2. THE MOUTH, SALIVARY GLANDS AND OESOPHAGUS
After studying this chapter you should be able to:
1. Describe the structures of the mouth and oesophagus.
2. Understand the mechanisms of taste, mastication, salivary secretion and swallowing.
Introduction
The functions of the mouth and oesophagus include:
• Mastication
• Taste
• Swallowing
• Lubrication
• Digestion
• Speech
• Signalling of thirst
• Protection of the body from harmful ingested substances.
The performance of all of these functions depends on the presence of saliva. In this chapter, the functional importance of saliva is illustrated by the problems encountered in individuals with xerostomia (dry mouth), a condition characterized by pathological changes in the salivary and mucous glands that result in impaired secretion (see Case 2.1 and Case 2.1). A second problem, involving denervation of structures following oral surgery is used to highlight the importance of nerves in control of functions in the mouth (see Case 2.2 and Case 2.2).
Case 2.1
A 60-year-old woman visited her general practitioner and complained of a persistent dry mouth, difficulties in chewing and swallowing, and sore gritty, eyes. She also said that her food seemed tasteless. The doctor examined the patient’s mouth. Her gums and teeth appeared inflamed and infected, and her tongue appeared lobulated. The patient was sent for investigation of salivary function.
The most frequent cause of dry mouth (xerostomia) is hypofunction of the salivary glands (which is often accompanied by hypofunction of the lacrimal glands). Figure 2.1 shows the appearance of the tongue in a patient with xerostomia.
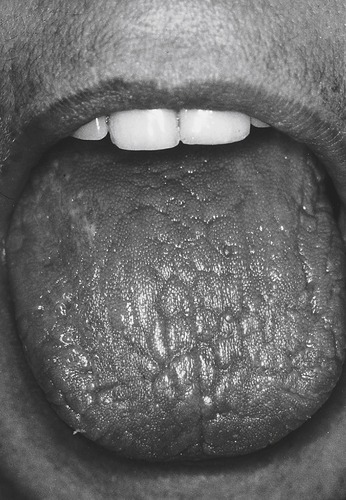 |
| Fig. 2.1 (Courtesy of Mr J. Hamburger, Dental School, University of Birmingham.) |
The following questions will be addressed:
• What are the major causes of dry mouth? Which oral conditions are associated with xerostomia? Which systemic conditions are associated with xerostomia?
• How can salivary function be assessed?
• Why is saliva important for oral and dental health?
• Which functions of the mouth would be impaired in xerostomia?
• Why is saliva important for the functioning of the oesophagus?
• Which drugs or other treatments can be used to alleviate xerostomia and what side-effects might be expected from these treatments?
Case 2.1
Causes and diagnosis
Causes
Xerostomia is a fairly common condition. Its prevalence is approximately 2% of the general population. It affects more women than men. The incidence increases with age. It is associated with conditions that are commoner in middle and old age, possibly partly because of the higher incidence of people on medication in these age groups. The symptoms are dry eyes and dry mouth. The major causes are:
• Medication, especially tricyclic antidepressants and sympathomimetic drugs
• Head and neck irradiation
• Autoimmune inflammatory diseases such as Sjögren’s syndrome, which targets exocrine glands in general.
Sjögren’s syndrome
In some patients with Sjögren’s syndrome the ducts of the submandibular glands are obstructed and the glands become swollen (Fig. 2.2). In such patients the submandibular glands in the neck are clearly located. Characteristically in Sjögren’s syndrome, there is atrophy of acinar tissue. It should be noted however, that there is normally an average loss of approximately 40% of acinar tissue between the ages of 40 and 65 years. Ductal hyperplasia and focal periductal infiltrates of lymphocytes (largely helper T cells) are also seen in Sjögren’s syndrome.
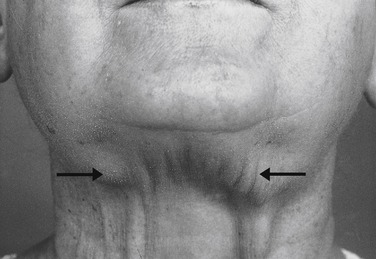 |
| Fig. 2.2 (Courtesy of Mr J. Hamburger, Dental School, University of Birmingham.) |
Figure 2.3 shows a histological section of a minor salivary gland in a patient with Sjögren’s syndrome, in which focal aggregates of lymphocytes can be clearly seen. In non-autoimmune inflammatory disease, the infiltration with lymphocytes is more diffuse. Atrophy of the mucous glands in the buccal mucosa may also be present. Primary Sjögren’s syndrome is characterized by dry mouth and eyes, but a secondary form exists in which these symptoms are accompanied by connective tissue disease, usually rheumatoid arthritis or lupus erythematosus, primary biliary cirrhosis, polymyositis, and a number of other conditions. In some patients with HIV disease the condition resembles Sjögren’s syndrome. Diabetes mellitus and diabetes insipidus can also cause symptoms of xerostomia as these conditions are accompanied by dehydration resulting from copious urine flow.
