Chapter 21 The liver in pregnancy
TABLE 21.1 Changes in liver biochemical test levels in normal pregnancy
| Test | Change | Trimester of maximum change |
|---|---|---|
| Albumin | ↓ 10%–60% | Second |
| Gamma globulins | None to slight ↓ | Third |
| Fibrinogen | ↓ 50% | Second |
| Transferrin | ↓ | Third |
| Bilirubin | None | — |
| Alkaline phosphatase | ↓ Two- to fourfold | Third |
| AST | None | — |
| ALT | None | — |
| Cholesterol | ↓ Twofold | Third |
↓, increase; ↓, decrease; ALT, alanine aminotransferase; AST, aspartate aminotransferase.
From Olans LB, Wolf JL. Liver disease in pregnancy. In: Carlson KJ, Eisenstat SA, eds. The Primary Care of Women, 2nd edn. St. Louis: Mosby–Year Book; 2003:531–539.
Overview
Approach to the Pregnant Patient
History
 Headache, peripheral edema, foamy urine, oliguria, and neurologic symptoms may occur in pre-eclampsia
Headache, peripheral edema, foamy urine, oliguria, and neurologic symptoms may occur in pre-eclampsiaTABLE 21.2 Differential diagnosis of elevated serum aminotransferase levels and/or jaundice according to trimester of pregnancy
| Trimester | Differential diagnosis |
|---|---|
| First | Hyperemesis gravidarum |
| Gallstones | |
| Viral hepatitis | |
| Drug-induced hepatitis | |
| Intrahepatic cholestasis of pregnancy∗ | |
| Second | Intrahepatic cholestasis of pregnancy |
| Gallstones | |
| Viral hepatitis | |
| Drug-induced hepatitis | |
| Pre-eclampsia/eclampsia∗ | |
| HELLP syndrome∗ | |
| Third | Intrahepatic cholestasis of pregnancy |
| Pre-eclampsia/eclampsia | |
| HELLP syndrome | |
| Acute fatty liver of pregnancy | |
HELLP, hemolysis, elevated liver tests, low platelets.
From Olans LB, Wolf J. Liver disease in pregnancy. In: Carlson KJ, Eisenstat SA, eds. The Primary Care of Women, 2nd edn. St. Louis: Mosby–Year Book; 2003:531–539.
TABLE 21.3 Rates of recurrence of pregnancy-associated liver disease in subsequent pregnancies
| Disease | Rate of recurrence |
|---|---|
| Intrahepatic cholestasis of pregnancy | 40%–70% |
| HELLP syndrome | 4%–27% |
| Acute fatty liver of pregnancy | 20%–70% in carriers of LCHAD mutation |
| Pre-eclampsia | 2%–43% |
HELLP, hemolysis, elevated liver tests, low platelets; LCHAD, long-chain 3-hydroxyacyl-coenzyme A dehydrogenase.
Physical examination
 Abnormal findings that occur with liver disease in pregnancy are jaundice, hepatomegaly, hepatic tenderness, friction rub or bruit, splenomegaly, Murphy’s sign, and diffuse excoriations
Abnormal findings that occur with liver disease in pregnancy are jaundice, hepatomegaly, hepatic tenderness, friction rub or bruit, splenomegaly, Murphy’s sign, and diffuse excoriationsDiagnostic tests
 The only major restrictions compared with the nongravid state are radiation and gadolinium exposures
The only major restrictions compared with the nongravid state are radiation and gadolinium exposures Routine blood chemistry tests and a blood count are helpful. Uric acid levels are often elevated in AFLP and may be elevated in pre-eclampsia
Routine blood chemistry tests and a blood count are helpful. Uric acid levels are often elevated in AFLP and may be elevated in pre-eclampsia Hemolysis and a low platelet count occur in HELLP syndrome. Disseminated intravascular coagulation (DIC) with a low fibrinogen level, increased fibrin split products, and an elevated partial thromboplastin time may also occur in HELLP syndrome
Hemolysis and a low platelet count occur in HELLP syndrome. Disseminated intravascular coagulation (DIC) with a low fibrinogen level, increased fibrin split products, and an elevated partial thromboplastin time may also occur in HELLP syndrome If viral hepatitis is suspected, serologic tests should be checked for the following: hepatitis A (immunoglobulin M [IgM] and IgG antibody to hepatitis A virus [anti-HAV]); hepatitis B (surface antigen [HBsAg] and antibody, core antibody, and, if HBsAg is positive, e antigen and antibody); hepatitis C (antibody to hepatitis C virus [anti-HCV] and possibly HCV RNA). If the patient has traveled to an endemic area, consider testing for hepatitis E (see Chapter 3)
