine on H1 receptors (e.g. hypertension, dizziness, headache, palpitations). However, intragastric pH-metry (for 12 or 24h) has largely superceded the used of gastric secretory tests because this offers more accurate measurement of gastric acidity and is done under more natural conditions.
The concentration of H+ ions increases with rate of flow, as does that of Cl− and K+ ions, while the concentration of Na+ ions decreases. These changes in composition occur because when the stomach is stimulated during a meal it is only the rate of the acid parietal secretion that increases appreciably. The secretion of alkaline fluid is mainly a passive process and so its rate is relatively unaffected. Thus dilution of the chyme by the alkaline juice is therefore less at high flow rates and the H+ and Cl− ion concentrations increase. Both acid and alkaline secretions are isotonic with plasma.
Absence of HCl secretion (achlorhydria) is seen when the gastric pits are destroyed. It is usually associated with lack of intrinsic factor that results in vitamin B12 deficiency and pernicious anaemia (see below). However, when loss of HCl secretory capacity occurs, the first clinical manifestation is usually iron-deficiency anaemia because lack of acid results in ingested iron being retained in an unabsorbable form (see Case 3.1: 5).
Cellular mechanisms of secretion
Secretions of the oxyntic cell
Hydrochloric acid
The secretion of H+ and Cl− ions by the stomach are both active processes. The energy is derived from the hydrolysis of ATP. The H+ ions are transported against an enormous concentration gradient: the concentration of H+ ions in the blood is approximately 10−8M while the concentration in the stomach lumen can be as high as 1.5 × 10−1M.
The mechanism whereby the H+ ions are generated within the cell is outlined in Figure 3.7. Carbon dioxide diffuses into the cell from the plasma. Inside the cell it combines with water to form carbonic acid. This reaction is catalysed by the enzyme carbonic anhydrase. The carbonic acid dissociates to give H+ and HCO3− ions. The HCO3− ions are transported into the blood, down a concentration gradient, in exchange for Cl− ions. The secretion of HCO3− ions into the blood when the stomach is secreting acid into the lumen results in the plasma becoming transiently alkaline. This phenomenon is known as the ‘alkaline tide’.
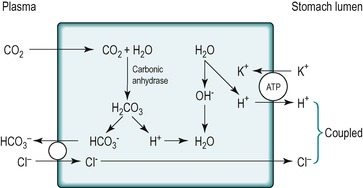 |
Fig. 3.7 Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|