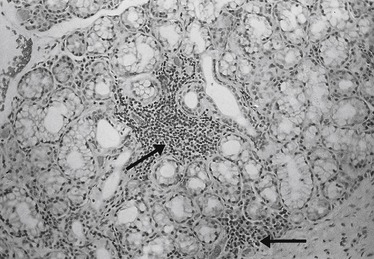 |
| Fig. 2.3 (Courtesy of Mr J. Hamburger, Dental School, University of Birmingham.) |
Symptomatic xerostomia
The ‘perception’ of oral dryness, in the absence of actual oral dryness, termed ‘symptomatic xerostomia’, can be the result of sensory or cognitive disorder. In addition, altered perception of oral sensation (oral dysaesthesia) is a feature of anxiety, although acute anxiety can actually cause clinical symptoms and signs of xerostomia.
Diagnosis
A simple test for xerostomia that can be carried out in the surgery involves swabbing the tongue with 5% citric acid, and measuring the volume of saliva that can be spat out into a graduated tube. Alternatively, a Curby cup can be placed over the opening of Stensen’s duct. This creates a vacuum and saliva can be collected. Saliva can also be collected with a pre-weighed sponge. Swallowing difficulty can also be assessed, i.e. whether water has to be taken with dry food for swallowing to be accomplished (e.g. the ‘cream cracker’ test). All of these tests have to be interpreted with care, but on the basis of such tests patients are initially categorized into ‘responders’ who have functional salivary gland tissue and ‘non-responders’ who do not. Scintigraphy (scintiscanning) is a technique involving intravenous administration of a radioisotope, usually technetium pertechnetate, a gamma emitter with a short half-life. This is taken up into the salivary acinar cells. Uptake with time can be measured using a Geiger counter. Responders by definition have functioning Na+/K+/Cl− co-transporters that can carry Cl− ions or technetium pertechnetate across the acinar cell membrane. Water moves passively across the membrane as a consequence. Non-responders have no functional epithelium and therefore cannot handle pertechnetate correctly. In Sjögren’s syndrome, there is a slow uptake of the isotope, a low peak value and a prolonged excretory phase.
Case 2.2
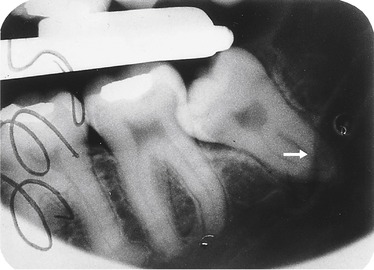
An 18-year-old man was admitted to hospital to have an impacted wisdom tooth extracted. The operation involved reflection of a flap of tissue to allow extraction of the tooth. In this patient the inferior dental nerve ran unusually close to the apical part of the tooth root and the nerve was accidentally damaged. (Figure 2.6 shows an X-radiograph from a subject in whom the dental nerve is abnormally close to the root of a wisdom tooth). Unfortunately, in the patient the lingual nerve was also damaged during the surgical procedure because it also ran unusually close to the tooth. As a result, after the anaesthetic had worn off, the side of the patient’s tongue and the lower lip on the operated side of his mouth were numb.
Perusal of this case history may provoke the following questions:
• Would the damage to the inferior dental nerve and the lingual nerve affect the patient’s ability to chew, swallow, or his speech?
• Would the nerve damage affect the patient’s sense of taste?
• Would the patient have defective salivary secretion and defective sense of taste?
• Would loss of pain sensation be a problem for this patient? Why was the patient’s lower lip numb?
