The specific entities in Table 3.1 are discussed in detail in the relevant chapters of this book, but this table provides a useful compilation of subtle biopsy diagnoses to consider when the biopsy looks almost normal. The next section of this chapter is devoted to highlighting some of the entities that do not fit well anywhere else in this book. Cryptogenic cirrhosis is considered in a separate section of this chapter. The last section discusses the differential in the almost normal, nonfibrotic liver when all of these other potential causes discussed in this chapter have been carefully excluded.
SINUSOIDAL CHANGES
The “Resolving Hepatitis Pattern”
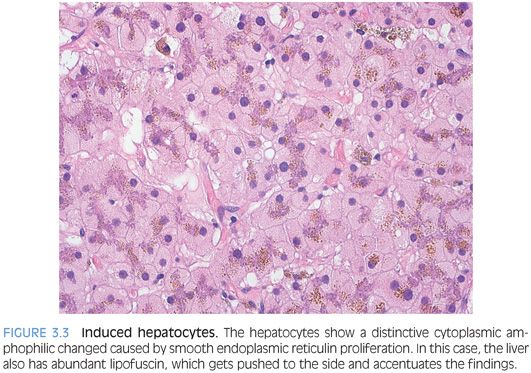
This pattern of injury is most commonly seen with acute idiosyncratic drug effects, where the agent was removed some weeks (by the patient, family physician, etc.) prior to seeing a hepatologist and having a liver biopsy. Acute self-limited viral hepatitis can also have the same findings. The biopsy shows minimal or no inflammation, while the lobules have scattered small clusters of pigmented macrophages, which represent the “cleanup” efforts in a site of prior liver injury (Fig. 3.1).
Hyperviscosity Syndromes
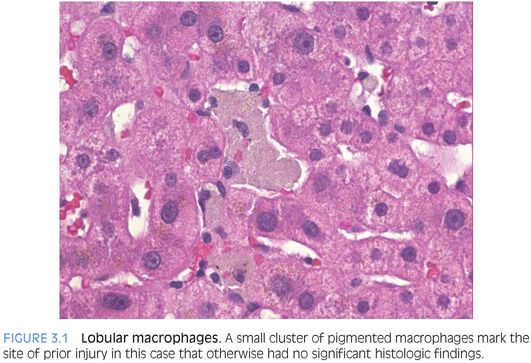
The liver biopsy findings in hyperviscosity syndromes have not been well described in the literature. The hyperviscosity syndrome can be seen in a wide variety of conditions, including multiple myeloma, Waldenström macroglobulinemia, and polycythemia vera. Autoimmune disease, such as Sjögren syndrome, systemic lupus erythematosus, or rheumatoid arthritis, can also be associated with the hyperviscosity syndrome. The histologic findings can be subtle, with little or no inflammation, and the histologic changes dominated by varying degrees of sinusoidal dilatation and congestion. In some cases, there can also be marked lobular disarray and nuclear pleomorphism, presumably due to chronic low-grade ischemia (Fig. 3.2).
Sinusoidal Dilatation
Sinusoidal dilatation and congestion can be an important clue to vascular outflow abnormalities. Sinusoidal dilatation has a zone 3 distribution and is often accompanied by Kupffer cell iron deposition when long-standing. There may be zone 3 or central vein fibrosis in chronic cases, but many times, fibrosis will not be evident. Other causes of sinusoidal dilatation include drug effect, and this pattern of injury is discussed in Chapter 13 on vascular disease. However, there are many cases in which the sinusoidal dilatation is subtle but truly seems to be present, and there is no clinical or imaging evidence for vascular outflow disease and no relevant medication history. In these cases, the differential includes systemic inflammatory diseases, infectious granulomatous diseases, autoimmune diseases, and paraneoplastic effects from carcinomas in other organs.1,2 Autoimmune conditions that can be associated with a mild sinusoidal dilatation include the antiphospholipid syndrome3 and rheumatoid arthritis.4 As a caveat, subtle sinusoidal dilatation can also be seen with rapid blood volume expansion and a wide variety of other conditions. In fact, very mild sinusoidal congestion is often without any diagnostic value and is sometimes overinterpreted. Any hepatocyte atrophy that accompanies the congestive changes increases confidence that the findings are real. The atrophy can be highlighted with a reticulin stain and this can be helpful in many cases. For cases without atrophy, the congestion or sinusoidal dilatation has to be reasonably more than seen in most biopsies to be clinically meaningful and takes some experience to comfortably recognize.
HEPATOCYTE CHANGES
There are a variety of very mild hepatocyte changes that can be associated with elevated liver enzymes. One important pattern is that of glycogen accumulation, which can range from mild to marked. The clinical and histologic findings of glycogen accumulation are discussed in more detail in Chapters 8 and 9.
Prominent Megamitochondria
Megamitochondria are commonly seen with fatty liver disease and with cholestatic liver disease. However, this section discusses cases that lack any significant fat or cholestatic changes and the main finding is that of prominent hepatocyte megamitochondria. Overall, this finding is nonspecific and only rarely seen as an isolated finding. In adults, it can be associated with drug effects, although typically, there will also be other findings of a drug reaction.5 In children, it can be associated with the earliest changes of inherited mitochondrial defects, with various defects of the urea cycle, or with other inherited metabolic defects such as lysinuric protein intolerance and hypermethioninemia.6
Pseudoground Glass Change in Cytoplasm
Pseudoground glass change is discussed in detail in Chapter 8. In many cases, the changes are striking and rather diffuse and thus easy to identify, but in some cases, they can be focal and more subtle. The main finding is that of large amphophilic inclusions in the hepatocytes in individuals who have a chronic illness or are immunosuppressed and are on many medications.
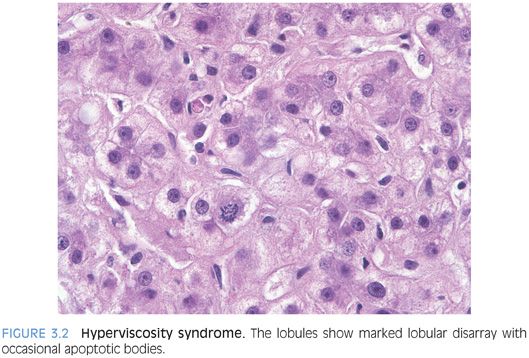
Induced Endoplasmic Reticulin Proliferation
This change is manifested by hepatocytes that have a distinctly amphophilic change to their cytoplasm (Fig. 3.3). The change does not lead to well-defined inclusions, in contrast to those seen in glycogen pseudoground glass, but also represents a drug effect. The hepatocyte cytoplasm in many cases is distinctly “two-toned” because the cytoplasm will be divided into two separate and distinctive colors. This change can be seen with a number of different medications.