If viral hepatitis is suspected, serologic tests should be checked for the following: hepatitis A (immunoglobulin M [IgM] and IgG antibody to hepatitis A virus [anti-HAV]); hepatitis B (surface antigen [HBsAg] and antibody, core antibody, and, if HBsAg is positive, e antigen and antibody); hepatitis C (antibody to hepatitis C virus [anti-HCV] and possibly HCV RNA). If the patient has traveled to an endemic area, consider testing for hepatitis E (see Chapter 3) The benefits of endoscopy, including endoscopic retrograde cholangiopancreatography (ERCP), should be weighed against the risks in pregnancy. Risks include fetal hypoxia from sedative drugs or positioning. Sedative medications and radiation exposure should be minimized
The benefits of endoscopy, including endoscopic retrograde cholangiopancreatography (ERCP), should be weighed against the risks in pregnancy. Risks include fetal hypoxia from sedative drugs or positioning. Sedative medications and radiation exposure should be minimized Although abdominal computed tomography (CT) is more sensitive than abdominal ultrasonography for hepatic rupture and may yield more information, radiation exposure and the stability of the patient should be considered in decisions about the choice of imaging test
Although abdominal computed tomography (CT) is more sensitive than abdominal ultrasonography for hepatic rupture and may yield more information, radiation exposure and the stability of the patient should be considered in decisions about the choice of imaging testLiver Disorders Unique to Pregnancy
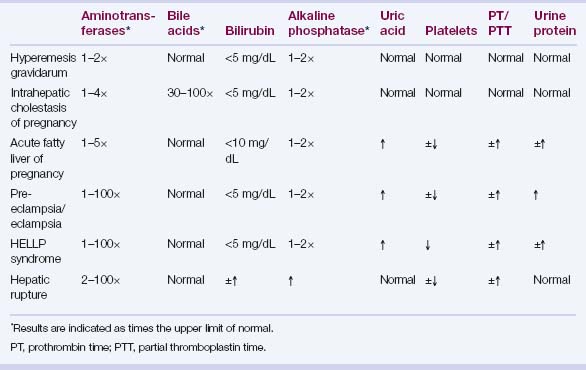
See Table 21.4 for the laboratory findings associated with these disorders.
Hyperemesis gravidarum
 Serum alanine aminotransferase (ALT) elevations generally 1- to 3-fold but may reach 20 times the upper limit of normal
Serum alanine aminotransferase (ALT) elevations generally 1- to 3-fold but may reach 20 times the upper limit of normalIntrahepatic cholestasis of pregnancy
 Incidence: 0.01% to 2%, with higher incidence in South Asian, South American, and Scandinavian populations; highest incidence (up to 27%) in Chilean Araucanian Indians
Incidence: 0.01% to 2%, with higher incidence in South Asian, South American, and Scandinavian populations; highest incidence (up to 27%) in Chilean Araucanian Indians Gene variants of hepatocanalicular transport proteins (ATP-binding cassette [ABC] transporter B4 = phosphatidylcholine floppase, ABC transporter B11 = bile salt export pump, ABC transporter C2 = conjugated organic anion transporter, ATP8B1 = FIC1) and their regulators (e.g., the bile acid sensor farnesoid X receptor, FXR) found in some patients; incidence of IHCP increased in mothers of children with progressive familial intrahepatic cholestasis (PFIC) type 3
Gene variants of hepatocanalicular transport proteins (ATP-binding cassette [ABC] transporter B4 = phosphatidylcholine floppase, ABC transporter B11 = bile salt export pump, ABC transporter C2 = conjugated organic anion transporter, ATP8B1 = FIC1) and their regulators (e.g., the bile acid sensor farnesoid X receptor, FXR) found in some patients; incidence of IHCP increased in mothers of children with progressive familial intrahepatic cholestasis (PFIC) type 3 Elevated serum aminotransferase levels (up to four-fold), serum bile acid levels (30–100x), mono- or disulfated progesterone metabolites (particularly 3- and 5-alpha isomers), and occasionally serum cholesterol and triglyceride levels
Elevated serum aminotransferase levels (up to four-fold), serum bile acid levels (30–100x), mono- or disulfated progesterone metabolites (particularly 3- and 5-alpha isomers), and occasionally serum cholesterol and triglyceride levels