The mouth
Anatomical features of the mouth
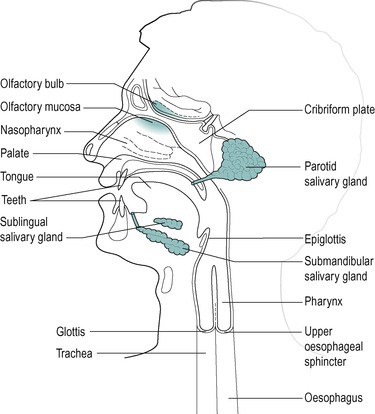
The oral cavity (mouth) is closed by the apposition of the lips. The lips and the cheeks are composed mainly of skeletal muscle embedded in elastic fibro-connective tissue. Figure 2.4 shows the anatomical features of the oral cavity and the structures within it, including the tongue and the teeth. It also shows associated structures, such as the olfactory mucosa, which are important for the functioning of the digestive system.
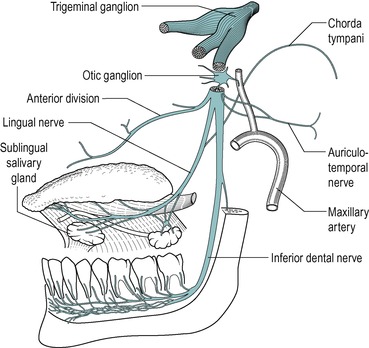
Innervation
The innervation of many structures of the mouth is via the four branches of the mandibular division of the trigeminal nerve (Fig. 2.5). These are:
1. The anterior division, which innervates the lateral pterygoid, temporal, and masseter muscles which are involved in mastication (see below)
2. The auriculotemporal nerve, which innervates structures of the ear
3. The inferior dental nerve, which innervates the lower lip and the tooth pulp, periodontal ligaments and gums
4. The lingual nerve, which innervates the anterior two-thirds of the tongue, the floor of the mouth, and the gum on the lingual side of the lower teeth.
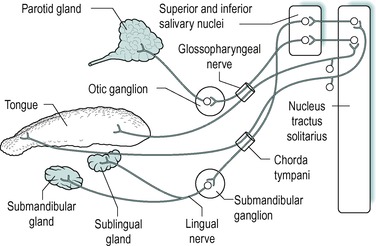
The lingual nerve is joined by the chorda tympani that run through the lateral pterygoid muscle. The chorda tympani carries sensory taste fibres from the lingual nerve to the facial nerve, and secretomotor (parasympathetic) fibres from the facial nerve to the lingual nerve. These fibres innervate the submandibular and sublingual salivary glands. Nerve damage is not uncommon following dental procedures, and this is described for a patient who had undergone a wisdom tooth extraction (see Box 3).
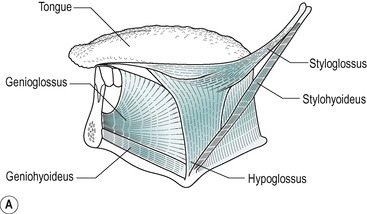
Anatomy and histology of the tongue
The tongue has a freely moveable portion known as the body, and a basal or root portion that is attached to the floor of the oral cavity, and forms part of the anterior wall of the pharynx. It is divided into anterior and posterior regions by the sulcus terminalis, a V-shaped groove with the apex of the V directed posteriorly. It is composed largely of skeletal muscle fibres and glands, and is covered by a mucous membrane. Some of the muscle fibres are intrinsic, and are confined to the tongue. These are arranged vertically, transversely and longitudinally. There are also extrinsic fibres, which originate outside the tongue, mainly on the mandible and hyoid bone, and pass into the tongue (Fig. 2.7A). The glands are located between the muscle fibres. The glands in the base of the tongue are mainly mucous and their ducts open behind the sulcus terminalis. In the body of the tongue, the glands are mainly serous and their ducts open anterior to the sulcus. Near the tip, the glands are mixed and their ducts open onto the inferior surface of the tongue.
On the upper surface of the tongue are numerous small protuberances, or papillae, which give the tongue its roughened appearance. Different types of papillae are present and these have different distributions on the tongue; fungiform and foliate papillae are present on the anterior and lateral surface and circumvallate papillae are on the base of the tongue. Papillae contain numerous nerve endings that sense touch. Most papillae have associated taste buds (see below). Lymphatic nodules (the lingual tonsil) protrude from the surface of the posterior one third of the tongue and give it a nodular, irregular appearance. Between the nodules are crypts where the epithelium is infiltrated with numerous lymphocytes. The inferior surface of the tongue is smooth and is underlain by a submucosa.
Taste
Taste buds
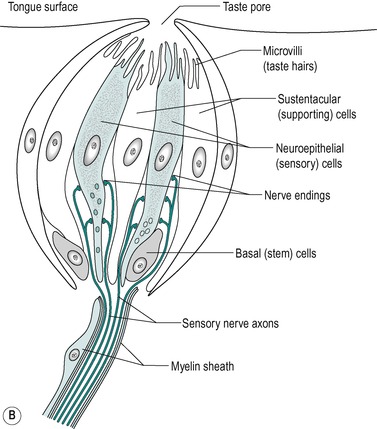
There are several thousand taste buds on the human tongue. Each circumvallate papilla contains several hundred taste buds. The taste buds contain the gustatory (taste) receptor cells. Figure 2.7B shows the structure of a taste bud. They are located in the oral (stratified squamous) epithelium, mainly in association with the papillae, but can be situated elsewhere in the oral cavity such as the palate and the epiglottis. They lie within the epithelium. They have a pale, barrel-shaped appearance with a depression, the taste pore, in the surface. This is an aperture that provides communication with the exterior. It contains three types of cell: supporting (sustentacular) cells, neuro-epithelial taste cells, and basal cells. The supporting cells lie at the periphery, and are arranged like the staves of a barrel. The neuroepithelial cells, 10–14 in each taste bud, lie more centrally. Two types of neuroepithelial sensory cell can be distinguished under the electron microscope; one type contains clear vesicles within its cytoplasm and the other contains dense core vesicles. The presence of different vesicles is consistent with the presence of different transmitter substances. These are stored in the vesicles prior to being released from the cell. Both the sensory cells and the support cells have long apical microvilli, or taste hairs, which project into the taste pore. The taste hairs lie in amorphous polysaccharide material that is secreted by the supporting cells. The basal cell is located peripherally near the basal lamina. These are the stem cells for the other cell types. There are club-shaped endings of sensory nerves lying between the cells. Chemical (taste) stimuli are received by the neuroepithelial cells and transmitted via the release of neurotransmitters from the cells to the nerve endings. The secretions of the serous glands of the papillae wash away food material and permit new taste stimuli to be received by the receptors.
Taste sensation
The solubilization of food constituents by saliva enables the sense of taste to be experienced. Thus, taste depends on the detection of chemicals that are dissolved in the saliva and for this reason, taste is compromised in xero-stomia (see Box 4). There are four submodalities: salt, sour (acid), sweet and bitter. Dissolved substances with these properties stimulate the receptors (the taste buds) on the tongue. Acid is the most potent stimulus; in humans, sucking a lemon can lead to the maximum rate of secretion, which can be 7–8mL of saliva per minute. A taste bud responds to several or all of these submodalities, but each taste bud is most sensitive to one particular taste. However, all taste buds respond to all four stimuli, given high enough concentrations of the appropriate chemicals. The taste buds that respond primarily to each submodality are situated as follows:
Case 2.1
Consequences for the functioning of the mouth and oesophagus
Lubrication
Saliva is necessary to aid chewing, swallowing and speech because of the lubricant properties conferred on it by its mucin content. Therefore these functions are all compromised in xerostomia. Saliva is necessary for mastication because it coats the food and lubricates it, making it more easily moved about in the mouth. During swallowing it is more easily moved back into the pharynx where it stimulates the pressure receptors that initiate the process, enabling it to pass smoothly into the oesophagus. Individuals with xerostomia therefore require fluid intake with food to enable chewing and swallowing to take place. The lubricant properties of saliva also assist the passage of the food bolus down the oesophagus and prevent abrasion of the walls by hard material in the swallowed food.
Digestion
Lack of salivary α-amylase does not result in malabsorption of starch if pancreatic α-amylase secretion is adequate, as the amylases from the two sources have similar catalytic actions in starch digestion, and adequate amounts of α-amylase are secreted by the pancreas.
Solution
Saliva is important for taste as it depends on substances dissolved in saliva. It is also important for the solution of substances that are absorbed by mouth.
Moistness
Lack of saliva signals thirst. Thirst is therefore a constant sensation in xerostomia.
Protection
Saliva is also important for oral and dental health: it washes the mouth, buffers acids in the food, and contains antimicrobial substances. Infections of the mouth are rare following dental surgery even though it is difficult to maintain aseptic conditions in the mouth. However, infections of the mouth and associated structures are common in xerostomia without the protective properties of saliva. In addition the constant rinsing of the oesophagus by saliva and its buffering and antimicrobial properties, help to protect the oesophagus from damage by acids, and to prevent infections.
Dental and oral health
Dental health depends on saliva for many reasons including its continuous rinsing of the oral and buccal cavities to wash away particles in which microorganisms grow, its ability to buffer acids (saliva is more alkaline at high rates of flow), its specific and non-specific immune functions due to the presence of immunoglobulins, the antimicrobial constituents sialoperoxidase, thiocyanate and lysozyme, and the presence of calcium phosphate, which prevents demineralization of the teeth. As a consequence of the decreased production of saliva various oral diseases are associated with xerostomia. These are dental caries, gum disease, mucosal ulceration and atrophy, infections of the mouth (e.g. candida), and ascending infection of the salivary glands.
In addition, in the absence of saliva, retention of dentures is more difficult. Patients who have a dry mouth because they are being treated with tricyclic antidepressants, ganglion-blocking drugs, or parasympathomimetic drugs (for hypertension), may experience difficulty in oral function if they wear dentures.
• Sour: the posterior sides of the tongue
• Salt: the anterior sides
• Sweet: the front of the tongue
• Bitter: the rear of the tongue.
There are however, no obvious structural differences in taste buds in the different regions. The differences in sensitivity are partly due to precise projections of the afferent nerves to the central nervous system and partly to the patterns of impulses from a population of chemoreceptors. The nerves from the taste buds in the anterior of the tongue pass in the chorda tympani (a branch of the facial nerve) and those from the taste buds in the posterior third travel in the glossopharyngeal nerve. These nerves project to the tractus solitarius (Fig. 2.8). The sensory nerves from the taste buds in the palate and epiglottis ascend in the vagus nerve. The possible pathological sequelae following damage to some of the nerves during oral surgery are discussed in Box 5.
 |
| Fig. 2.8 |
Case 2.2
Consequences for the functioning of the mouth
Chewing, swallowing and speech
Chewing depends on activation of periodontal receptors that results in impulses in sensory nerve fibres in the inferior dental nerve being transmitted to the chewing centre. However, in practice, chewing is not usually much impaired following such nerve damage. The tongue, which is innervated by the lingual nerve, moves the food around in the mouth to aid chewing. Therefore if the tongue is partially denervated the process of mastication could be impaired, but this is not usually a serious problem.
The swallowing reflex is initiated when the tongue moves the food bolus to the back of the mouth where it activates pressure receptors in the pharynx. However, swallowing is usually not seriously affected after such nerve damage, because only a small part of the musculature is likely to be affected.
Articulation of many sounds depends on fine control of the movements of the muscles of the tongue. These reflexes partly depend on tactile information from the tongue, but in practice, unilateral damage to these nerves, accompanying wisdom tooth extraction, does not affect speech to any significant extent.
Taste
Some nerve fibres in the lingual nerve carry sensory information from the taste buds on the tongue (via the chorda tympani). Loss of some taste sensation on one side of the tongue could occur in the patient but it is not usually a serious problem.
Salivary secretion
The patient is unlikely to suffer from a dry mouth because between meals the mouth is kept moist by saliva from the smaller glands in the oral and buccal mucosa. When food is eaten or at the approach of food over half of the increased flow comes from the parotid glands. The lingual nerve innervates the submandibular and sublingual salivary glands but not the parotids (Fig. 2.5). The latter are innervated by fibres in the glossopharyngeal nerve. Thus interference with the flow of saliva is not a serious problem after unilateral lingual nerve damage accompanying a wisdom tooth extraction.
Loss of pain sensation
The numbness experienced by this patient due to the damaged lingual nerve could be a serious problem because the patient could injure his tongue by biting it without realizing it. He may also burn the tongue and other tissues in his mouth by drinking liquid that is too hot. The patient’s lower lip was also numb, because of this structure is innervated by the inferior dental nerve. Thus injury could also occur due to accidental biting or scalding of the lip. Fortunately for this patient, sensation in the affected areas would probably return over the subsequent few weeks.
The dissolved chemicals in the saliva diffuse into the taste pore from the fluid layer on the tongue. Appropriate chemicals, such as NaCl, are detected by receptor molecules on the taste hairs, and this results in a depolarization of the cell membrane (receptor potential) of the taste bud cell which causes the release of an excitatory transmitter that evokes a generator potential in the sensory nerve endings (see the companion volume The Nervous System). The mechanism of the response to salt (NaCl) has been well studied (Fig. 2.9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree